- AKTUALNOŚCI
- NARODOWY POZP 2017-2022
- MODEL ORGANIZACYJNY ŚWIAT
- MODEL ORGANIZACYJNY DB
- KONTAKT
-
ARCHIWUM
-
PODKARPACKI POZP 2017-2022
>
- Aktualności do 2020
- Forum PK 2017-2018
- KONGRES ZP 2017 Sesja ZP DZIECI
- Forum PK 2016 Dzieci i Młodzież
-
NPOZP 2015 kalendarium
>
- 2015 V-IX wystąpienia
- 20150527 Apel Porozumienia na Rzecz NPOZP
- 20150729 Komunikat prasowy
- 20150801 Ekspertyza prof. Jacka Wciórki
- 20150804 Wystąpienie do Marszałka Sejmu
- 20150806 Interpelacja Posła Józefa Lasoty
- 20150813 List otwarty
- 20150820 Wspólne stanowisko
- 20150821 Ekspertyza Regina Bisikiewicz
- 20150821 Ekspertyza - załącznik RB
- 20150903 Apel Porozumienia na Rzecz NPOZP
- 20150911 Oświadczenie po głosowaniu
- 20150922 Opinia o Raporcie za 2014
- Forum PK 2014 XII Rzeszow
- Forum PK 2014 V Stalowa Wola >
- RPO 2014 Raport streszczenie
- Forum PK 2013
- Interwencja 2013 redukcja łóżek w Rzeszowie
- Konferencja PK 2012 ZP DZIECI
- PkPOZP 2012-2016
- NPOZP 2007-2015 >
-
PODKARPACKI POZP 2017-2022
>
-
EKONOMIKA ZDROWIA PSYCHICZNEGO
- EZP01 Teoria ekonomiczna w zarysie
- EZP02 Rys historyczny systemu KCh iNFZ
- EZP08 Rachunek kosztów działań ABC
- EZP03 Jakość i efektywność
- EZP12 Program pilotażowy - wytyczne i ocena
- EZP05 Opieka koordynowana
- EZP06 Opieka stopniowalna
- EZP04 JGP
- EZP07 Zarządzanie populacyjne
- EZP09 Wielka Brytania commissioning & payment
- EZP10 USA utilizatian & payment
- EZP11 Niemcy cost-effectiveness
- EZP13 Włochy
- EZP14
- EZP15
- EZP16
- Standardy Holandia
- Standardy Australia
- Standardy Niemcy
- Standardy Włochy
- Standardy Anglia
- UK OPIEKA ŚRODOWISKOWA
- UK OPIEKA STACJONARNA
- UK STANDARDY NICE
- Debata medialna o pilotażu CZP
THE INITIAL PSYCHIATRIC INTERVIEW
Robert Waldinger M.D.
Alan M. Jacobson M.D.
WSTĘPNY WYWIAD PSYCHIATRYCZNY (tłumaczenie Google)
Robert Waldinger
Alan M.Jacobson
1 .Jakie są główne cele pierwszego wywiadu psychiatrycznego?
Postawienie wstępnej diagnostyki różnicowej i sformułowanie planu leczenia. Cele te osiąga się poprzez:
Zbieranie informacji:
■ Dojście do empatycznego zrozumienia, jak czuje się pacjent. To zrozumienie jest podstawą do nawiązania relacji z pacjentem.
Kiedy klinicysta uważnie słucha, a następnie wyraża uznanie dla zmartwień i trosk pacjenta, pacjent zyskuje poczucie, że jest rozumiany. To poczucie bycia zrozumianym jest podstawą całego późniejszego leczenia i pozwala klinicyście zainicjować związekw którym można zawrzeć sojusz na rzecz leczenia.
2. To dużo, na czym należy się skupić podczas pierwszego spotkania. A pomoc pacjentowi?
Wstępna diagnoza i plan leczenia mogą być szczątkowe. Rzeczywiście, gdy pacjenci są w kryzysie, historia może być niejasna, niekompletna lub zawężona. W rezultacie niektóre interwencje są podejmowane nawet wtedy, gdy zbierane są podstawowe informacje o
historii, relacjach rodzinnych i obecnych stresorach. Bardzo ważne jest, aby pamiętać, że trudności emocjonalne często powodują izolację. Doświadczenie dzielenia się swoim problemem
z zatroskanym słuchaczem może samo w sobie przynieść ogromną ulgę. Tak więc wstępny wywiad jest początkiem leczenia jeszcze przed ustaleniem formalnego planu leczenia.
3. Jak powinna być zorganizowana rozmowa wstępna?
Nie ma jednego ideału, ale warto pomyśleć o wstępnej rozmowie zgłoszeniowej jako składającej się z trzech elementów:
Nawiąż wstępny kontakt z pacjentem i zapytaj o zgłaszaną skargę lub problemy, czyli o to, co sprowadziło pacjenta na pierwsze spotkanie. Niektórzy pacjenci opowiadają swoje historie bez większych wskazówek ze strony klinicysty, podczas gdy inni wymagają wyraźnych instrukcji w formie konkretnych pytań, które pomogą im uporządkować myśli. Podczas tej fazy pierwszego wywiadu pacjent powinien mieć jak najwięcej możliwości podążania za własnymi schematami myślowymi.
Uzyskaj określone informacje, w tym historię prezentowanych problemów, istotne informacje medyczne, pochodzenie rodzinne, historię społeczną oraz określone objawy i wzorce zachowań. Formalnie przetestuj stan psychiczny (patrz ten rozdział).
Zapytaj, czy pacjent ma jakieś pytania lub o których nie wspomniał obawy. Następnie pacjent otrzymuje wstępne zalecenia dotyczące dalszej oceny i/lub rozpoczęcia leczenia.
Chociaż te trzy części wywiadu można rozpatrywać oddzielnie, często przeplatają się one ze sobą, np. obserwacje stanu psychicznego można prowadzić od momentu spotkania klinicysty z pacjentem.
Stosowny wywiad medyczny i rodzinny może zostać przywołany w trakcie przedstawiania innych obaw, a pacjenci mogą zadawać ważne pytania dotyczące zaleceń dotyczących leczenia, gdy przedstawiają swój początkowy wywiad.
4. Czy wstępna ocena różni siew przypadku złożonych sytuacji?
Wstępna ocena psychiatryczna może wymagać więcej niż jednej sesji w złożonych sytuacjach - na przykład podczas oceny dzieci lub rodzin lub oceny przydatności pacjenta do określonego podejścia terapeutycznego, takiego jak krótka psychoterapia. Wstępna ocena może również wymagać zebrania informacji z innych źródeł: rodziców, dzieci, współmałżonka, najlepszego przyjaciela, nauczyciela, funkcjonariuszy policji i/lub innych pracowników służby zdrowia. Kontakty te mogą zostać włączone do pierwszej wizyty lub mogą wystąpić później. Pierwszym krokiem w dokonywaniu takich usta leń jest wyjaśnienie pacjentowi powodu ich zawarcia oraz uzyskanie wyraźnej, pisemnej zgody na kontakt.
5. Jak należy podejść do źródła skierowań?
Prawie zawsze właściwe jest skontaktowanie się ze źródłem skierowania w celu zebrania informacji i wyjaśnienia wstępnych wrażeń diagnostycznych i planów leczenia. Wyjątki mogą wystąpić, gdy skierowanie pochodzi od innych pacjentów, przyjaciół lub innych osób niebędących profesjonalistami, których pacjent chce wykluczyć z leczenia.
6. Czy istnieją jakieś odmiany tych wytycznych dla wstępnej oceny?
Konkretne orientacje teoretyczne mogą dyktować istotne różnice w wstępnej ocenie. Na przykład terapeuta behawioralny kieruje dyskusję do konkretnych analiz bieżących problemów i poświęca niewiele czasu na doświadczenia z wczesnego dzieciństwa. Ocena psychofarmakologiczna kładzie nacisk na specyficzne wzorce objawów, reakcje na wcześniejsze leczenie farmakologiczne oraz występowanie chorób psychicznych w rodzinie. Podejście przedstawione w tym rozdziale jest zestawem zasad o szerokim zastosowaniu, które można zastosować w ocenie większości pacjentów.
7. W jaki sposób zbierane są informacje z wywiadu?
Klinicysta musi dowiedzieć się jak najwięcej o tym, jak pacjent myśli i czuje. Podczas wywiadu klinicznego zbierane są informacje z tego, co pacjent mówi klinicyście; krytycznie ważne wskazówki pochodzą również z tego, jak rozwija się historia. Zatem zarówno treść wywiadu (tj. to, co mówi pacjent), jak i przebieg wywiadu (tj. sposób, w jaki pacjent to mówi) oferują ważne drogi do zrozumienia problemów pacjenta. Weź pod uwagę kolejność przekazywanych informacji, komfort mówienia o nich, emocje związane z dyskusją, reakcje pacjenta na pytania i wstępne uwagi, spójność prezentacji oraz czas podania informacji. Pełne opracowanie takich informacji może zająć jedną lub kilka sesji w ciągu dni, tygodni lub miesięcy, ale podczas pierwszego wywiadu można zasugerować głębsze obawy.
Na przykład 35-letnia kobieta zgłosiła zaniepokojenie nawracającą astmą jej syna i związanymi z tym trudnościami w szkole. Swobodnie mówiła o swoich obawach i zasięgała rady, jak pomóc synowi. Zapytana o myśli męża, na chwilę się uspokoiła. Następnie powiedziała, że podziela jej obawy i przeniosła dyskusję z powrotem na jej syna. Jej wahanie wskazywało na inne problemy, które pozostały nierozwiązane podczas pierwszej sesji. Rzeczywiście, zaczęła kolejną sesję od pytania: „Czy mogę mówić o czymś innym niż o moim synu?". Uspokoiwszy się, opisała chroniczną złość męża na syna z powodu jego „słabości". Jego złość i jej własne uczucia w odpowiedzi stały się ważnym celem późniejszego leczenia.
8. Jak należy rozpocząć rozmowę zgłoszeniową?
Tu i teraz jest miejscem, w którym zaczyna się wszystkie wywiady. Można zadać jedno z wielu prostych pytań: „Co cię dzisiaj do mnie sprowadza? Możesz mi powiedzieć, co cię trapi?Jak
Czy to dlatego, że zdecydowałeś się umówić na to spotkanie? W przypadku niespokojnych pacjentów przydatna jest struktura: wczesne zapytanie o wiek, stan cywilny i sytuację życiową może dać im czas na stanie się czują się komfortowo, zanim przystąpią do opisu swoich problemów. Jeśli lęk jest ewidentny, prosty komentarz na temat lęku może pomóc pacjentom porozmawiać o swoich zmartwieniach.
9. Czy wysoce ustrukturyzowany format jest ważny?
Nie. Pacjenci muszą mieć możliwość uporządkowania swoich informacji w sposób, który im najbardziej odpowiada. Klinicysta, który przedwcześnie poddaje pacjenta strumieniowi konkretnych pytań, ogranicza informacje o własnym procesie myślowym pacjenta, nie uczy się, jak pacjent radzi sobie z ciszą lub smutkiem, odcina mu możliwość podpowiedzi lub wprowadzenia nowych tematów.
Ponadto zadanie polegające na formułowaniu jednego konkretnego pytania po drugim może zakłócać zdolność lekarza do słuchania i rozumienia pacjenta.
Nie oznacza to, że należy unikać konkretnych pytań. Często pacjenci udzielają rozbudowanych odpowiedzi na konkretne pytania, takie jak „Kiedy byłeś żonaty?" Ich odpowiedzi mogą otworzyć nowe możliwości dochodzenia. Kluczem jest unikanie szybkiego podejścia i umożliwienie pacjentom rozwinięcia myśli.
10. Jak należy zadawać pytania?
Pytania powinny być formułowane w sposób zachęcający pacjentów do rozmowy. Pytania otwarte, które nie wskazują odpowiedzi, zwykle pozwalają ludziom rozwinąć więcej niż pytania szczegółowe lub naprowadzające. Ogólnie rzecz biorąc, pytania naprowadzające (np. „Czy czułeś się smutny, kiedy twoja dziewczyna się wyprowadziła?") mogą przeszkadzać w rozmowie, ponieważ mogą sprawiać wrażenie, że osoba przeprowadzająca wywiad oczekuje od pacjenta pewnych uczuć. Niewiodące pytania („Jak się czułeś, kiedy twoja dziewczyna się wyprowadziła?") są równie bezpośrednie i skuteczniejsze.
11. Jaki jest skuteczny sposób radzenia sobie z wahaniami pacjentów?
Kiedy pacjenci potrzebują pomocy w opracowaniu, proste stwierdzenie i/lub prośba mogą wywołać więcej informacji: „Opowiedz mi o tym więcej". Powtarzanie lub zastanawianie się nad tym, co mówią pacjenci, również zachęca ich do otwarcia się (np. „Mówiłeś o swojej dziewczynie"). Czasami komentarze, które konkretnie odzwierciedlają zrozumienie przez lekarza odczuć pacjenta w związku ze zdarzeniami, mogą pomóc pacjentowi rozwinąć temat. Takie podejście zapewnia potwierdzenie zarówno klinicyście, jak i pacjentowi, że nadają na tych samych falach. Gdy klinicysta prawidłowo zareaguje na ich odczucia, pacjenci często potwierdzają odpowiedź poprzez dalszą dyskusję. Pacjent, którego dziewczyna odeszła, może czuć się zrozumiany i swobodniej rozmawiać o stracie po komentarzu typu „Wydajesz się zniechęcony wyprowadzką swojej dziewczyny".
12. Podaj przykład, jak kompleksowe gromadzenie informacji może wskazać problem.
Starszy mężczyzna został skierowany z powodu narastającego przygnębienia. W pierwszym wywiadzie opisał najpierw trudności finansowe, a następnie poruszył niedawny rozwój problemów medycznych, których kulminacją była diagnoza raka prostaty. Kiedy zaczął mówić o raku i chęci poddania się, zamilkł. W tym momencie wywiadu klinicysta wyraził uznanie, że pacjent wydawał się być przytłoczony narastającymi problemami finansowymi i, w większości, wszystko, medyczne zmiany. Pacjent cicho skinął głową, a następnie rozwinął swoje szczególne obawy dotyczące tego, jak jego żona będzie sobie radzić po jego śmierci. Nie czuł, że jego dzieci będą jej pomocne. Nie było jeszcze jasne, czyjego pesymizm odzwierciedlał depresyjną nadmierną reakcję na diagnozę raka, czy też dokładną ocenę rokowania. Dalsza ocena objawów i stanu psychicznego oraz krótka rozmowa z żoną w dalszej części spotkania wykazały, że rokowania są całkiem dobre. Następnie leczenie koncentrowało się na jego depresyjnych reakcjach na diagnozę.
13. Jak najlepiej formułować pytania?
Klinicysta powinien używać języka, który nie jest techniczny ani nadmiernie intelektualny. Jeśli to możliwe, należy używać własnych słów pacjenta. Jest to szczególnie ważne w przypadku spraw intymnych, takich jak problemy seksualne. Ludzie opisują swoje doświadczenia seksualne w dość zróżnicowanym języku. Jeśli pacjent mówi, że jest gejem, użyj dokładnie tego terminu, a nie pozornie równoważnego terminu, takiego jak homoseksualista. Ludzie używają niektórych słów, a innych nie, ze względu na specyficzne konotacje, jakie niosą dla nich różne słowa; na początku takie rozróżnienia mogą nie być oczywiste dla klinicysty.
14. A co z pacjentami, którzy nie są wstanie porozumiewać się w spójny sposób?
Klinicysta musi przez cały czas być świadomy tego, co dzieje się podczas wywiadu. Jeśli pacjent ma halucynacje lub jest bardzo zdenerwowany, nieuznanie zdenerwowania lub niepokojącego doświadczenia może zwiększyć niepokój pacjenta.
Omówienie aktualnego zdenerwowania pacjenta pomaga złagodzić napięcie i mówi pacjentowi, że lekarz słucha. Jeśli historia pacjenta jest chaotyczna lub niejasna, uznaj trudności w zrozumieniu pacjenta i oceń możliwe przyczyny (np. psychoza z poluzowanymi skojarzeniami vs. lęk przed wizytą).
Kiedy pytania ogólne (np. „Opowiedz mi coś o swoim pochodzeniu") są nieskuteczne, może być konieczne zadawanie szczegółowych pytań dotyczących rodziców, szkoły i dat wydarzeń. Pamiętaj jednak, że zadawanie niekończących się pytań w celu złagodzenia własnego niepokoju, a nie pacjenta, może być kuszące.
15. Podsumuj kluczowe punkty, o których należy pamiętać podczas pierwszego wywiadu.
Umożliwienie pacjentowi swobodnego opowiedzenia własnej historii musi być zrównoważone poprzez uwzględnienie zdolności pacjenta do skupienia się na istotnych tematach. Niektóre osoby wymagają wskazówek od klinicysty, aby uniknąć zagubienia się w stycznych tematach. Inni mogą potrzebować spójnej struktury, ponieważ mają problemy z uporządkowaniem myśli, być może z powodu wysokiego stopnia niepokoju. Empatyczny komentarz na temat niepokoju pacjenta może go zmniejszyć, a tym samym doprowadzić do wyraźniejszej komunikacji.
Niektóre wytyczne dotyczące rozmowy zgłoszeniowej
• Pozwól, aby pierwsza część wstępnego wywiadu podążała za tokiem myślenia pacjenta.
• Zapewnij strukturę, aby pomóc pacjentom, którzy mają problemy z uporządkowaniem myśli lub dokończeniem uzyskiwania określonych danych.
• Formułuj pytania, aby zachęcić pacjenta do rozmowy (np. pytania otwarte, nienaprowadzające).
• Używaj słów pacjenta.
• Bądź wyczulony na wczesne oznaki utraty kontroli nad zachowaniem (np. wstawanie do tempa).
• Zidentyfikuj mocne strony pacjenta oraz obszary problemowe.
• Unikaj żargonu i technicznego języka.
• Unikaj pytań zaczynających się od „dlaczego".
• Unikaj przedwczesnych zapewnień.
• Nie pozwalaj pacjentom zachowywać się niewłaściwie (np. łamać lub rzucać przedmiotami).
• postaw granice wobec wszelkich zagrażających zachowań i w razie potrzeby wezwij niezbędną pomoc.
16. Jakich konkretnych pułapek należy unikać podczas wstępna rozmowa zgłoszeniowa?
Unikaj żargonu lub terminów technicznych, chyba że jest to jasno wyjaśnione i konieczne. Pacjenci mogą używać żargonu, na przykład: „Miałem paranoję". Jeśli pacjent używa słowa technicznego, zapytaj o jego znaczenie. Możesz być zaskoczony zrozumieniem pacjenta. Na przykład pacjenci mogą używać słowa „paranoik", aby zasugerować strach przed dezaprobatą społeczną lub pesymizm co do przyszłości. Uważaj również, aby podczas wywiadu przypisać problemom pacjenta etykietę diagnostyczną. Pacjent może być przestraszony i zdezorientowany etykietą.
Ogólnie rzecz biorąc, unikaj zadawania pytań zaczynających się od „dlaczego". Pacjenci mogą nie wiedzieć, dlaczego mają określone doświadczenia lub uczucia i mogą czuć się nieswojo, a nawet głupio, jeśli uważają, że ich odpowiedzi nie są „dobre". Pytanie dlaczego oznacza również, że oczekujesz od pacjenta szybkich wyjaśnień.
Pacjenci dowiadują się więcej o źródłach swoich problemów, zastanawiając się nad swoim życiem podczas wywiadu i kolejnych sesji. Kiedy masz ochotę zapytać dlaczego, sformułuj pytanie tak, aby wywołało bardziej szczegółową odpowiedź.
Alternatywy obejmują „Co się stało?" „Jak to się stało?" lub „Co o tym myślisz?'
Unikaj przedwczesnej pewności siebie. Kiedy pacjenci są zdenerwowani, jak to często bywa podczas pierwszych wywiadów, osoba przeprowadzająca wywiad może ulec pokusie, by rozwiać obawy pacjenta, mówiąc: „Wszystko będzie dobrze" lub „Nie ma tu nic naprawdę złego".
Jednak zapewnienie jest prawdziwe tylko wtedy, gdy klinicysta (1) dokładnie zbadał charakter i zakres problemów pacjenta oraz (2) jest pewien tego, co mówi pacjentowi. Przedwczesne zapewnienie może zwiększyć niepokój pacjenta, sprawiając wrażenie, że lekarz wyciągnął pochopne wnioski bez dokładnej oceny lub po prostu mówi to, co pacjent chce usłyszeć. Pozostawia również pacjentów samych ze swoimi obawami oto, co naprawdę jest nie tak.
Co więcej, przedwczesne zapewnienia raczej zamykają dyskusję niż zachęcają do dalszych badań problem. Bardziej uspokajające może być zapytanie pacjenta, co go niepokoi. Proces (tj. charakter interakcji) pociesza pacjenta bardziej niż jakakolwiek pojedyncza rzecz, którą może powiedzieć klinicysta.
Postaw granice zachowaniom.
Z powodu problemów psychiatrycznych niektórzy pacjenci mogą stracić kontrolę nad sesją. Chociaż opisane tutaj podejście kładzie nacisk na pozwolenie pacjentowi na kierowanie dużą częścią werbalnej dyskusji, czasami należy wyznaczyć granice niewłaściwego zachowania. Pacjenci, którzy są podnieceni i chcą się rozebrać lub grożą, że rzucą przedmiotem, muszą być kontrolowani.
Cel ten najczęściej osiąga się poprzez komentowanie narastającego pobudzenia, omawianie go, dopytywanie o źródła niepokoju i informowanie pacjentów o granicach akceptowalnego zachowania. W rzadkich przypadkach pomoc z zewnątrz może być konieczna (np. ochroniarze na oddziale ratunkowym), zwłaszcza jeśli zachowanie się nasila, a przesłuchujący wyczuwa niebezpieczeństwo. Wywiad należy przerwać do czasu, gdy zachowanie pacjenta będzie można opanować w taki sposób, aby można było bezpiecznie kontynuować.
17. O czym często zapomina się w ocenie pacjentów?
Nowy pacjent nawiązuje kontakt z klinicystą z powodu problemów i zmartwień; to są uzasadnione pierwsze tematy wywiadu. Pomocne jest również zrozumienie mocnych stron pacjenta, które są podstawą, na której będzie opierać się leczenie. Mocne strony obejmują sposoby, w jakie pacjent z powodzeniem radził sobie z przeszłym i obecnym cierpieniem, osiągnięciami, źródłami wewnętrznej wartości, przyjaźniami, osiągnięciami w pracy i wsparciem rodziny. Mocne strony obejmują również hobby i zainteresowania, które pacjenci wykorzystują do walki ze swoimi zmartwieniami.
Pytania typu „Z czego jesteś dumny?" lub „Co lubisz w sobie?" może ujawnić takie informacje.
Często informacje wychodzą po namyśle w trakcie rozmowy. Na przykład jeden pacjent był bardzo dumny ze swojej wolontariatu w kościele. Wspomniał o tym tylko mimochodem, omawiając swoje zajęcia na tydzień przed spotkaniem. Jednak ta praca wolontariacka była jego jedynym aktualnym źródłem osobistej wartości. Zwrócił się do niego, gdy zdenerwował się brakiem sukcesów w karierze.
18. Jaka jest rola humoru w wywiadzie?
Pacjenci mogą używać humoru, aby odwrócić rozmowę od tematów wywołujących lęk lub niepokojących. Czasami przydatne może być zezwolenie na takie odchylenia, aby pomóc pacjentom zachować równowagę emocjonalną. Jednak zbadaj dalej, czy humor wydaje się prowadzić do radykalnej zmiany tematu, który wydawał się ważny i / lub emocjonalnie istotny. Humor może również skierować klinicysta w kierunku nowych obszarów do zbadania.
Lekki żart pacjenta (np. o seksie) może być pierwszym krokiem do wprowadzenia tematu, który później nabiera znaczenia.
Ze strony klinicysty humor może mieć charakter ochronny i obronny. Tak jak pacjent może odczuwać niepokój lub dyskomfort, tak samo może czuć się osoba przeprowadzająca wywiad. Uważaj, bo humor może przynieść odwrotny skutek. Może to zostać odebrane jako kpina. Może również pozwolić zarówno pacjentowi, jak i klinicyście uniknąć ważnych tematów. Czasami humor jest wspaniałym sposobem na pokazanie ludzkich cech rozmówcy i tym samym zbudowanie terapeutycznego sojuszu. Mimo wszystko pamiętaj o problematycznych aspektach humoru, zwłaszcza gdy ty i twój pacjent nie znacie się dobrze.
19. Jak ocenia się zamiary samobójcze?
Ze względu na częstość występowania zaburzeń depresyjnych i ich związek z samobójstwem, podczas pierwszego wywiadu zawsze należy uwzględnić możliwość wystąpienia intencji samobójczych. Pytanie o samobójstwo nie sprowokuje do aktu. Jeśli temat nie pojawia się spontanicznie, można użyć kilku pytań, aby wydobyć myśli pacjenta na temat samobójstwa (wymienione w kolejności, w jakiej można je wykorzystać do rozpoczęcia dyskusji):
■Jak źle się czujesz?
■ Czy myślałeś o zrobieniu sobie krzywdy?
■ Czy chciałeś umrzeć?
■ Czy myślałeś o zabiciu się?
■ Czy próbowałeś?
-Jak, kiedy i co doprowadziło do twojej próby?
-Jeśli nie próbowałeś, co skłoniło cię do powstrzymania się?
■ Czy czujesz się bezpiecznie wracając do domu?
-Jakie ustalenia można poczynić, aby zwiększyć twoje bezpieczeństwo i zmniejszyć ryzyko działania pod wpływem myśli samobójczych?
20. Jak najlepiej zakończyć pierwszą rozmowę ewaluacyjną?
Jednym ze sposobów jest zapytanie pacjenta, czy ma jakieś konkretne pytania lub wątpliwości, na które nie odpowiedział. Po omówieniu takich zagadnień krótko podsumuj istotne wrażenia i wnioski diagnostyczne, a następnie zasugeruj sposób postępowania. Bądź tak jasny, jak to możliwe, jeśli chodzi o sformułowanie problemu, diagnozę i kolejne kroki. To czas, aby wspomnieć o konieczności wykonania jakichkolwiek badań, w tym badań laboratoryjnych i dalszych badań psychologicznych oraz uzyskania zgody na spotkanie lub rozmowę z ważnymi osobami, które mogą dostarczyć potrzebnych informacji lub powinny zostać uwzględnione w planie leczenia.
Zarówno klinicysta, jak i pacjent powinni uznać, że plan jest wstępny i może zawierać alternatywy, które wymagają dalszej dyskusji. Jeśli zalecone jest leczenie, klinicysta powinien opisać konkretne korzyści i oczekiwany przebieg, a także poinformować pacjenta o potencjalnych skutkach ubocznych, działaniach niepożądanych i alternatywnych metodach leczenia. Często pacjenci chcą przemyśleć sugestie, uzyskać więcej informacji na temat leków lub porozmawiać z członkami rodziny. W większości przypadków sytuacja kliniczna nie jest na tyle wyłaniająca się, aby podczas pierwszego wywiadu konieczne było podjęcie zdecydowanych działań. Należy jednak jasno przedstawiać zalecenia, nawet jeśli są one wstępne i ukierunkowane przede wszystkim na dalszą diagnostykę.
W tym momencie kuszące jest zapewnienie fałszywego zapewnienia, na przykład: „Wiem, że wszystko będzie dobrze". Jest całkowicie uzasadnione — a nawet lepsze — dopuszczanie niepewności, gdy niepewność istnieje. Pacjenci mogą tolerować niepewność, jeśli widzą, że klinicysta ma plan dalszego wyjaśnienia problemu i wypracowania solidnego planu leczenia.
Taka dyskusja może wymagać przedłużenia, dopóki nie będzie jasne, czy pacjent może bezpiecznie opuścić szpital lub czy wymaga przyjęcia do szpitala).
Robert Waldinger M.D.
Alan M. Jacobson M.D.
WSTĘPNY WYWIAD PSYCHIATRYCZNY (tłumaczenie Google)
Robert Waldinger
Alan M.Jacobson
1 .Jakie są główne cele pierwszego wywiadu psychiatrycznego?
Postawienie wstępnej diagnostyki różnicowej i sformułowanie planu leczenia. Cele te osiąga się poprzez:
Zbieranie informacji:
- Główne dolegliwości, problem: historia obecnych i przeszłych myśli samobójczych lub wyobrażeń o zabójstwie
- Historia przedstawianych problemów: aktualna i przeszła historia doświadczania przemocy (np. przemoc domowa, znęcanie się nad dziećmi)
- Czynniki wywołujące: historia wcześniejszych problemów ze zdrowiem psychicznym, w tym diagnoza i leczenie psychiatryczne
- Objawy: przebieg i nasilenie dolegliwości w kontekście rozwoju i doświadczeń społecznych
- Afektywny: historia doświadczeń kryzysu psychicznego w rodzinie i wśród osób z osobistej sieci społecznej
- Poznawczy: historia rozwoju poznawczego
- Fizyczny: historia doświadczenia chorób somatycznych i ich leczenia
- Używanie i nadużywanie substancji:
- Doświadczenia zmian w pełnieniu ról społecznych i funkcjonowaniu społecznym:
■ Dojście do empatycznego zrozumienia, jak czuje się pacjent. To zrozumienie jest podstawą do nawiązania relacji z pacjentem.
Kiedy klinicysta uważnie słucha, a następnie wyraża uznanie dla zmartwień i trosk pacjenta, pacjent zyskuje poczucie, że jest rozumiany. To poczucie bycia zrozumianym jest podstawą całego późniejszego leczenia i pozwala klinicyście zainicjować związekw którym można zawrzeć sojusz na rzecz leczenia.
2. To dużo, na czym należy się skupić podczas pierwszego spotkania. A pomoc pacjentowi?
Wstępna diagnoza i plan leczenia mogą być szczątkowe. Rzeczywiście, gdy pacjenci są w kryzysie, historia może być niejasna, niekompletna lub zawężona. W rezultacie niektóre interwencje są podejmowane nawet wtedy, gdy zbierane są podstawowe informacje o
historii, relacjach rodzinnych i obecnych stresorach. Bardzo ważne jest, aby pamiętać, że trudności emocjonalne często powodują izolację. Doświadczenie dzielenia się swoim problemem
z zatroskanym słuchaczem może samo w sobie przynieść ogromną ulgę. Tak więc wstępny wywiad jest początkiem leczenia jeszcze przed ustaleniem formalnego planu leczenia.
3. Jak powinna być zorganizowana rozmowa wstępna?
Nie ma jednego ideału, ale warto pomyśleć o wstępnej rozmowie zgłoszeniowej jako składającej się z trzech elementów:
Nawiąż wstępny kontakt z pacjentem i zapytaj o zgłaszaną skargę lub problemy, czyli o to, co sprowadziło pacjenta na pierwsze spotkanie. Niektórzy pacjenci opowiadają swoje historie bez większych wskazówek ze strony klinicysty, podczas gdy inni wymagają wyraźnych instrukcji w formie konkretnych pytań, które pomogą im uporządkować myśli. Podczas tej fazy pierwszego wywiadu pacjent powinien mieć jak najwięcej możliwości podążania za własnymi schematami myślowymi.
Uzyskaj określone informacje, w tym historię prezentowanych problemów, istotne informacje medyczne, pochodzenie rodzinne, historię społeczną oraz określone objawy i wzorce zachowań. Formalnie przetestuj stan psychiczny (patrz ten rozdział).
Zapytaj, czy pacjent ma jakieś pytania lub o których nie wspomniał obawy. Następnie pacjent otrzymuje wstępne zalecenia dotyczące dalszej oceny i/lub rozpoczęcia leczenia.
Chociaż te trzy części wywiadu można rozpatrywać oddzielnie, często przeplatają się one ze sobą, np. obserwacje stanu psychicznego można prowadzić od momentu spotkania klinicysty z pacjentem.
Stosowny wywiad medyczny i rodzinny może zostać przywołany w trakcie przedstawiania innych obaw, a pacjenci mogą zadawać ważne pytania dotyczące zaleceń dotyczących leczenia, gdy przedstawiają swój początkowy wywiad.
4. Czy wstępna ocena różni siew przypadku złożonych sytuacji?
Wstępna ocena psychiatryczna może wymagać więcej niż jednej sesji w złożonych sytuacjach - na przykład podczas oceny dzieci lub rodzin lub oceny przydatności pacjenta do określonego podejścia terapeutycznego, takiego jak krótka psychoterapia. Wstępna ocena może również wymagać zebrania informacji z innych źródeł: rodziców, dzieci, współmałżonka, najlepszego przyjaciela, nauczyciela, funkcjonariuszy policji i/lub innych pracowników służby zdrowia. Kontakty te mogą zostać włączone do pierwszej wizyty lub mogą wystąpić później. Pierwszym krokiem w dokonywaniu takich usta leń jest wyjaśnienie pacjentowi powodu ich zawarcia oraz uzyskanie wyraźnej, pisemnej zgody na kontakt.
5. Jak należy podejść do źródła skierowań?
Prawie zawsze właściwe jest skontaktowanie się ze źródłem skierowania w celu zebrania informacji i wyjaśnienia wstępnych wrażeń diagnostycznych i planów leczenia. Wyjątki mogą wystąpić, gdy skierowanie pochodzi od innych pacjentów, przyjaciół lub innych osób niebędących profesjonalistami, których pacjent chce wykluczyć z leczenia.
6. Czy istnieją jakieś odmiany tych wytycznych dla wstępnej oceny?
Konkretne orientacje teoretyczne mogą dyktować istotne różnice w wstępnej ocenie. Na przykład terapeuta behawioralny kieruje dyskusję do konkretnych analiz bieżących problemów i poświęca niewiele czasu na doświadczenia z wczesnego dzieciństwa. Ocena psychofarmakologiczna kładzie nacisk na specyficzne wzorce objawów, reakcje na wcześniejsze leczenie farmakologiczne oraz występowanie chorób psychicznych w rodzinie. Podejście przedstawione w tym rozdziale jest zestawem zasad o szerokim zastosowaniu, które można zastosować w ocenie większości pacjentów.
7. W jaki sposób zbierane są informacje z wywiadu?
Klinicysta musi dowiedzieć się jak najwięcej o tym, jak pacjent myśli i czuje. Podczas wywiadu klinicznego zbierane są informacje z tego, co pacjent mówi klinicyście; krytycznie ważne wskazówki pochodzą również z tego, jak rozwija się historia. Zatem zarówno treść wywiadu (tj. to, co mówi pacjent), jak i przebieg wywiadu (tj. sposób, w jaki pacjent to mówi) oferują ważne drogi do zrozumienia problemów pacjenta. Weź pod uwagę kolejność przekazywanych informacji, komfort mówienia o nich, emocje związane z dyskusją, reakcje pacjenta na pytania i wstępne uwagi, spójność prezentacji oraz czas podania informacji. Pełne opracowanie takich informacji może zająć jedną lub kilka sesji w ciągu dni, tygodni lub miesięcy, ale podczas pierwszego wywiadu można zasugerować głębsze obawy.
Na przykład 35-letnia kobieta zgłosiła zaniepokojenie nawracającą astmą jej syna i związanymi z tym trudnościami w szkole. Swobodnie mówiła o swoich obawach i zasięgała rady, jak pomóc synowi. Zapytana o myśli męża, na chwilę się uspokoiła. Następnie powiedziała, że podziela jej obawy i przeniosła dyskusję z powrotem na jej syna. Jej wahanie wskazywało na inne problemy, które pozostały nierozwiązane podczas pierwszej sesji. Rzeczywiście, zaczęła kolejną sesję od pytania: „Czy mogę mówić o czymś innym niż o moim synu?". Uspokoiwszy się, opisała chroniczną złość męża na syna z powodu jego „słabości". Jego złość i jej własne uczucia w odpowiedzi stały się ważnym celem późniejszego leczenia.
8. Jak należy rozpocząć rozmowę zgłoszeniową?
Tu i teraz jest miejscem, w którym zaczyna się wszystkie wywiady. Można zadać jedno z wielu prostych pytań: „Co cię dzisiaj do mnie sprowadza? Możesz mi powiedzieć, co cię trapi?Jak
Czy to dlatego, że zdecydowałeś się umówić na to spotkanie? W przypadku niespokojnych pacjentów przydatna jest struktura: wczesne zapytanie o wiek, stan cywilny i sytuację życiową może dać im czas na stanie się czują się komfortowo, zanim przystąpią do opisu swoich problemów. Jeśli lęk jest ewidentny, prosty komentarz na temat lęku może pomóc pacjentom porozmawiać o swoich zmartwieniach.
9. Czy wysoce ustrukturyzowany format jest ważny?
Nie. Pacjenci muszą mieć możliwość uporządkowania swoich informacji w sposób, który im najbardziej odpowiada. Klinicysta, który przedwcześnie poddaje pacjenta strumieniowi konkretnych pytań, ogranicza informacje o własnym procesie myślowym pacjenta, nie uczy się, jak pacjent radzi sobie z ciszą lub smutkiem, odcina mu możliwość podpowiedzi lub wprowadzenia nowych tematów.
Ponadto zadanie polegające na formułowaniu jednego konkretnego pytania po drugim może zakłócać zdolność lekarza do słuchania i rozumienia pacjenta.
Nie oznacza to, że należy unikać konkretnych pytań. Często pacjenci udzielają rozbudowanych odpowiedzi na konkretne pytania, takie jak „Kiedy byłeś żonaty?" Ich odpowiedzi mogą otworzyć nowe możliwości dochodzenia. Kluczem jest unikanie szybkiego podejścia i umożliwienie pacjentom rozwinięcia myśli.
10. Jak należy zadawać pytania?
Pytania powinny być formułowane w sposób zachęcający pacjentów do rozmowy. Pytania otwarte, które nie wskazują odpowiedzi, zwykle pozwalają ludziom rozwinąć więcej niż pytania szczegółowe lub naprowadzające. Ogólnie rzecz biorąc, pytania naprowadzające (np. „Czy czułeś się smutny, kiedy twoja dziewczyna się wyprowadziła?") mogą przeszkadzać w rozmowie, ponieważ mogą sprawiać wrażenie, że osoba przeprowadzająca wywiad oczekuje od pacjenta pewnych uczuć. Niewiodące pytania („Jak się czułeś, kiedy twoja dziewczyna się wyprowadziła?") są równie bezpośrednie i skuteczniejsze.
11. Jaki jest skuteczny sposób radzenia sobie z wahaniami pacjentów?
Kiedy pacjenci potrzebują pomocy w opracowaniu, proste stwierdzenie i/lub prośba mogą wywołać więcej informacji: „Opowiedz mi o tym więcej". Powtarzanie lub zastanawianie się nad tym, co mówią pacjenci, również zachęca ich do otwarcia się (np. „Mówiłeś o swojej dziewczynie"). Czasami komentarze, które konkretnie odzwierciedlają zrozumienie przez lekarza odczuć pacjenta w związku ze zdarzeniami, mogą pomóc pacjentowi rozwinąć temat. Takie podejście zapewnia potwierdzenie zarówno klinicyście, jak i pacjentowi, że nadają na tych samych falach. Gdy klinicysta prawidłowo zareaguje na ich odczucia, pacjenci często potwierdzają odpowiedź poprzez dalszą dyskusję. Pacjent, którego dziewczyna odeszła, może czuć się zrozumiany i swobodniej rozmawiać o stracie po komentarzu typu „Wydajesz się zniechęcony wyprowadzką swojej dziewczyny".
12. Podaj przykład, jak kompleksowe gromadzenie informacji może wskazać problem.
Starszy mężczyzna został skierowany z powodu narastającego przygnębienia. W pierwszym wywiadzie opisał najpierw trudności finansowe, a następnie poruszył niedawny rozwój problemów medycznych, których kulminacją była diagnoza raka prostaty. Kiedy zaczął mówić o raku i chęci poddania się, zamilkł. W tym momencie wywiadu klinicysta wyraził uznanie, że pacjent wydawał się być przytłoczony narastającymi problemami finansowymi i, w większości, wszystko, medyczne zmiany. Pacjent cicho skinął głową, a następnie rozwinął swoje szczególne obawy dotyczące tego, jak jego żona będzie sobie radzić po jego śmierci. Nie czuł, że jego dzieci będą jej pomocne. Nie było jeszcze jasne, czyjego pesymizm odzwierciedlał depresyjną nadmierną reakcję na diagnozę raka, czy też dokładną ocenę rokowania. Dalsza ocena objawów i stanu psychicznego oraz krótka rozmowa z żoną w dalszej części spotkania wykazały, że rokowania są całkiem dobre. Następnie leczenie koncentrowało się na jego depresyjnych reakcjach na diagnozę.
13. Jak najlepiej formułować pytania?
Klinicysta powinien używać języka, który nie jest techniczny ani nadmiernie intelektualny. Jeśli to możliwe, należy używać własnych słów pacjenta. Jest to szczególnie ważne w przypadku spraw intymnych, takich jak problemy seksualne. Ludzie opisują swoje doświadczenia seksualne w dość zróżnicowanym języku. Jeśli pacjent mówi, że jest gejem, użyj dokładnie tego terminu, a nie pozornie równoważnego terminu, takiego jak homoseksualista. Ludzie używają niektórych słów, a innych nie, ze względu na specyficzne konotacje, jakie niosą dla nich różne słowa; na początku takie rozróżnienia mogą nie być oczywiste dla klinicysty.
14. A co z pacjentami, którzy nie są wstanie porozumiewać się w spójny sposób?
Klinicysta musi przez cały czas być świadomy tego, co dzieje się podczas wywiadu. Jeśli pacjent ma halucynacje lub jest bardzo zdenerwowany, nieuznanie zdenerwowania lub niepokojącego doświadczenia może zwiększyć niepokój pacjenta.
Omówienie aktualnego zdenerwowania pacjenta pomaga złagodzić napięcie i mówi pacjentowi, że lekarz słucha. Jeśli historia pacjenta jest chaotyczna lub niejasna, uznaj trudności w zrozumieniu pacjenta i oceń możliwe przyczyny (np. psychoza z poluzowanymi skojarzeniami vs. lęk przed wizytą).
Kiedy pytania ogólne (np. „Opowiedz mi coś o swoim pochodzeniu") są nieskuteczne, może być konieczne zadawanie szczegółowych pytań dotyczących rodziców, szkoły i dat wydarzeń. Pamiętaj jednak, że zadawanie niekończących się pytań w celu złagodzenia własnego niepokoju, a nie pacjenta, może być kuszące.
15. Podsumuj kluczowe punkty, o których należy pamiętać podczas pierwszego wywiadu.
Umożliwienie pacjentowi swobodnego opowiedzenia własnej historii musi być zrównoważone poprzez uwzględnienie zdolności pacjenta do skupienia się na istotnych tematach. Niektóre osoby wymagają wskazówek od klinicysty, aby uniknąć zagubienia się w stycznych tematach. Inni mogą potrzebować spójnej struktury, ponieważ mają problemy z uporządkowaniem myśli, być może z powodu wysokiego stopnia niepokoju. Empatyczny komentarz na temat niepokoju pacjenta może go zmniejszyć, a tym samym doprowadzić do wyraźniejszej komunikacji.
Niektóre wytyczne dotyczące rozmowy zgłoszeniowej
• Pozwól, aby pierwsza część wstępnego wywiadu podążała za tokiem myślenia pacjenta.
• Zapewnij strukturę, aby pomóc pacjentom, którzy mają problemy z uporządkowaniem myśli lub dokończeniem uzyskiwania określonych danych.
• Formułuj pytania, aby zachęcić pacjenta do rozmowy (np. pytania otwarte, nienaprowadzające).
• Używaj słów pacjenta.
• Bądź wyczulony na wczesne oznaki utraty kontroli nad zachowaniem (np. wstawanie do tempa).
• Zidentyfikuj mocne strony pacjenta oraz obszary problemowe.
• Unikaj żargonu i technicznego języka.
• Unikaj pytań zaczynających się od „dlaczego".
• Unikaj przedwczesnych zapewnień.
• Nie pozwalaj pacjentom zachowywać się niewłaściwie (np. łamać lub rzucać przedmiotami).
• postaw granice wobec wszelkich zagrażających zachowań i w razie potrzeby wezwij niezbędną pomoc.
16. Jakich konkretnych pułapek należy unikać podczas wstępna rozmowa zgłoszeniowa?
Unikaj żargonu lub terminów technicznych, chyba że jest to jasno wyjaśnione i konieczne. Pacjenci mogą używać żargonu, na przykład: „Miałem paranoję". Jeśli pacjent używa słowa technicznego, zapytaj o jego znaczenie. Możesz być zaskoczony zrozumieniem pacjenta. Na przykład pacjenci mogą używać słowa „paranoik", aby zasugerować strach przed dezaprobatą społeczną lub pesymizm co do przyszłości. Uważaj również, aby podczas wywiadu przypisać problemom pacjenta etykietę diagnostyczną. Pacjent może być przestraszony i zdezorientowany etykietą.
Ogólnie rzecz biorąc, unikaj zadawania pytań zaczynających się od „dlaczego". Pacjenci mogą nie wiedzieć, dlaczego mają określone doświadczenia lub uczucia i mogą czuć się nieswojo, a nawet głupio, jeśli uważają, że ich odpowiedzi nie są „dobre". Pytanie dlaczego oznacza również, że oczekujesz od pacjenta szybkich wyjaśnień.
Pacjenci dowiadują się więcej o źródłach swoich problemów, zastanawiając się nad swoim życiem podczas wywiadu i kolejnych sesji. Kiedy masz ochotę zapytać dlaczego, sformułuj pytanie tak, aby wywołało bardziej szczegółową odpowiedź.
Alternatywy obejmują „Co się stało?" „Jak to się stało?" lub „Co o tym myślisz?'
Unikaj przedwczesnej pewności siebie. Kiedy pacjenci są zdenerwowani, jak to często bywa podczas pierwszych wywiadów, osoba przeprowadzająca wywiad może ulec pokusie, by rozwiać obawy pacjenta, mówiąc: „Wszystko będzie dobrze" lub „Nie ma tu nic naprawdę złego".
Jednak zapewnienie jest prawdziwe tylko wtedy, gdy klinicysta (1) dokładnie zbadał charakter i zakres problemów pacjenta oraz (2) jest pewien tego, co mówi pacjentowi. Przedwczesne zapewnienie może zwiększyć niepokój pacjenta, sprawiając wrażenie, że lekarz wyciągnął pochopne wnioski bez dokładnej oceny lub po prostu mówi to, co pacjent chce usłyszeć. Pozostawia również pacjentów samych ze swoimi obawami oto, co naprawdę jest nie tak.
Co więcej, przedwczesne zapewnienia raczej zamykają dyskusję niż zachęcają do dalszych badań problem. Bardziej uspokajające może być zapytanie pacjenta, co go niepokoi. Proces (tj. charakter interakcji) pociesza pacjenta bardziej niż jakakolwiek pojedyncza rzecz, którą może powiedzieć klinicysta.
Postaw granice zachowaniom.
Z powodu problemów psychiatrycznych niektórzy pacjenci mogą stracić kontrolę nad sesją. Chociaż opisane tutaj podejście kładzie nacisk na pozwolenie pacjentowi na kierowanie dużą częścią werbalnej dyskusji, czasami należy wyznaczyć granice niewłaściwego zachowania. Pacjenci, którzy są podnieceni i chcą się rozebrać lub grożą, że rzucą przedmiotem, muszą być kontrolowani.
Cel ten najczęściej osiąga się poprzez komentowanie narastającego pobudzenia, omawianie go, dopytywanie o źródła niepokoju i informowanie pacjentów o granicach akceptowalnego zachowania. W rzadkich przypadkach pomoc z zewnątrz może być konieczna (np. ochroniarze na oddziale ratunkowym), zwłaszcza jeśli zachowanie się nasila, a przesłuchujący wyczuwa niebezpieczeństwo. Wywiad należy przerwać do czasu, gdy zachowanie pacjenta będzie można opanować w taki sposób, aby można było bezpiecznie kontynuować.
17. O czym często zapomina się w ocenie pacjentów?
Nowy pacjent nawiązuje kontakt z klinicystą z powodu problemów i zmartwień; to są uzasadnione pierwsze tematy wywiadu. Pomocne jest również zrozumienie mocnych stron pacjenta, które są podstawą, na której będzie opierać się leczenie. Mocne strony obejmują sposoby, w jakie pacjent z powodzeniem radził sobie z przeszłym i obecnym cierpieniem, osiągnięciami, źródłami wewnętrznej wartości, przyjaźniami, osiągnięciami w pracy i wsparciem rodziny. Mocne strony obejmują również hobby i zainteresowania, które pacjenci wykorzystują do walki ze swoimi zmartwieniami.
Pytania typu „Z czego jesteś dumny?" lub „Co lubisz w sobie?" może ujawnić takie informacje.
Często informacje wychodzą po namyśle w trakcie rozmowy. Na przykład jeden pacjent był bardzo dumny ze swojej wolontariatu w kościele. Wspomniał o tym tylko mimochodem, omawiając swoje zajęcia na tydzień przed spotkaniem. Jednak ta praca wolontariacka była jego jedynym aktualnym źródłem osobistej wartości. Zwrócił się do niego, gdy zdenerwował się brakiem sukcesów w karierze.
18. Jaka jest rola humoru w wywiadzie?
Pacjenci mogą używać humoru, aby odwrócić rozmowę od tematów wywołujących lęk lub niepokojących. Czasami przydatne może być zezwolenie na takie odchylenia, aby pomóc pacjentom zachować równowagę emocjonalną. Jednak zbadaj dalej, czy humor wydaje się prowadzić do radykalnej zmiany tematu, który wydawał się ważny i / lub emocjonalnie istotny. Humor może również skierować klinicysta w kierunku nowych obszarów do zbadania.
Lekki żart pacjenta (np. o seksie) może być pierwszym krokiem do wprowadzenia tematu, który później nabiera znaczenia.
Ze strony klinicysty humor może mieć charakter ochronny i obronny. Tak jak pacjent może odczuwać niepokój lub dyskomfort, tak samo może czuć się osoba przeprowadzająca wywiad. Uważaj, bo humor może przynieść odwrotny skutek. Może to zostać odebrane jako kpina. Może również pozwolić zarówno pacjentowi, jak i klinicyście uniknąć ważnych tematów. Czasami humor jest wspaniałym sposobem na pokazanie ludzkich cech rozmówcy i tym samym zbudowanie terapeutycznego sojuszu. Mimo wszystko pamiętaj o problematycznych aspektach humoru, zwłaszcza gdy ty i twój pacjent nie znacie się dobrze.
19. Jak ocenia się zamiary samobójcze?
Ze względu na częstość występowania zaburzeń depresyjnych i ich związek z samobójstwem, podczas pierwszego wywiadu zawsze należy uwzględnić możliwość wystąpienia intencji samobójczych. Pytanie o samobójstwo nie sprowokuje do aktu. Jeśli temat nie pojawia się spontanicznie, można użyć kilku pytań, aby wydobyć myśli pacjenta na temat samobójstwa (wymienione w kolejności, w jakiej można je wykorzystać do rozpoczęcia dyskusji):
■Jak źle się czujesz?
■ Czy myślałeś o zrobieniu sobie krzywdy?
■ Czy chciałeś umrzeć?
■ Czy myślałeś o zabiciu się?
■ Czy próbowałeś?
-Jak, kiedy i co doprowadziło do twojej próby?
-Jeśli nie próbowałeś, co skłoniło cię do powstrzymania się?
■ Czy czujesz się bezpiecznie wracając do domu?
-Jakie ustalenia można poczynić, aby zwiększyć twoje bezpieczeństwo i zmniejszyć ryzyko działania pod wpływem myśli samobójczych?
20. Jak najlepiej zakończyć pierwszą rozmowę ewaluacyjną?
Jednym ze sposobów jest zapytanie pacjenta, czy ma jakieś konkretne pytania lub wątpliwości, na które nie odpowiedział. Po omówieniu takich zagadnień krótko podsumuj istotne wrażenia i wnioski diagnostyczne, a następnie zasugeruj sposób postępowania. Bądź tak jasny, jak to możliwe, jeśli chodzi o sformułowanie problemu, diagnozę i kolejne kroki. To czas, aby wspomnieć o konieczności wykonania jakichkolwiek badań, w tym badań laboratoryjnych i dalszych badań psychologicznych oraz uzyskania zgody na spotkanie lub rozmowę z ważnymi osobami, które mogą dostarczyć potrzebnych informacji lub powinny zostać uwzględnione w planie leczenia.
Zarówno klinicysta, jak i pacjent powinni uznać, że plan jest wstępny i może zawierać alternatywy, które wymagają dalszej dyskusji. Jeśli zalecone jest leczenie, klinicysta powinien opisać konkretne korzyści i oczekiwany przebieg, a także poinformować pacjenta o potencjalnych skutkach ubocznych, działaniach niepożądanych i alternatywnych metodach leczenia. Często pacjenci chcą przemyśleć sugestie, uzyskać więcej informacji na temat leków lub porozmawiać z członkami rodziny. W większości przypadków sytuacja kliniczna nie jest na tyle wyłaniająca się, aby podczas pierwszego wywiadu konieczne było podjęcie zdecydowanych działań. Należy jednak jasno przedstawiać zalecenia, nawet jeśli są one wstępne i ukierunkowane przede wszystkim na dalszą diagnostykę.
W tym momencie kuszące jest zapewnienie fałszywego zapewnienia, na przykład: „Wiem, że wszystko będzie dobrze". Jest całkowicie uzasadnione — a nawet lepsze — dopuszczanie niepewności, gdy niepewność istnieje. Pacjenci mogą tolerować niepewność, jeśli widzą, że klinicysta ma plan dalszego wyjaśnienia problemu i wypracowania solidnego planu leczenia.
Taka dyskusja może wymagać przedłużenia, dopóki nie będzie jasne, czy pacjent może bezpiecznie opuścić szpital lub czy wymaga przyjęcia do szpitala).
Rozliczanie świadczeń zdrowotnych w USA według wykonań „fee-for-service” (odpowiednio w Polsce - produkty rozliczeniowe w NFZ, zdarzenia medyczne w systemie IT)
BILLING and LEGAL STUFF
Your Signature (and a supervisor signature, if required)
Date of Service
Start and Stop Times of the Group
Total Time
ICD-10 Code
CPT Code
https://therathink.com/mental-health-cpt-codes/
The Most Common Mental Health CPT Codes (najbardziej powszechne kody procedur w opiece psychiatrycznej)
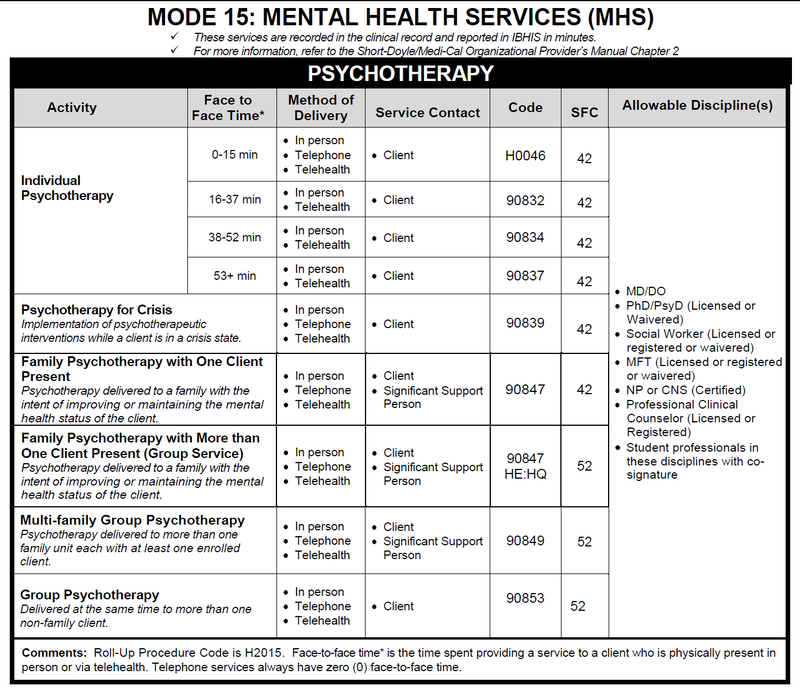
The most common CPT Codes used by therapists and behavioral health professionals:
Outpatient Mental Health Therapist Diagnostics, Evaluation, Intake CPT Code:
Outpatient Psychiatry Diagnostics / Evaluation / Client Intake CPT Code:
● Psychotherapy must be at least 16 minutes.
● Time is very important and should be rounded to the nearest CPT Code.
● Outpatient vs. Inpatient is not important.
● E/M codes can only be used by prescribers (MD, DO, APN, PA).
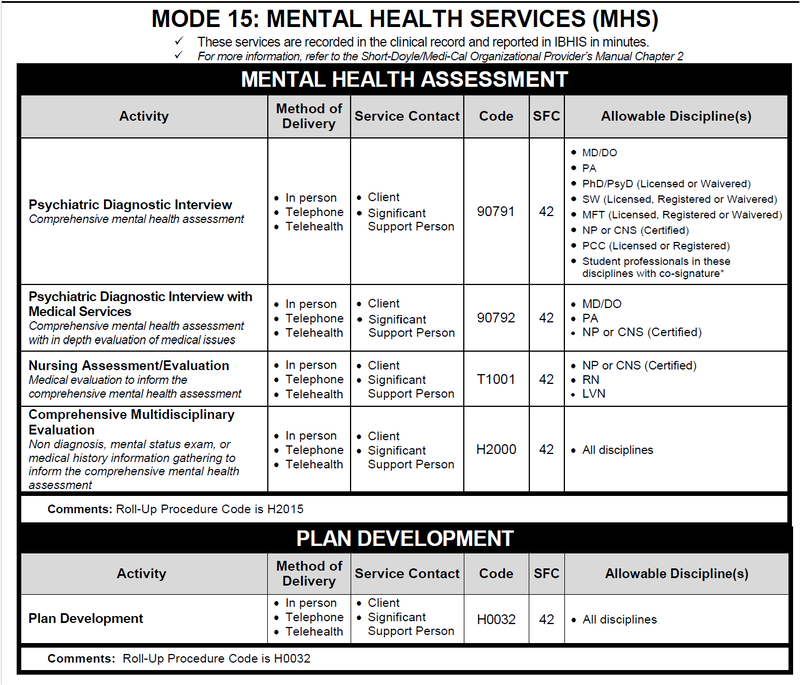
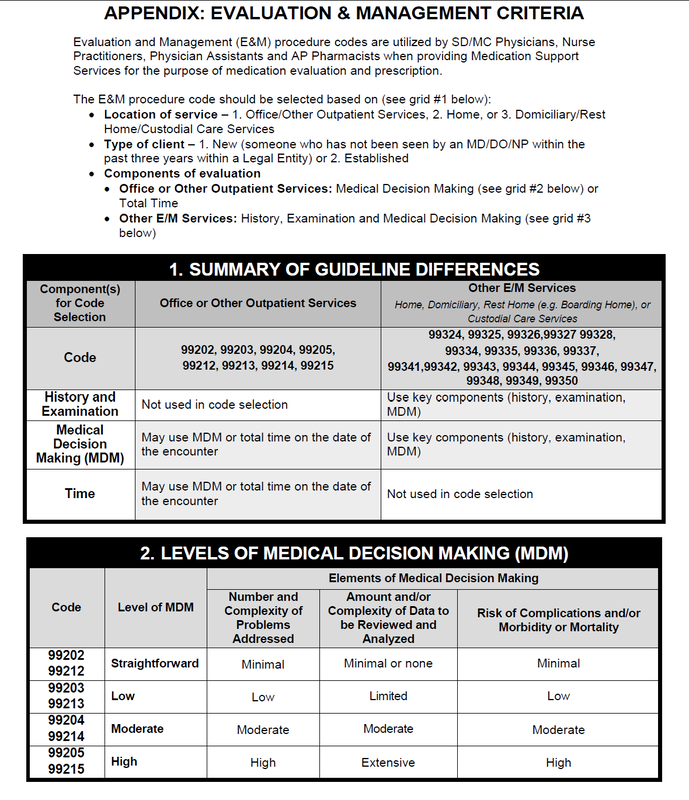
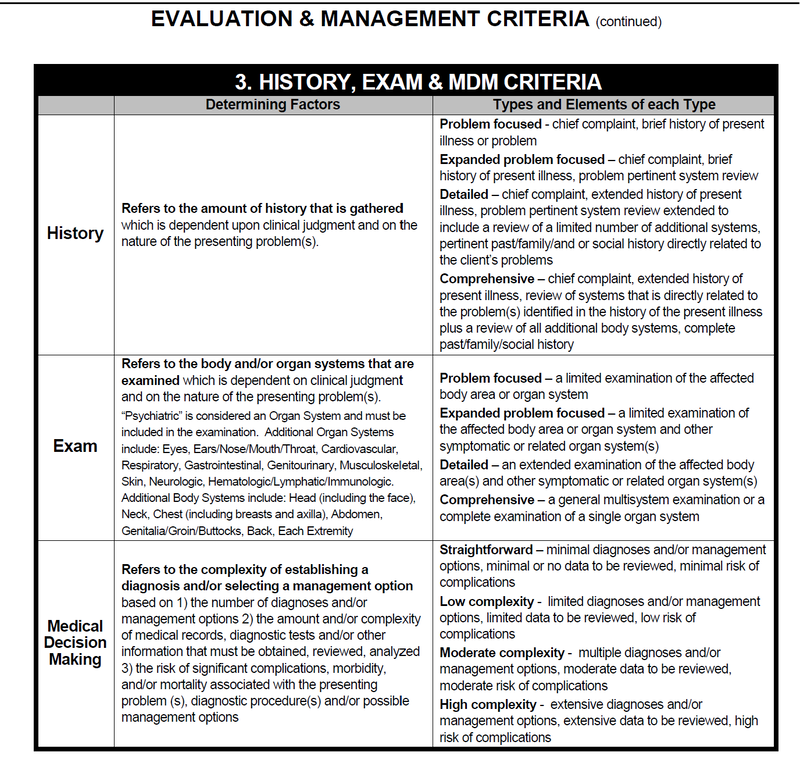
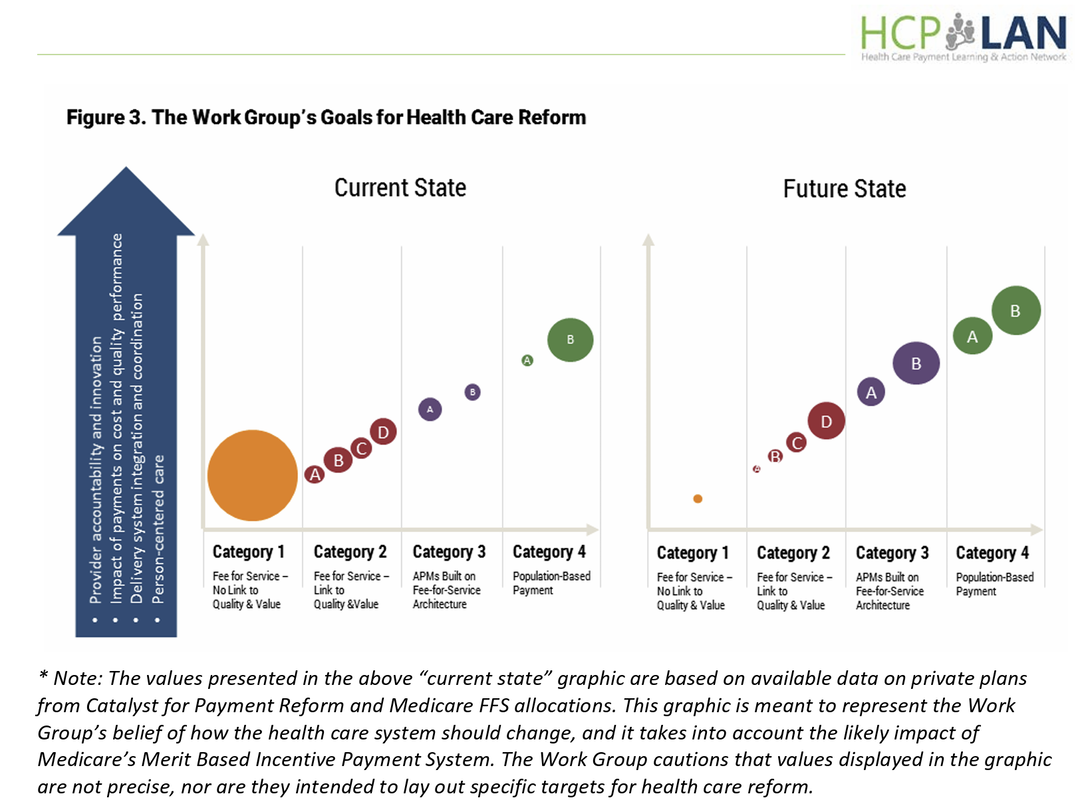
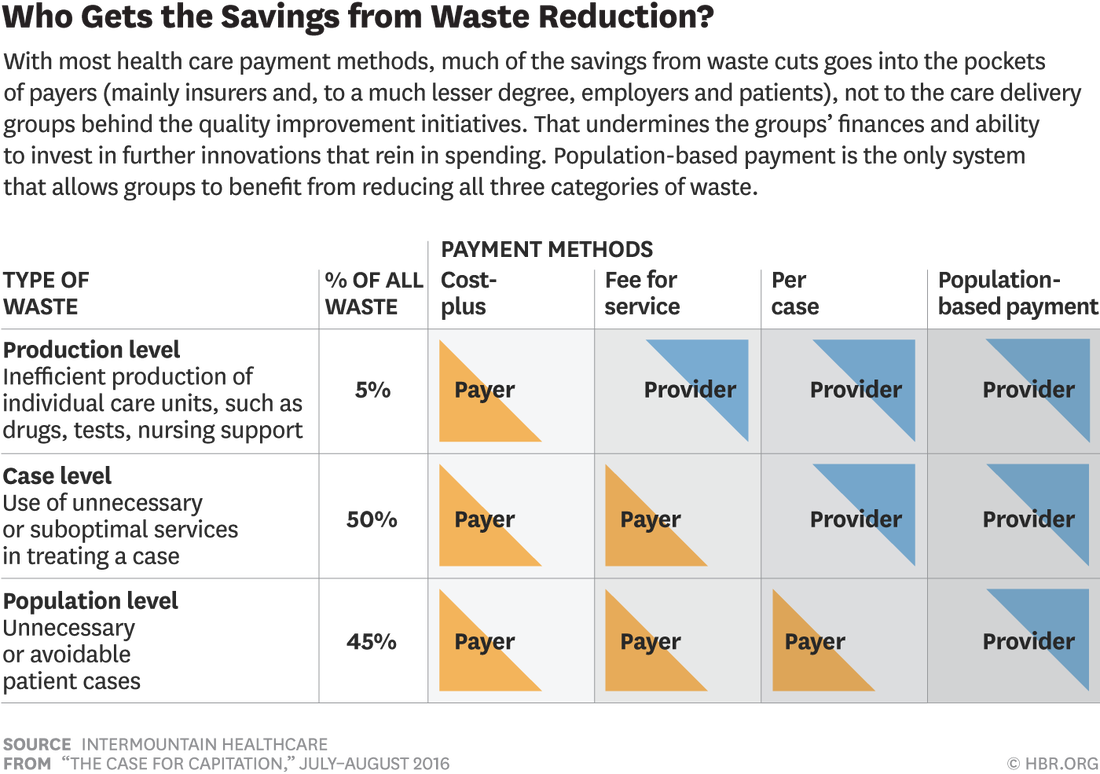
Lektura amerykańskiej klasyfikacji świadczeń w opiece psychiatrycznej opracowanej do rozliczeń „fee-for-service” pozwala dokonać porównań i wyciągnąć różne wnioski. W rozliczeniach za wykonanie świadczeń bierze się pod uwagę:
Personel – kto wykonywał świadczenie
Termin – data wykonania świadczenia
Czas rozpoczęcia i zakończenia, czas trwania świadczenia
ICD-10 rozpoznanie
KOD ŚWIADCZENIA/PROCEDURY
Lista KODÓW jest tak rozbudowana, że zawiera w sobie sumę informacji: profesjonalista, rodzaj świadczenia i czas jego wykonania.
Ciekawostką jest to, że “diagnostyczny wywiad psychiatryczny” 90791 – Psychiatric Diagnostic Evaluation (usually just one/client is covered) dzieli się na wywiad, który wykonują wszyscy pracownicy działalności podstawowej, oraz wywiad ze świadczeniem medycznym – porada lekarska diagnostyczna. W Polsce, z niezrozumiałych powodów porady diagnostyczne wykonuje albo lekarz psychiatra albo psycholog, co sugeruje urzędnikom nie wprost, że psychoterapeuta, pielęgniarka, terapeuta środowiskowy nie uczestniczą w procesie diagnostycznym, inaczej nie mogą spotkać się z pacjentem i porozmawiać z jakim problemem przychodzi, jak się czuje, czego potrzebuje i oczekuje!!!
Activity: Psychiatric Diagnostic Interview (Comprehensive mental health assessment) –
Allowable Discipline(s):
•Medical Doctor / Doctor of Osteopathy (completed a psychiatry residency program) lekarz psychiatra
•Physician Assistant (PA)
•Clinical Psychologist PhD/PsyD (Licensed or Waivered) psycholog
• Social Worker SW (Licensed, Registered or Waivered) pracownik socjalny
•Marriage & Family Therapist MFT (Licensed, Registered or Waivered)
•Nurse Practitioner (NP) or Clinical Nurse Specialist (CNS) (Certified) pielęgniarka
•Professional Clinical Counselor PCC (Licensed or Registered)
•Student professionals in these disciplines with co-signature*
Psychiatric Diagnostic Interview with Medical Services (Comprehensive mental health assessment with in depth evaluation of medical issues)
Allowable Discipline(s):
• MD/DO lekarz
• PA lekarz
• NP or CNS (Certified) pielęgniarka
BILLING and LEGAL STUFF
Your Signature (and a supervisor signature, if required)
Date of Service
Start and Stop Times of the Group
Total Time
ICD-10 Code
CPT Code
https://therathink.com/mental-health-cpt-codes/
The Most Common Mental Health CPT Codes (najbardziej powszechne kody procedur w opiece psychiatrycznej)
The most common CPT Codes used by therapists and behavioral health professionals:
Outpatient Mental Health Therapist Diagnostics, Evaluation, Intake CPT Code:
- 90791 – Psychiatric Diagnostic Evaluation (usually just one/client is covered)
- 90832 – Psychotherapy, 30 minutes (16-37 minutes).
- 90834 – Psychotherapy, 45 minutes (38-52 minutes).
- 90837 – Psychotherapy, 60 minutes (53 minutes and over).
- 90846 – Family or couples psychotherapy, without patient present.
- 90847 – Family or couples psychotherapy, with patient present.
- 90853 – Group Psychotherapy (not family).
- 98968 – Telephone therapy (non-psychiatrist) – limit 3 units/hours per application.
- 90839 – Psychotherapy for crisis, 60 minutes (30-74 minutes).
- +90840 – Add-on code for an additional 30 minutes (75 minutes and over). Used in conjunction with 90839.
- +90785 – Interactive Complexity add-on code. Covered below.
- 90404 – Cigna / MHN EAP CPT Code. These two companies use a unique CPT code for EAP sessions.
- 96101 – Psychological testing, interpretation and reporting by a psychologist (per Hour)
- 90880 – Hypnotherapy – limit 10 units/hours per application
- 90876 – Biofeedback
- 90849 – Multiple family group psychotherapy
- 90845 – Psychoanalysis
- Add-On CPT Code 90785 – Interactive complexity. Example: play therapy using dolls or other toys. This is an interactive complexity add-on code that is not a payable expense. This code only indicates that the treatment is complex in nature.
- Add-On CPT Code 90863 – Pharmacologic Management after therapy.
- Add-On CPT Code 99050 – Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed.
- Add-On CPT Code 99051 – Services provided in the office during regularly scheduled evening, weekend, or holiday office hours.
- Add-On CPT Code 99354 – Additional time after the additional time of 74 minutes. Adding another 30 minutes. (Only use if the duration of your session is at least 90 minutes for 90837 or 80 minutes for 90847).
- Add-On CPT Code 99355 – Additional time after first 60 minutes. First additional 30 to 74 minutes.
- Add-On CPT Code 90840 – 30 additional minutes of psychotherapy for crisis. Used only in conjunction with CPT 90839.
- Add-On CPT Code 90833 – 30 minute psychotherapy add-on. Example: Psychiatrist evaluates medication response, then has 30 minute session.
- Add-On CPT Code 90836 – 45 minute psychotherapy add-on. Example: Clinical Nurse Specialist evaluates medication response, then has 45 minute session.
Outpatient Psychiatry Diagnostics / Evaluation / Client Intake CPT Code:
- 90792 – Psychiatric Diagnostic Evaluation with medical services (usually just one/client is covered)
- 99201 – E/M – New Patient Office Visit – 10 Minutes
- 99202 – E/M – New Patient Office Visit – 20 Minutes
- 99203 – E/M – New Patient Office Visit – 30 Minutes
- 99204 – E/M – New Patient Office Visit – 45 Minutes
- 99205 – E/M – New Patient Office Visit – 60 Minutes
- 99211 – E/M – Established Patients – 5 Minutes
- 99212 – E/M – Established Patients – 10 Minutes
- 99213 – E/M – Established Patients – 15 Minutes
- 99214 – E/M – Established Patients – 25 Minutes
- 99215 – E/M – Established Patients – 40 Minutes
- 99443 – Telephone therapy (psychiatrist), – limit 3 units/hours per application
● Psychotherapy must be at least 16 minutes.
● Time is very important and should be rounded to the nearest CPT Code.
● Outpatient vs. Inpatient is not important.
● E/M codes can only be used by prescribers (MD, DO, APN, PA).
Lektura amerykańskiej klasyfikacji świadczeń w opiece psychiatrycznej opracowanej do rozliczeń „fee-for-service” pozwala dokonać porównań i wyciągnąć różne wnioski. W rozliczeniach za wykonanie świadczeń bierze się pod uwagę:
Personel – kto wykonywał świadczenie
Termin – data wykonania świadczenia
Czas rozpoczęcia i zakończenia, czas trwania świadczenia
ICD-10 rozpoznanie
KOD ŚWIADCZENIA/PROCEDURY
Lista KODÓW jest tak rozbudowana, że zawiera w sobie sumę informacji: profesjonalista, rodzaj świadczenia i czas jego wykonania.
Ciekawostką jest to, że “diagnostyczny wywiad psychiatryczny” 90791 – Psychiatric Diagnostic Evaluation (usually just one/client is covered) dzieli się na wywiad, który wykonują wszyscy pracownicy działalności podstawowej, oraz wywiad ze świadczeniem medycznym – porada lekarska diagnostyczna. W Polsce, z niezrozumiałych powodów porady diagnostyczne wykonuje albo lekarz psychiatra albo psycholog, co sugeruje urzędnikom nie wprost, że psychoterapeuta, pielęgniarka, terapeuta środowiskowy nie uczestniczą w procesie diagnostycznym, inaczej nie mogą spotkać się z pacjentem i porozmawiać z jakim problemem przychodzi, jak się czuje, czego potrzebuje i oczekuje!!!
Activity: Psychiatric Diagnostic Interview (Comprehensive mental health assessment) –
Allowable Discipline(s):
•Medical Doctor / Doctor of Osteopathy (completed a psychiatry residency program) lekarz psychiatra
•Physician Assistant (PA)
•Clinical Psychologist PhD/PsyD (Licensed or Waivered) psycholog
• Social Worker SW (Licensed, Registered or Waivered) pracownik socjalny
•Marriage & Family Therapist MFT (Licensed, Registered or Waivered)
•Nurse Practitioner (NP) or Clinical Nurse Specialist (CNS) (Certified) pielęgniarka
•Professional Clinical Counselor PCC (Licensed or Registered)
•Student professionals in these disciplines with co-signature*
Psychiatric Diagnostic Interview with Medical Services (Comprehensive mental health assessment with in depth evaluation of medical issues)
Allowable Discipline(s):
• MD/DO lekarz
• PA lekarz
• NP or CNS (Certified) pielęgniarka
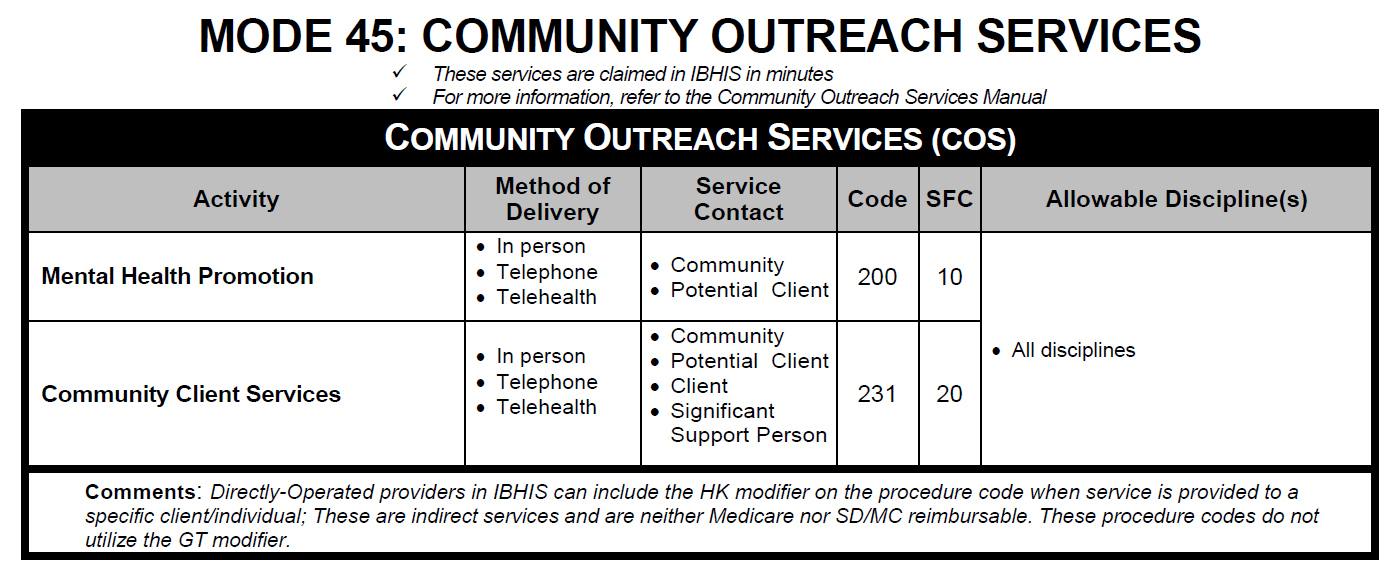
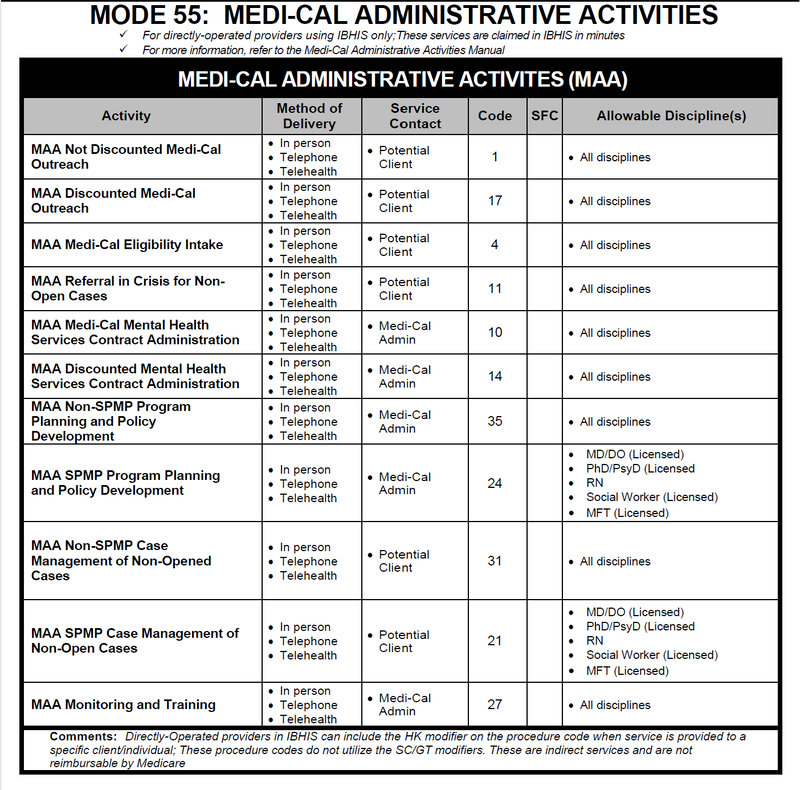
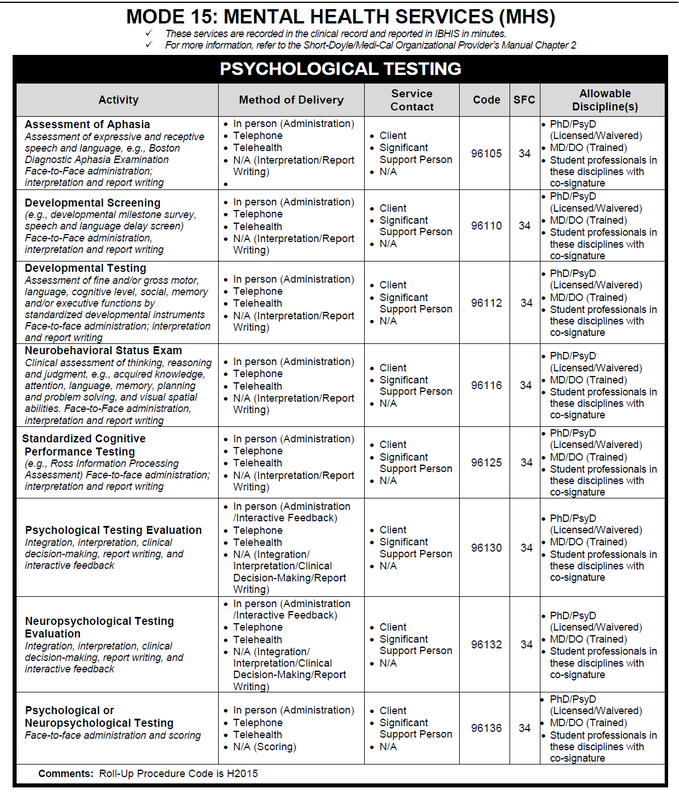
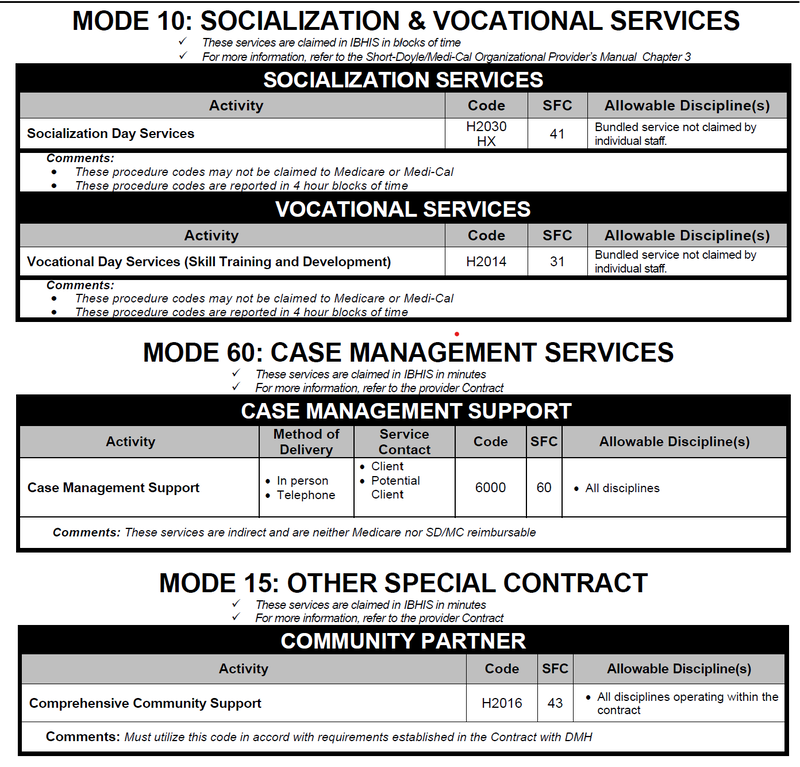
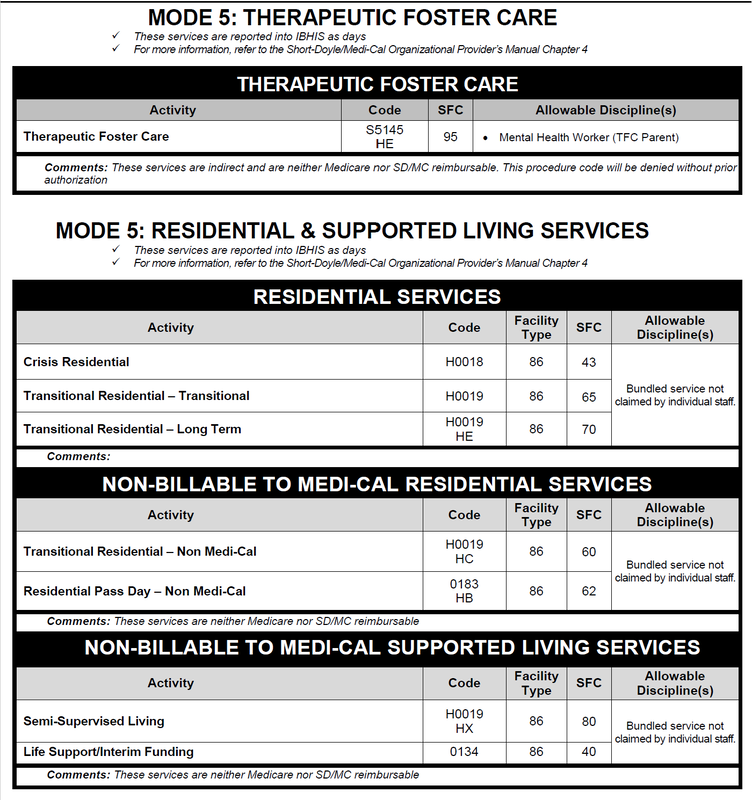
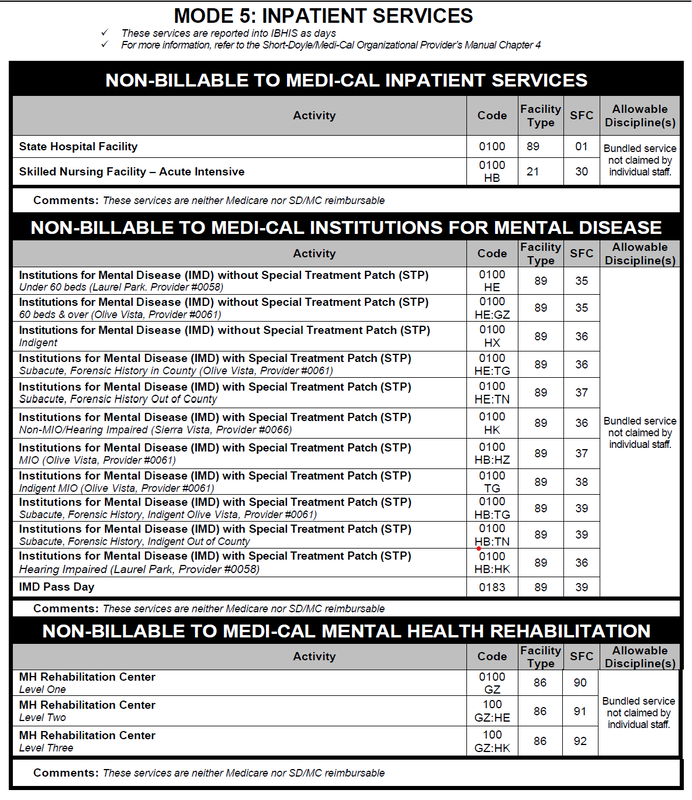
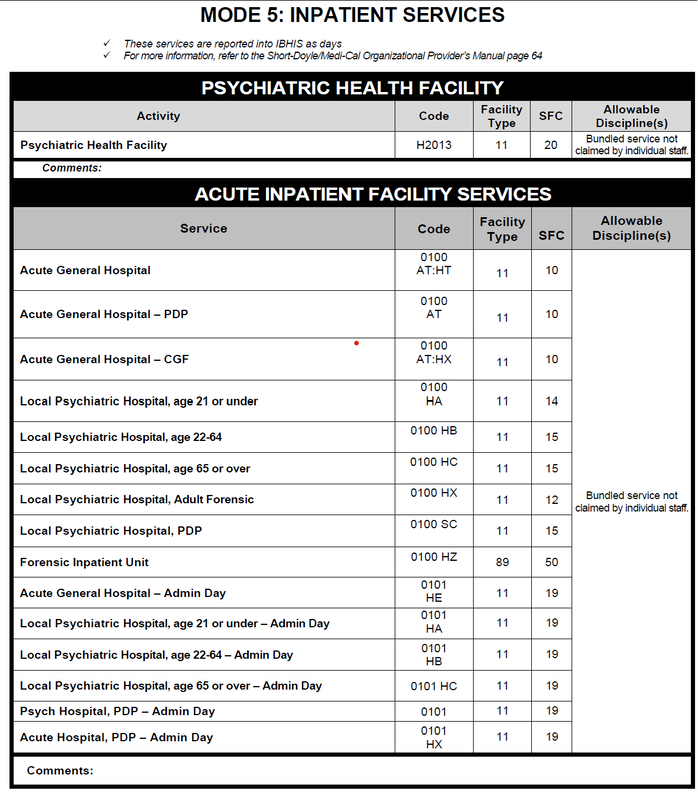
A GUIDE TO PROCEDURE CODES FOR CLAIMING MENTAL HEALTH SERVICES
County of Los Angeles – Department of Mental Health Quality Assurance Division, 2017
TABLE OF CONTENTS
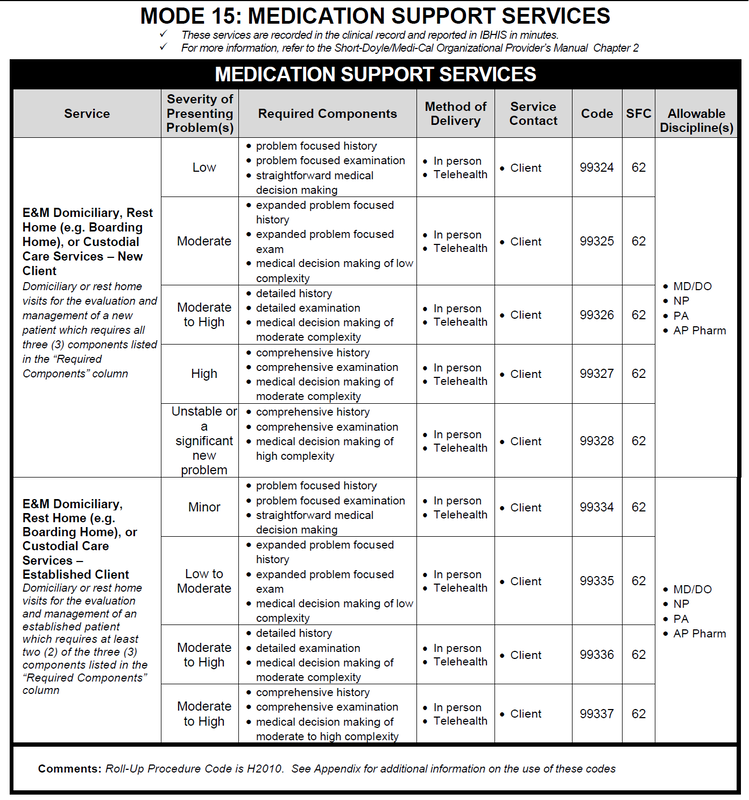
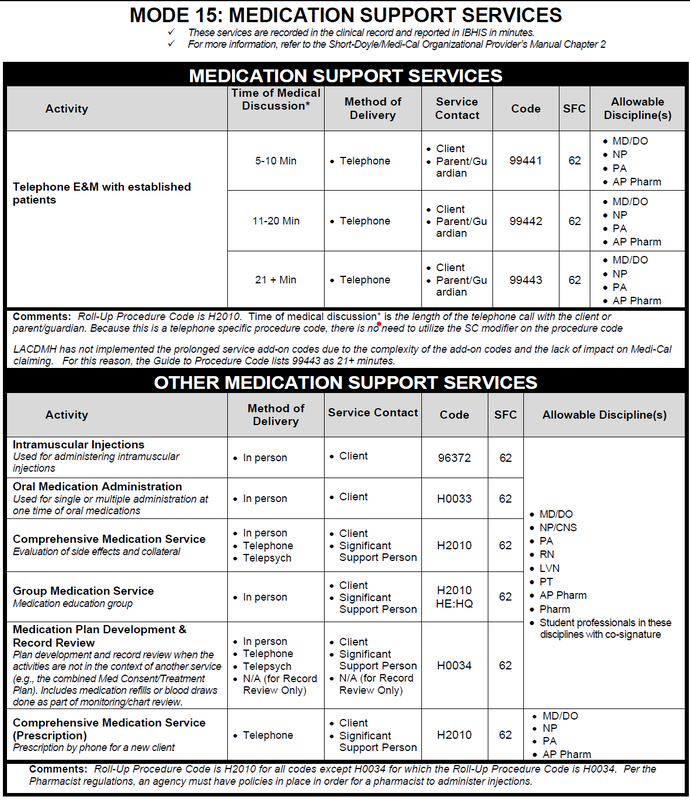
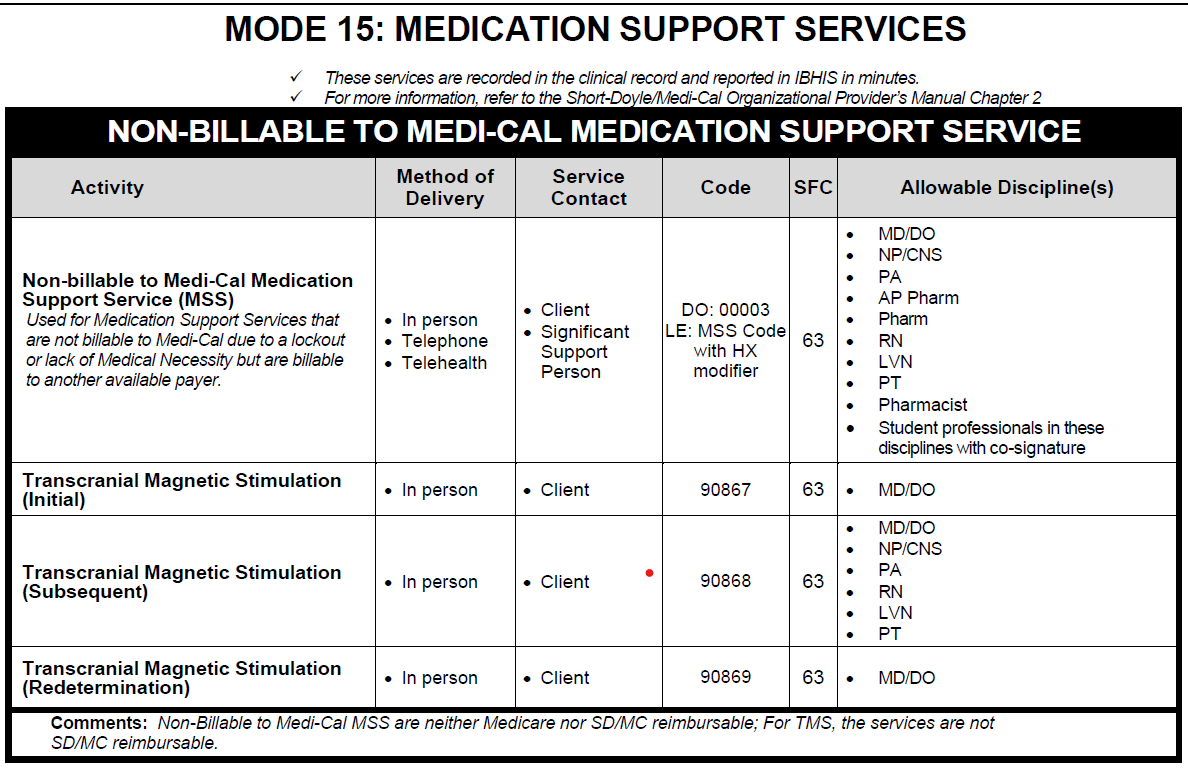
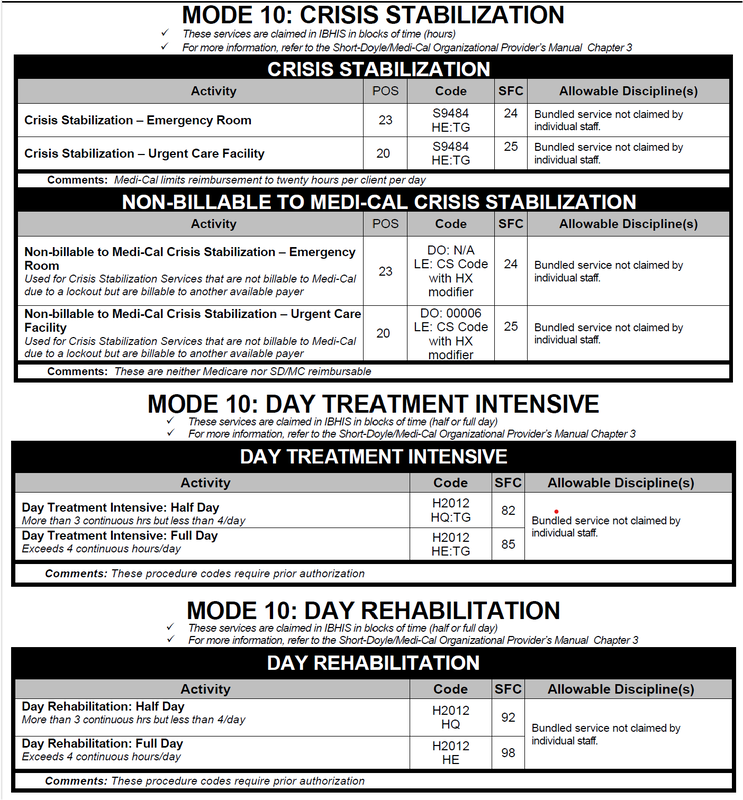
Specialty Mental Health Services – Outpatient and Day Services
Mental Health Services (Mode 15)
Clinical Assessment with Client
Plan Development
Individual Psychotherapy
Family and Group Services
Rehabilitation
Psychological Testing
Other Mental Health Services
Record Review
No Contact – Report Writing
Services to Special Populations
MAT
Intensive Home Based Services (IHBS)
TBS
Non-Billable to Medi-Cal Mental Health Services
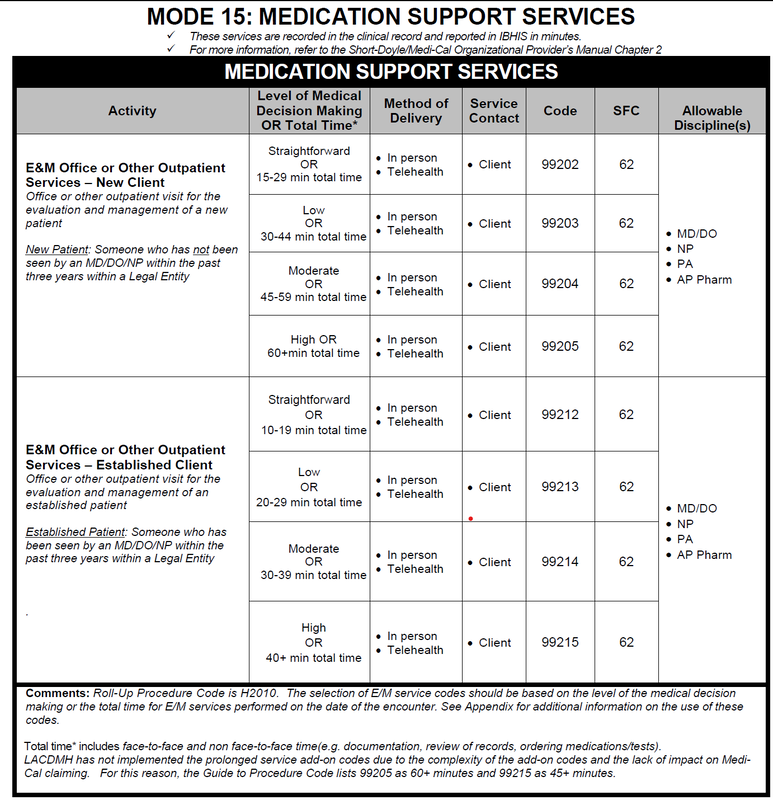
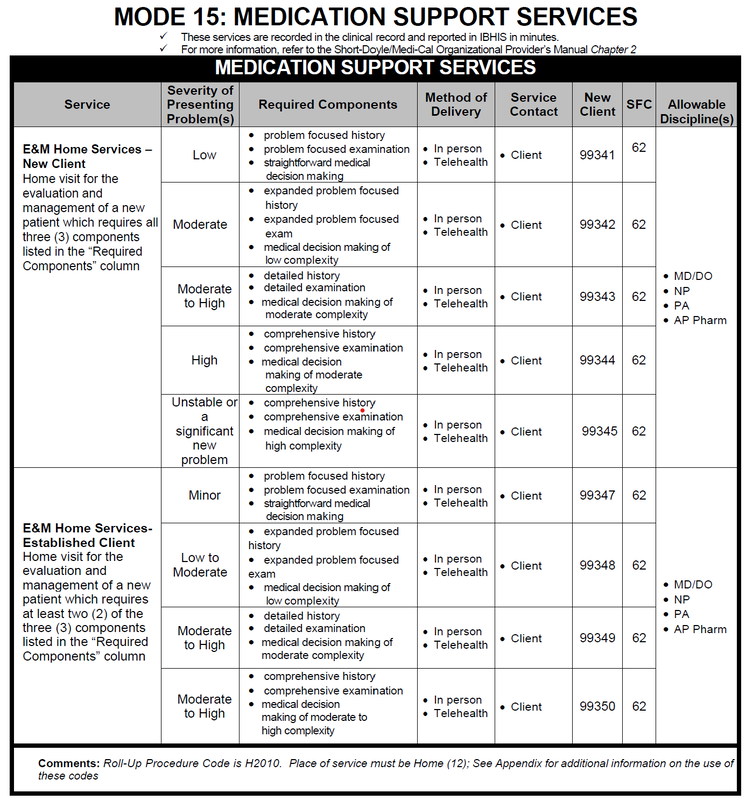
Medication Support Services (Mode 15)
Evaluation & Management
Medication Support
Non-Billable to Medi-Cal Medication Support Services
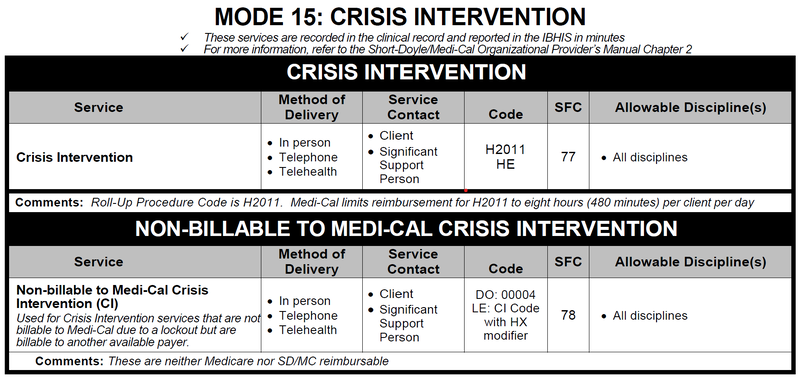
Crisis Intervention (Mode 15)
Crisis Intervention
Non Billable to Medi-Cal Crisis Intervention
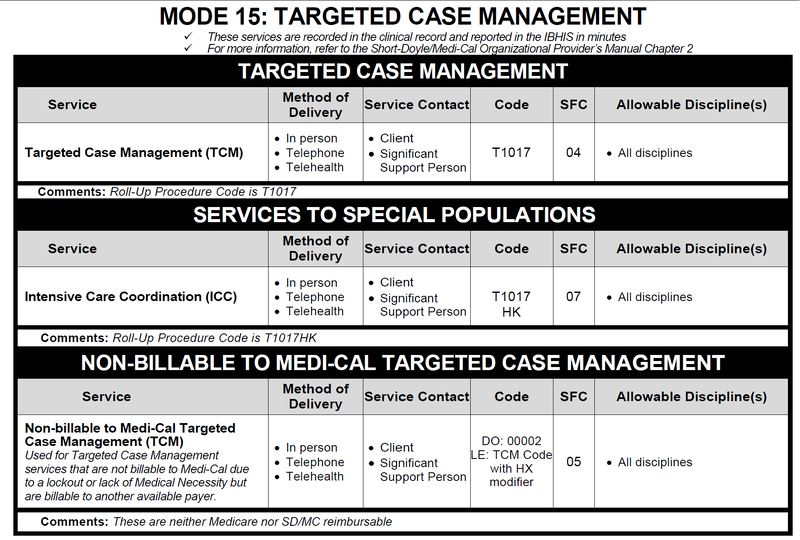
Targeted Case Management (Mode 15)
Targeted Case Management
Services to Special Populations
Intensive Care Coordination (ICC)
Non-Billable to Medi-Cal Targeted Case Management
Crisis Stabilization, Day Rehabilitation and Day Treatment Intensive (Mode 10)
Crisis Stabilization
Day Rehabilitation and Day Treatment Intensive
Non-Medi-Cal Services
Socialization and Vocational Day Services (Mode 10
Community Outreach Services (Mode 45) and Case Management Support (Mode 60)
24-hour Services
Residential & Other Supported Living Services (Mode 05)
State Hospital, IMD, & MH Rehabilitation Center Services (Mode 05)
Acute Inpatient (Mode 05)
Network (Fee-For-Service) (Mode 15)
Electroconvulsive Therapy
Evaluation & Management – Hospital Inpatient Services
Evaluation & Management – Nursing Facility
Evaluation & Management – Domiciliary, Board & Care, or Custodial Care Facility
Evaluation & Management – Office or Other Outpatient Service
Evaluation & Management – Outpatient Consultations
Evaluation & management – Inpatient Consultations
Community Partner (Mode 15)
Comprehensive Community Support
Never Billable Codes in IBHIS
Analiza porównawcza klasyfikacji procedur w USA i Polsce (rozporządzenie koszykowe) DOC
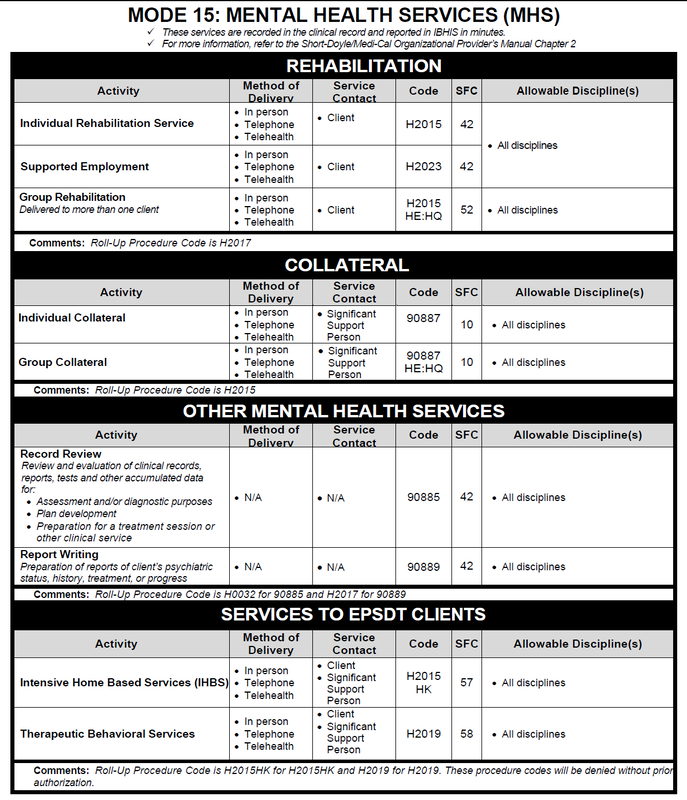
Dokument amerykański daje wyobrażenie, jak powinno wyglądać polskie rozporządzenie Ministra Zdrowia w sprawie świadczeń gwarantowanych w zakresie opieki psychiatrycznej opracowane do rozliczeń za ich wykonanie.
W Polsce i USA funkcjonuje podobny system finansowania ochrony zdrowia psychicznego według zasady „fee-for-service”, czyli refundacja za świadczenie. To jest rozwiązanie typowe dla ubezpieczeń społecznych. W odróżnieniu od Stanów Zjednoczonych w Polsce nie ma wolnego rynku ubezpieczeń zdrowotnych. Stąd wystarczy jedno zarządzenie prezesa NFZ do punktowej wyceny poszczególnych procedur z koszyka. Negocjacjom podlega jedynie stawka, wartość złotówkowa punktu lub osobodoby. Ponieważ w USA funkcjonuje wolny rynek ubezpieczeń zdrowotnych dlatego stworzono ogólnokrajowy katalog procedur z kodami, standardami czasowymi, uprawnione grupy zawodowe do ich wykonywania. Porównanie koszyka polskiego i amerykańskiego pozwala zauważyć pewne różnice, które pociągają za sobą określone konsekwencje.
1. Psychiatric Diagnostic Interview /psychiatryczny wywiad diagnostyczny/ może przeprowadzić każdy pracownik zdrowia psychicznego. Jeżeli rozumieć to jako rozmowę o problemach zdrowia psychicznego, z którymi ktoś zgłasza się do CZP na przykład w punkcie zgłoszeniowym, to oczywiste jest, że nie musi to być porada lekarska diagnostyczna lub tylko porada psychologiczna. Każdy profesjonalnie przygotowany do kontaktu terapeutycznego z pacjentem i jego rodziną może taką rozmowę przeprowadzić. W Polsce od początku reformy 1999 roku zawężono kontakt diagnostyczno-terapeutyczny do psychiatry i psychologa /psychoterapeuty/.
2. Psychiatric Diagnostic Interview with Medical Services – diagnostyczny wywiad psychiatryczny ze świadczeniem medycznym jest realizowany wyłącznie dla lekarzy. Tak więc dodanie „czynności medycznych” do wywiadu psychiatrycznego decyduje o wyłączności lekarskiej. To jest lekarska porada diagnostyczna w polskim wydaniu.
3. Plan Development – Plan Development A stand-alone Mental Health Service that includes developing Client Care Plans, approval of Client Care Plans and/or monitoring of a client’s progress. Plan development may be done as part of an interdisciplinary inter/intra-agency conference and/or consultation with other mental health providers in order to develop and/or monitor the client’s mental health treatment. Plan development may also be done as part of a contact with the client in order to develop and/or monitor the client’s mental health treatment.
Szczegółowy opis pokazuje, że plan terapii /opieki/ tworzony jest zespołowo. Do tego czasami konieczne jest zorganizowanie zebrania zebrania /konferencji, konsultacji przypadku/. Wiadomo, że specjaliści/terapeuci mogą komunikować się ze sobą za pomocą wpisów do dokumentacji medycznej. Jednakże w Polsce rozliczane są wyłącznie porady, wizyty, osobodni z udziałem pacjenta. Wszystkie inne czynności pod nieobecność pacjenta, tak jak zebranie zespołu ustalające plan terapii nie są refundowane. W modelu psychiatrii „mono-dyscyplinarnej” i „gabinetowej” plan terapii (farmakoterapia, psychoterapia) określa jednoosobowo lekarz lub psychoterapeuta. W terapii zaburzeń lękowych, nie psychotycznych, nie upośledzających funkcjonowanie społeczne to jest wystarczające. W polskich realiach nie było warunków do pracy zespołowej niezbędnej w modelu środowiskowym. W podejściu systemowym i otwartego dialogu indywidualny plan terapii/zdrowienia może być omawiany i uzgadniany w obecności pacjenta i jego rodziny. Jednakże powstaje problem, jak taką sesję terapeutyczną rozliczyć, czy jako poradę lekarską diagnostyczną, czy poradę psychologiczną, czy sesję terapii rodzinnej, czy sesję wsparcia psychospołecznego. Jakkolwiek rozliczyć taką procedurę, to w Polsce będzie ona nieopłacalna. Z praktyki wiadomo, że intensywny i wielodyscyplinarny kontakt terapeutyczny od początku kryzysu psychicznego z włączeniem rodziny i innych opiekunów przynosi efekty na dalszym etapie leczenia. Dopiero w pilotażowych Centrach Zdrowia Psychicznego istnieje szansa, że zostaną przywrócone normalne standardy opieki psychiatrycznej.
4. Collateral - Collateral (one or more clients represented) 1) Gathering information from family or significant support person(s) for the purpose of assessment. 2) Interpretation or explanation of results of psychiatric examinations or other accumulated data to family or other significant support person(s) 3)Providing services to family or significant support person(s) for the purpose of assisting the client in his/her mental health treatment (e.g., providing consultation or psychoeducation about client’s condition, teaching the family member or significant support person(s) skills that will improve the client’s mental health condition). 90887** A collateral/significant support person is, in the opinion of the client or the staff providing the service, a person who has or could have a significant role in the successful outcome of treatment, including, but not limited to, parent, spouse, or other relative, legal guardian or representative, or anyone living in the same household as the client. Agency staff, including Board & Care operators, are not collaterals.
Ta procedura nie ma odpowiednika w polskim koszyku, bo dotyczy osób innych niż pacjent, z którymi czasami trzeba się spotkać. Dorosły pacjent raczej powinien uczestniczyć w sesjach rodzinnych i sesjach wsparcia psychospołecznego, jednak nie zawsze to jest możliwe. W psychiatrii wieku rozwojowego takich sytuacji jest więcej, gdy dziecko nie uczestniczy w rozmowie terapeuty z rodzicami, na przykład dla omówienia spraw konfliktowych między nimi itp.
Szczególnie w psychiatrii dzieci i młodzieży – aktualna kategoryzacja procedur i sposób ich sprawozdawania do NFZ zniekształca rzeczywistość i ogranicza działania terapeutyczne. Z uwarunkowań prawnych wiadomo, że dziecko i nastolatek do osiągnięcia pełnoletności jest pacjentem ubezwłasnowolnionym. Rodzice lub opiekunowie prawni muszą wyrazić zgodę na leczenie. Od ukończenia szesnastego roku życia nastolatek co najwyżej może się nie zgodzić na terapię. W praktyce to rodzice najczęściej, prawie zawsze, rejestrują dzieci do psychiatry lub psychologa /psychoterapeuty/, a następnie przyprowadzają je do specjalisty. Lekarz lub psycholog prawie zawsze rozmawia z rodzicem lub rodzicami w trakcie lub po kontakcie z dzieckiem. To powinno być odnotowane w systemie – każdy uczestnik spotkania i opisany każdy kontakt. Dopiero wówczas uda się ocenić w jakich standardach prowadzona jest w Polsce ambulatoryjna opieka psychiatryczna dla dzieci i młodzieży, czemu tak mało jest sesji terapii rodzinnych.
5. Other no contact services -Review of Records Review of Records - Psychiatric evaluation of hospital records, other psychiatric reports, psychometric and/or projective tests, and other accumulated data for: Assessment and/or diagnostic purposes; Plan Development (development of client plans and services and/or monitoring a client’s progress) when not in the context of another service Note: All of these services are classified as Individual Mental Health Services and are reported under Service Function 42; When claiming for Review of Records, there must be clear documentation regarding how the information reviewed will inform the assessment, diagnosis and/or treatment plan.; No contact - Report Writing does not include activities such as writing letters to notify clients that their case will be closed (Przegląd dokumentacji medycznej w celach diagnostycznych oraz układanie lub monitorowanie IPZ)
6. Other no contact services - Report Writing No contact – Report Writing - Preparation of reports of client’s psychiatric status, history, treatment, or progress to other treating staff for care coordination when not part of another service Note: All of these services are classified as Individual Mental Health Services and are reported under Service Function 42; When claiming for Review of Records, there must be clear documentation regarding how the information reviewed will inform the assessment, diagnosis and/or treatment plan.; No contact - Report Writing does not include activities such as writing letters to notify clients that their case will be closed(bez kontaktu z pcjentem - pisanie dokumentacji medycznej)
Punkty 5 i 6 to inne czynności związane z opracowaniem i analizą dokumentacji medycznej. W Polsce nie wyodrębnia się tej czynności, zakładając, że porada zawiera prowadzenie dokumentacji medycznej. Wówczas należy się spodziewać, że specjalista będzie skracał czas kontaktu terapeutycznego z pacjentem w ramach standardu czasowego. W zarządzeniach prezesa NFZ oczywiście jest podane, że porady mają trwać co najmniej określony czas. Formalnie specjalista może poświęcić nieograniczoną ilość czasu, tyle że NFZ zapłaci jedynie za to minimum. W przypadku gdy terapeuta w sprawozdawczości podaje osobno czas kontaktu terapeutycznego i czas na czynności administracyjne możliwe jest dochowanie standardów.
7. Medication support - Comprehensive Medication Service - Medication Support Services to clients, collaterals, and/or other pertinent parties (e.g. PCP). Services may include: Prescription by phone, medication education by phone or in person, discussion of side effects by phone or in person, medication plan development by phone or in person, and medication group in person. /zalecanie i edukacja o lekach także przez telefon/ farmakoterapia jest jednoznacznie skategoryzowana, jako medication support. W dalszych szczegółowych opisach podano, że za edukację dotyczącą zażywania leków odpowiada lekarz, ewentualnie pielęgniarka./
8. Rehabilitation Service - Individual Rehabilitation Service: Service delivered to one client to provide assistance in improving, maintaining, or restoring the client’s functional, daily living, social and leisure, grooming and personal hygiene, or meal preparation skills, or his/her support resources. CCR §1810.243. /Indywidualne świadczenie rehabilitacyjne – kojarzy się z terapią środowiskową/
9. Group Rehabilitation (family and non-family) Service delivered to more than one client at the same time to provide assistance in improving, maintaining, or restoring his/her support resources or his/her functional skills - daily living, social and leisure, grooming and personal hygiene, or meal preparation. /grupowa rehabilitacja kojarzy się z oddziałem dziennym/
10. Rehabilitation Service - Psychoeducation to Non-Client, Non-Collateral Rehabilitation Service - Psychoeducation to Non-Client, Non-Collateral: Providing services to non-clients, non-collaterals (e.g., school teachers) for the purpose of assisting the client in his/her mental health treatment (e.g., providing consultation or psychoeducation about client’s condition, teaching the non-client, non-collateral person skills that will improve the client’s mental health condition).
Psychoedukacja dla pracowników instytucji np. nauczyciele, którzy nie są pacjentami, ani ich bliskimi. Sesja wsparcia psychospołecznego nie odnosi się do takiej sytuacji. W psychiatrii dzieci i młodzieży to jest potrzebna procedura /czynność/, której brakuje w polskim koszyku. W Polsce koszyk został upleciony w paradygmacie medycznym – leczenie to działania lekarza/terapeuty adresowane do pacjenta. W medycynie zabiegowej i somatycznej to się sprawdza. W psychiatrii, gdzie w standardach światowych obowiązuje model bio-psycho-społeczny, taka zawężenie rozumienia świadczeń medycznych/pomocowych wypacza opiekę psychiatryczną.
Należy dodać, że rehabilitacja jest prowadzona przez wszystkich pracowników zdrowia psychicznego.
11. On-going support to maintain employment (This service requires the client be currently employed, paid or unpaid; school is not considered employment.)
Ta procedura wskazuje na obowiązek troski o utrzymanie zatrudnienia przez pacjenta, w okresie gdy jest w opiece psychiatrycznej.
Pełny przegląd amerykańskiego katalogu procedur wskazuje na to, że został on opracowany z myślą skategoryzowania wszelkich niezbędnych czynności związanych z opieką psychiatryczną w różnych formach. Można tam znaleźć wiele innych różnić w stosunku do Polski, które prowokują do zastanowienia, czemu u nas jest właśnie tak, jak jest. Bez oceny, gdzie jest lepiej. Tak po prostu, dla zrozumienia skąd i po co jest to co jest. Amerykańska klasyfikacja procedur /czynności/ sprawia wrażenie, że jest zupełna. Uwzględnia zarówno kontakt twarzą w twarz i za pomocą telefonu, Internetu.
Czy każda procedura jest wyceniona? Tego nie wiem na pewno. To jest do sprawdzenia. Jednak wątpię. Prawdopodobnie wyceniony jest czas pracy danego specjalisty odpowiednio do kwalifikacji. W sprawozdaniu wpisuje się kod danej procedury i określa ile czasu to zajęło. To jest podstawą do rozliczenia usługi.
Transforming Mental Health Care in the United States
The U.S. mental health system has reached a moment (2021) when a historic transformation to address persistent problems appears realistic. These problems include high levels of unmet need for care, underdevelopment of community-based supports that can help avoid unnecessary emergency care or police engagement, and disparities in access and quality of services.
Amerykański system zdrowia psychicznego osiągnął moment (2021), w którym nastąpił historyczny transformacja mająca na celu rozwiązanie utrzymujących się problemów wydaje się realistyczna. Problemy te obejmują wysoki poziom niezaspokojonej potrzeby opieki, niedorozwój wsparcia środowiskowego, które może pomóc uniknąć niepotrzebnej opieki w nagłych wypadkach lub zaangażowania policji, a także różnic w dostępie i jakość usług.
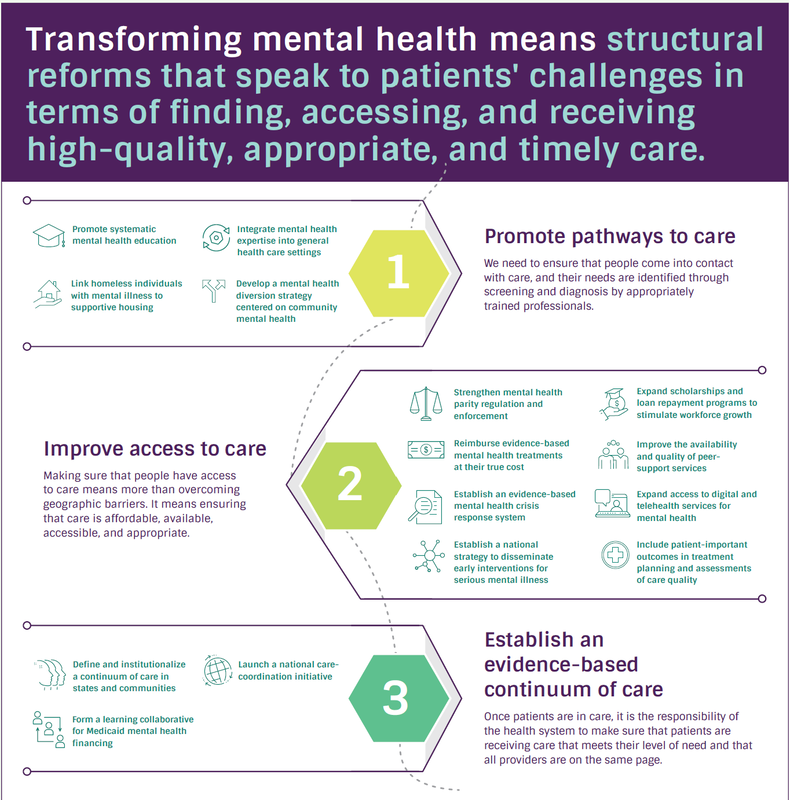
1. Promote pathways to care. Too often, people with mental health needs do not even make contact with mental health providers. This is partly attributable to a system in which individuals are unaware of available resources, fear the repercussions and stigma associated with mental illness, and fail to receive screenings and diagnoses. High-need populations, such as those with a pattern of homelessness or criminal justice involvement, may also require shepherding to services that best meet their needs.
2. Improve access to care. Once a patient is identified as needing care, several barriers may obstruct actual receipt of services. These include the cost to the consumer (affordability), the capacity of the system to provide adequate care in a timely manner (availability), the location
of services (accessibility), and the suitability of services from the consumer’s perspective(appropriateness). All four barriers must be removed for patients to use services.
3. Establish an evidence-based continuum of care. Once patients are inside the system, uncertainty remains. Will the care be evidence-based? Will it correspond to the patient’s level of need? Will it be provided in a timely and consistent manner? There is no guarantee that mental health systems can answer “yes” to these questions and, ultimately, improve patient outcomes. For this to happen, the internal mechanics of systems need to be recalibrated, and rewards need to be established to align services with patient needs.
Tłumaczenie Google
1. Promuj ścieżki opieki. Zbyt często osoby z potrzebami w zakresie zdrowia psychicznego nawet nie kontaktują się z dostawcami usług w zakresie zdrowia psychicznego. Częściowo można to przypisać systemowi, w którym jednostki nie są świadome dostępnych zasobów, obawiają się konsekwencji i piętna związanego z chorobą psychiczną oraz nie poddają się badaniom przesiewowym i diagnozom. Populacje o wysokich potrzebach, takie jak bezdomne lub zaangażowane w wymiar sprawiedliwości w sprawach karnych, mogą również wymagać kierowania do usług, które najlepiej odpowiadają ich potrzebom.
2. Poprawić dostęp do opieki. Gdy pacjent zostanie zidentyfikowany jako wymagający opieki, kilka barier może utrudniać faktyczne otrzymanie usług. Obejmują one koszt dla konsumenta (przystępność cenowa), zdolność systemu do zapewnienia odpowiedniej opieki w odpowiednim czasie (dostępność), lokalizację usług (dostępność) oraz przydatność usług z punktu widzenia konsumenta (właściwość). Wszystkie cztery bariery muszą zostać usunięte, aby pacjenci mogli korzystać z usług.
3. Ustanowienie ciągłości opieki opartej na dowodach. Gdy pacjenci znajdą się w systemie, niepewność pozostaje. Czy opieka będzie oparta na dowodach? Czy będzie odpowiadać poziomowi potrzeb pacjenta? Czy będzie świadczona w sposób terminowy i spójny? Nie ma gwarancji, że systemy zdrowia psychicznego mogą odpowiedzieć „tak” na te pytania i ostatecznie poprawić wyniki leczenia pacjentów. Aby tak się stało, wewnętrzna mechanika systemów musi zostać ponownie skalibrowana, a finansowanie musi mieć na celu dostosowanie świadczeń do potrzeb pacjentów.
The U.S. mental health system has reached a moment (2021) when a historic transformation to address persistent problems appears realistic. These problems include high levels of unmet need for care, underdevelopment of community-based supports that can help avoid unnecessary emergency care or police engagement, and disparities in access and quality of services.
Amerykański system zdrowia psychicznego osiągnął moment (2021), w którym nastąpił historyczny transformacja mająca na celu rozwiązanie utrzymujących się problemów wydaje się realistyczna. Problemy te obejmują wysoki poziom niezaspokojonej potrzeby opieki, niedorozwój wsparcia środowiskowego, które może pomóc uniknąć niepotrzebnej opieki w nagłych wypadkach lub zaangażowania policji, a także różnic w dostępie i jakość usług.
1. Promote pathways to care. Too often, people with mental health needs do not even make contact with mental health providers. This is partly attributable to a system in which individuals are unaware of available resources, fear the repercussions and stigma associated with mental illness, and fail to receive screenings and diagnoses. High-need populations, such as those with a pattern of homelessness or criminal justice involvement, may also require shepherding to services that best meet their needs.
2. Improve access to care. Once a patient is identified as needing care, several barriers may obstruct actual receipt of services. These include the cost to the consumer (affordability), the capacity of the system to provide adequate care in a timely manner (availability), the location
of services (accessibility), and the suitability of services from the consumer’s perspective(appropriateness). All four barriers must be removed for patients to use services.
3. Establish an evidence-based continuum of care. Once patients are inside the system, uncertainty remains. Will the care be evidence-based? Will it correspond to the patient’s level of need? Will it be provided in a timely and consistent manner? There is no guarantee that mental health systems can answer “yes” to these questions and, ultimately, improve patient outcomes. For this to happen, the internal mechanics of systems need to be recalibrated, and rewards need to be established to align services with patient needs.
Tłumaczenie Google
1. Promuj ścieżki opieki. Zbyt często osoby z potrzebami w zakresie zdrowia psychicznego nawet nie kontaktują się z dostawcami usług w zakresie zdrowia psychicznego. Częściowo można to przypisać systemowi, w którym jednostki nie są świadome dostępnych zasobów, obawiają się konsekwencji i piętna związanego z chorobą psychiczną oraz nie poddają się badaniom przesiewowym i diagnozom. Populacje o wysokich potrzebach, takie jak bezdomne lub zaangażowane w wymiar sprawiedliwości w sprawach karnych, mogą również wymagać kierowania do usług, które najlepiej odpowiadają ich potrzebom.
2. Poprawić dostęp do opieki. Gdy pacjent zostanie zidentyfikowany jako wymagający opieki, kilka barier może utrudniać faktyczne otrzymanie usług. Obejmują one koszt dla konsumenta (przystępność cenowa), zdolność systemu do zapewnienia odpowiedniej opieki w odpowiednim czasie (dostępność), lokalizację usług (dostępność) oraz przydatność usług z punktu widzenia konsumenta (właściwość). Wszystkie cztery bariery muszą zostać usunięte, aby pacjenci mogli korzystać z usług.
3. Ustanowienie ciągłości opieki opartej na dowodach. Gdy pacjenci znajdą się w systemie, niepewność pozostaje. Czy opieka będzie oparta na dowodach? Czy będzie odpowiadać poziomowi potrzeb pacjenta? Czy będzie świadczona w sposób terminowy i spójny? Nie ma gwarancji, że systemy zdrowia psychicznego mogą odpowiedzieć „tak” na te pytania i ostatecznie poprawić wyniki leczenia pacjentów. Aby tak się stało, wewnętrzna mechanika systemów musi zostać ponownie skalibrowana, a finansowanie musi mieć na celu dostosowanie świadczeń do potrzeb pacjentów.
SYSTEM UBEZPIECZENIOWY W USA I JEGO KONSEKWENCJE DLA PACJENTA I SPECJALISTY – NADZÓR UBEZPIECZALNI
Na koniec ciekawostka z USA. Jeżeli ktokolwiek narzeka na NFZ, to niech przeczyta poniższy dodatek o tym co się dzieje w Ameryce. Zapewniam, że po lekturze będzie szczęśliwy, że nasz swojski płatnik publiczny ma jeszcze daleko do poziomu amerykańskiego. W tej Ameryce to strach być pacjentem oraz lekarzem – nigdy nie wiesz, czy cię będą leczyć oraz czy ci zapłacą... W polskiej opiece psychiatrycznej jest zupełnie inaczej: świadczeniobiorca nie jest pewien, czy leczenie służy zdrowieniu, a świadczeniodawca nie jest pewien, czy po tym, jak mu zapłacą, to mu nie zabiorą...
Poniższy tekst w tłumaczeniu Google, z drobnymi korektami DB.
Understanding Health Insurance / Zrozumienie ubezpieczenia zdrowotnego
https://www-nami-org.translate.goog/Your-Journey/Individuals-with-Mental-Illness/Understanding-Health-Insurance?_x_tr_sl=ru&_x_tr_tl=pl&_x_tr_hl=pl&_x_tr_pto=wapp
Ubezpieczenie jest kluczowym narzędziem, które może zapewnić dostęp do leczenia potrzebnego do wyzdrowienia. Ubezpieczenie zdrowotne pomaga opłacić potrzeby w zakresie zdrowia psychicznego, w tym badania kontrolne, wizyty u specjalistów, opiekę w nagłych wypadkach i pobyty w szpitalu. W większości przypadków ubezpieczenie powstrzyma osobę od pokrycia pełnych kosztów usług medycznych.
Ubezpieczenie lub przeglądanie aktualnego planu ubezpieczeniowego może wydawać się skomplikowane, ale znajomość podstaw może pomóc w pomyślnym poruszaniu się po systemie.
Rodzaje ubezpieczenia zdrowotnegoZrozumienie różnic w planach ubezpieczenia zdrowotnego może pomóc osobie w podjęciu świadomej decyzji o tym, który plan jest odpowiedni i jakie opcje są dostępne. Poziom zasięgu i dostępności usług oraz specjalistów ds. zdrowia psychicznego zależy od rodzaju wybranego planu.
Typowe rodzaje ubezpieczeń zdrowotnych obejmują:
Przeczytaj więcej o tych opcjach ubezpieczenia, które mogą być dostępne na naszej stronie poświęconej rodzajom ubezpieczenia zdrowotnego .
Ile ubezpieczenia potrzebuje ktoś?Każda osoba jest inna i nie każdy potrzebuje takiej samej sumy ubezpieczenia. Czynnikiem ograniczającym dla wielu osób jest koszt planu. Ale dana osoba powinna upewnić się, że ma jak największe pokrycie pieniędzy, które wydaje.
Niezależnie od tego, czy wybierasz ubezpieczenie po raz pierwszy, czy oceniasz obecny plan, oto kilka rzeczy, o których należy pamiętać:
https://www-nami-org.translate.goog/Your-Journey/Living-with-a-Mental-Health-Condition/Understanding-Health-Insurance/What-to-Do-If-You-re-Denied-Care-By-Your-Insurance?_x_tr_sl=ru&_x_tr_tl=pl&_x_tr_hl=pl&_x_tr_pto=wapp
Zakłady ubezpieczeń zdrowotnych mogą odmówić leczenia choroby psychicznej z wielu powodów i przy użyciu różnych metod, które określają, czy dany rodzaj leczenia jest uznawany za medycznie konieczny, czy też jest częścią świadczeń w pakiecie ubezpieczeniowym.
Jeśli masz prawo do określonej usługi lub wsparcia, masz prawo odwołać się od decyzji firmy ubezpieczeniowej. Wiele osób może otrzymać potrzebną im opiekę po złożeniu odwołania. Jeśli uważasz, że odmówiono ci opieki w sposób niesprawiedliwy, istnieją przepisy federalne i stanowe, które pomogą ci się chronić.
Zrozumienie warunków ubezpieczeniaOdmowa potrzebnej usługi lub leczenia w zakresie zdrowia psychicznego może być frustrującym procesem. Częścią tego stresującego czasu są mylące terminy stosowane przez firmy ubezpieczeniowe. Poniżej znajdują się definicje niektórych z najczęstszych terminów używanych w przypadku odmowy świadczenia usług zdrowotnych.
Poniżej znajdują się sygnały wskazujące, że możesz mieć podstawy do odwołania się od decyzji podjętej w ramach planu zdrowotnego zgodnie z prawem parytetowym.
Powszechnie odmawiane rodzaje opiekiNiektóre rodzaje usług leczenia w zakresie zdrowia psychicznego są odrzucane po wyższych stawkach niż w przypadku innych schorzeń. Jeśli odmówiono Ci następujących świadczeń i usług, a uważasz, że masz do nich prawo w ramach planu zdrowotnego, możesz rozważyć złożenie odwołania.
Federalne Centrum Usług Medicaid i Medicare (CMS) może również egzekwować parytet, jeśli stany nie egzekwują prawa. Jeśli masz obawy, że Twój plan ubezpieczeniowy nie jest zgodny z parytetem, skontaktuj się z linią pomocy CMS pod numerem 1-877-267-2323, wewnętrzny 6-1565.
Jeśli masz plan samoubezpieczenia — plan, w którym pracodawca przyjmuje ryzyko finansowe związane z zapewnieniem świadczeń opieki zdrowotnej swoim pracownikom — Departament Pracy Stanów Zjednoczonych (DOL) ma prawo egzekwować parytet. Aby dowiedzieć się więcej, zadzwoń pod bezpłatny numer DOL pod numer 1-866-444-3272 lub skontaktuj się z doradcą ds. świadczeń w jednym z biur regionalnych DOL .
Jeśli masz plan zdrowotny w ramach Medicare lub Medicaid, istnieją różne procedury odwoławcze. Skontaktuj się ze swoim planem, aby uzyskać szczegółowe informacje.
How to Prepare for an Insurance Treatment Review / Jak przygotować się do przeglądu leczenia ubezpieczeniowego
(w tłumaczeniu Google)
25 czerwca 2019
https://www.icanotes.com/2019/06/25/how-to-prepare-for-an-insurance-treatment-review/
Jako specjalista ds. zdrowia behawioralnego chcesz zapewnić swoim klientom najlepszą opiekę i nie musieć ograniczać ich opieki ze względu na kwestie ubezpieczeniowe. To zrozumiałe, jeśli czujesz się przytłoczony oczekującą weryfikacją, ale istnieją sposoby, aby przejąć kontrolę nad sytuacją. Jeśli wiesz, jak przygotować się do przeglądu leczenia, będziesz gotowy bronić opieki nad swoim klientem, abyś mógł kontynuować leczenie zgodnie z planem - ze spokojem. Jest wiele informacji na temat recenzji leczenia ubezpieczeniowego i mnóstwo pytań, które należy zadać. W tym poście odpowiemy na często zadawane pytania, pokażemy, jak przygotować się do przeglądu ubezpieczenia i udzielimy wskazówek, jak radzić sobie z odrzuceniem roszczenia.
Spis treści
Przegląd leczenia, zwany także przeglądem wykorzystania, ma miejsce wtedy, gdy firma ubezpieczeniowa kontaktuje się z terapeutą lub innym dostawcą opieki behawioralnej, aby zadać mu pytania dotyczące leczenia klienta. Celem recenzenta jest ustalenie, czy leczenie jest konieczne z medycznego punktu widzenia i czy stanowi część akceptowalnego i skutecznego planu leczenia. Ubezpieczyciel zdecyduje następnie, czy będzie nadal zwracał koszty behawioralnych usług zdrowotnych objętych przeglądem. W większości przypadków, zwłaszcza w przypadku usług w zakresie zdrowia psychicznego, przegląd jest standardowym oczekiwaniem i jest rutynowo planowany na określone dni/godziny (w przypadku kontaktu telefonicznego) i przypada w określonych terminach (w przypadku korzystania z poczty elektronicznej) w ramach tego konkretnego cyklu leczenia, a to został zorganizowany przez członka personelu (telefoniczny/elektroniczny) nawiązywania pierwszego kontaktu w celu ustalenia, czy dana osoba jest tam w celu wykonania usług, oraz powodu, dla którego muszą tam być.
Często zadawane pytania dotyczące recenzji leczenia zdrowia psychicznego
Recenzje leczenia mogą wydawać się zniechęcające, jeśli nie wiesz, czego się spodziewać lub jak się przygotować. Przyjrzyjmy się często zadawanym pytaniom dotyczącym przeglądów ubezpieczeń i różnych rodzajów planów, dzięki czemu będziesz lepiej przygotowany do mówienia językiem ubezpieczycieli.
1. Kto określa konieczność medyczną?
Chociaż rządy federalne i stanowe tworzą pewne wytyczne, których muszą przestrzegać firmy ubezpieczeniowe, w przeciwnym razie ubezpieczyciel decyduje, co jest uważane za konieczność medyczną. Jeśli firma ubezpieczeniowa zdecyduje, że usługa nie jest konieczna z medycznego punktu widzenia, może odrzucić roszczenie.
2. Co służy do określenia konieczności medycznej?
Kryteria konieczności medycznej różnią się w zależności od polityki. Jednak niektóre usługi są zwykle uważane za konieczne lub niepotrzebne z medycznego punktu widzenia. Na przykład Medicare definiuje medycznie niezbędne usługi lub materiały potrzebne do zdiagnozowania lub leczenia stanu, który spełnia „akceptowane standardy medycyny”. Jednak Medicare nie obejmuje usług zbędnych z medycznego punktu widzenia, takich jak:
Prywatni ubezpieczyciele mogą ustalać własne kryteria, o ile przestrzegają stanowych i federalnych przepisów dotyczących opieki zdrowotnej. Na przykład Aetna wymienia następujące kryteria konieczności medycznej dla planów organizacji utrzymania zdrowia (HMO):
3. Czym różni się przegląd od wniosku o rejestrację?
Twoja praktyka może otrzymywać listy od firm ubezpieczeniowych z prośbą o dokumentację pacjenta. Mogą nazwać żądanie rekordu audytem korekty ryzyka lub gromadzeniem danych. Centers for Medicare and Medicaid Services (CMS) stosuje audyty korekty ryzyka w celu określenia odpowiednich składek. Ogólnie rzecz biorąc, celem wniosku o rejestrację jest ustalenie stanu zdrowia beneficjentów, aby ubezpieczyciele mogli określić, gdzie przelać środki. Prośba o dokumentację nie dotyczy określenia konieczności medycznej ani przeglądu planów leczenia. W przypadku prośby o rejestrację możesz zadzwonić do ubezpieczyciela i zapytać dokładnie, czego potrzebują do gromadzenia danych i sprawdzić stanowe przepisy dotyczące udostępniania rekordów. Nie ma potrzeby publikowania prywatnych notatek z psychoterapii .
4. Czym różni się przegląd od audytu?
Podczas gdy przegląd leczenia koncentruje się na konieczności i skuteczności planu leczenia twojego klienta, audyt zwykle przegląda dokumentację, aby potwierdzić, że przestrzegasz wymagań dotyczących dokumentacji planu ubezpieczeniowego. Firmy ubezpieczeniowe często losowo wybierają świadczeniodawców do przeglądania wykresów i innych form dokumentacji. Audyt nie ma nic wspólnego z oceną skuteczności Twojego leczenia. Możesz uzyskać listę wymagań dokumentacyjnych dla dowolnego planu ubezpieczeniowego, który udostępniasz, aby zawsze być przygotowanym na wyrywkowy audyt.
5. Czym jest izba rozliczeniowa w opiece zdrowotnej?
Mówiąc najprościej, izba rozliczeniowa opieki zdrowotnej odgrywa rolę pośrednika między Twoją praktyką a ubezpieczycielem. Kiedy jesteś gotowy do złożenia wniosku o zwrot kosztów, możesz złożyć wniosek do izby rozrachunkowej, a nie bezpośrednio do ubezpieczyciela. Izba rozliczeniowa sprawdzi błędy, aby upewnić się, że wniosek zostanie zaakceptowany. Współpraca z izbą rozliczeniową może poprawić wydajność i uprościć proces rozliczeniowy.
6. Umowa z opłatą za usługę vs. Kapitalizacja: jaka jest różnica?
Plan opłaty za usługę (FFS Fee-For-Service) to tradycyjny plan ubezpieczeniowy, w którym ubezpieczyciel płaci bezpośrednio lekarzowi lub innemu podmiotowi świadczącemu opiekę zdrowotną lub zwraca klientowi koszty po złożeniu przez niego roszczenia. Z drugiej strony kapitalizacja obejmuje stałe miesięczne płatności uzgodnione w umowie między świadczeniodawcą a firmą ubezpieczeniową. W przypadku umowy kapitacyjnej lekarz otrzymuje uzgodnione płatności na pacjenta objętego planem zdrowotnym. Opłaty ustalane są z rocznym wyprzedzeniem i pozostają takie same przez cały rok, bez względu na to, jak często pacjent korzysta z usług. Kapitalizacja pomaga towarzystwom ubezpieczeń zdrowotnych kontrolować koszty, zniechęcając lekarzy do zapewniania większej opieki niż to konieczne. Główną korzyścią dla lekarzy jest mniej prowadzenia księgowości i brak konieczności oczekiwania na zwrot kosztów.
7. Opłata za usługę vs. Oparte na wartości: jaka jest różnica?
Opieka zdrowotna oparta na wartościach ma miejsce wtedy, gdy lekarze są wynagradzani na podstawie wyników leczenia pacjentów . Dlatego dostawcy są nagradzani za pomaganie pacjentom w prowadzeniu zdrowszego i szczęśliwszego życia. Opieka oparta na wartości różni się zarówno od podejścia kapitałowego, jak i FFS, ponieważ koncentruje się bardziej na jakości opieki niż na ilości. Ten typ modelu ma na celu zapewnienie niższych kosztów i lepszych wyników dla pacjentów, wyższą satysfakcję pacjentów dla świadczeniodawców i zdrowszą populację z mniejszą liczbą zgłoszeń.
Plany zdrowotne w Stanach Zjednoczonych coraz częściej odchodzą od tradycyjnego systemu płatności za usługę (ang. fee-for-service) w kierunku modelu opieki opartej na wartości (ang. value-based care), który w swoim założeniu powinien prowadzić do zwiększenia jakości usług, a nie ich ilości. Podobne zmiany obserwuje się w rodzaju płatności za usługi z zakresu zdrowia psychicznego. Świadczeniodawcy w związku z wprowadzanymi zmianami stają się odpowiedzialni za jakość, wynki i całkowity koszt opieki. Podstawą wprowadzenia opieki opartej na wartości powinno być określenie przez płatnika odpowiednich skal i miar zawartych w umowach o płatności, które dostosowują zwrot kosztów świadczeniodawcy w oparciu o wyniki w zakresie zdrowia psychicznego.
Na koniec ciekawostka z USA. Jeżeli ktokolwiek narzeka na NFZ, to niech przeczyta poniższy dodatek o tym co się dzieje w Ameryce. Zapewniam, że po lekturze będzie szczęśliwy, że nasz swojski płatnik publiczny ma jeszcze daleko do poziomu amerykańskiego. W tej Ameryce to strach być pacjentem oraz lekarzem – nigdy nie wiesz, czy cię będą leczyć oraz czy ci zapłacą... W polskiej opiece psychiatrycznej jest zupełnie inaczej: świadczeniobiorca nie jest pewien, czy leczenie służy zdrowieniu, a świadczeniodawca nie jest pewien, czy po tym, jak mu zapłacą, to mu nie zabiorą...
Poniższy tekst w tłumaczeniu Google, z drobnymi korektami DB.
Understanding Health Insurance / Zrozumienie ubezpieczenia zdrowotnego
https://www-nami-org.translate.goog/Your-Journey/Individuals-with-Mental-Illness/Understanding-Health-Insurance?_x_tr_sl=ru&_x_tr_tl=pl&_x_tr_hl=pl&_x_tr_pto=wapp
Ubezpieczenie jest kluczowym narzędziem, które może zapewnić dostęp do leczenia potrzebnego do wyzdrowienia. Ubezpieczenie zdrowotne pomaga opłacić potrzeby w zakresie zdrowia psychicznego, w tym badania kontrolne, wizyty u specjalistów, opiekę w nagłych wypadkach i pobyty w szpitalu. W większości przypadków ubezpieczenie powstrzyma osobę od pokrycia pełnych kosztów usług medycznych.
Ubezpieczenie lub przeglądanie aktualnego planu ubezpieczeniowego może wydawać się skomplikowane, ale znajomość podstaw może pomóc w pomyślnym poruszaniu się po systemie.
Rodzaje ubezpieczenia zdrowotnegoZrozumienie różnic w planach ubezpieczenia zdrowotnego może pomóc osobie w podjęciu świadomej decyzji o tym, który plan jest odpowiedni i jakie opcje są dostępne. Poziom zasięgu i dostępności usług oraz specjalistów ds. zdrowia psychicznego zależy od rodzaju wybranego planu.
Typowe rodzaje ubezpieczeń zdrowotnych obejmują:
- Prywatne ubezpieczenie zdrowotne
- pomoc medyczna
- opieka medyczna
- ŻETON
- Opieka zdrowotna TRICARE i VA
Przeczytaj więcej o tych opcjach ubezpieczenia, które mogą być dostępne na naszej stronie poświęconej rodzajom ubezpieczenia zdrowotnego .
Ile ubezpieczenia potrzebuje ktoś?Każda osoba jest inna i nie każdy potrzebuje takiej samej sumy ubezpieczenia. Czynnikiem ograniczającym dla wielu osób jest koszt planu. Ale dana osoba powinna upewnić się, że ma jak największe pokrycie pieniędzy, które wydaje.
Niezależnie od tego, czy wybierasz ubezpieczenie po raz pierwszy, czy oceniasz obecny plan, oto kilka rzeczy, o których należy pamiętać:
- Przystępność cenowa. Porównaj miesięczne składki, odliczenia, współpłacenie i/lub współubezpieczenie, aby upewnić się, że otrzymujesz najlepszą ofertę dla swoich potrzeb w zakresie ubezpieczenia zdrowotnego. Zastanów się nie tylko nad tym, ile płacisz miesięcznie, ale także ile pieniędzy potrzebujesz na opłacenie współpłacenia i współubezpieczenia.
- Dostępność specjalistów zdrowia psychicznego. Upewnij się, że w sieci dostawców planu zdrowotnego znajduje się szeroka gama specjalistów ds. zdrowia psychicznego. Niektórzy specjaliści ds. zdrowia psychicznego nie biorą ubezpieczenia, więc sprawdź, za co plan ubezpieczeniowy pokryje dostawców sieci.
- Ubezpieczenie leków na receptę. Jeśli dana osoba znalazła odpowiedni lek do leczenia swojej choroby, powinna znaleźć plan obejmujący ten lek w celu utrzymania dobrego samopoczucia.
- Ograniczenia liczby wizyt lekarskich związanych ze zdrowiem psychicznym. Niektóre plany zdrowotne nakładają ograniczenia na liczbę wizyt w gabinecie w celu na przykład terapii. Wybierz plan, który pozwala na wymaganą liczbę wizyt. W zależności od potrzeb danej osoby może być konieczne rozważenie różnic w zakresie opieki szpitalnej i ambulatoryjnej.
https://www-nami-org.translate.goog/Your-Journey/Living-with-a-Mental-Health-Condition/Understanding-Health-Insurance/What-to-Do-If-You-re-Denied-Care-By-Your-Insurance?_x_tr_sl=ru&_x_tr_tl=pl&_x_tr_hl=pl&_x_tr_pto=wapp
Zakłady ubezpieczeń zdrowotnych mogą odmówić leczenia choroby psychicznej z wielu powodów i przy użyciu różnych metod, które określają, czy dany rodzaj leczenia jest uznawany za medycznie konieczny, czy też jest częścią świadczeń w pakiecie ubezpieczeniowym.
Jeśli masz prawo do określonej usługi lub wsparcia, masz prawo odwołać się od decyzji firmy ubezpieczeniowej. Wiele osób może otrzymać potrzebną im opiekę po złożeniu odwołania. Jeśli uważasz, że odmówiono ci opieki w sposób niesprawiedliwy, istnieją przepisy federalne i stanowe, które pomogą ci się chronić.
Zrozumienie warunków ubezpieczeniaOdmowa potrzebnej usługi lub leczenia w zakresie zdrowia psychicznego może być frustrującym procesem. Częścią tego stresującego czasu są mylące terminy stosowane przez firmy ubezpieczeniowe. Poniżej znajdują się definicje niektórych z najczęstszych terminów używanych w przypadku odmowy świadczenia usług zdrowotnych.
- Kryteria konieczności medycznej to standardy stosowane w planach zdrowotnych do decydowania, czy leczenie lub środki ochrony zdrowia zalecane przez twojego dostawcę usług w zakresie zdrowia psychicznego są rozsądne, konieczne i odpowiednie. Jeśli plan zdrowotny zdecyduje, że leczenie spełnia te standardy, wówczas żądana opieka jest uważana za niezbędną z medycznego punktu widzenia.
- Przegląd wykorzystania , znany również jako zarządzanie wykorzystaniem, to proces stosowany przez ubezpieczycieli do decydowania, czy żądana opieka w zakresie zdrowia psychicznego jest medycznie konieczna, skuteczna i zgodna z przyjętą praktyką medyczną . Zgodnie z przyjętą praktyką medyczną oznacza, że skuteczność leczenia lub usługi w zakresie zdrowia psychicznego została udowodniona w oparciu o dowody naukowe.
- Uprzednia autoryzacja , znana również jako wstępna akceptacja, wstępna autoryzacja, wstępna akceptacja lub wstępna certyfikacja, jest rodzajem przeglądu wykorzystania i polega na tym, że Ty lub Twój dostawca usług musicie poprosić o zatwierdzenie, zanim Twój plan zdrowotny wyrazi zgodę na opłacenie usługi, planu leczenia lub lek na receptę.
- Terapia krokowa to rodzaj uprzedniej zgody, w ramach której musisz wypróbować tańszy lek na receptę lub usługę, zanim będziesz mógł przejść na droższą receptę lub usługę.
Poniżej znajdują się sygnały wskazujące, że możesz mieć podstawy do odwołania się od decyzji podjętej w ramach planu zdrowotnego zgodnie z prawem parytetowym.
- Wyższe koszty lub mniej wizyt w przypadku usług w zakresie zdrowia psychicznego niż w przypadku innych rodzajów opieki zdrowotnej.
- Konieczność zadzwonienia i uzyskania pozwolenia na objęcie opieką zdrowia psychicznego, ale nie w przypadku innych rodzajów opieki zdrowotnej.
- Odmowa świadczenia usług w zakresie zdrowia psychicznego, ponieważ nie uznano ich za konieczne z medycznego punktu widzenia, ale plan nie odpowiada na prośbę o kryteria konieczności medycznej, których używają.
- Niemożność znalezienia w sieci świadczeniodawców zdrowia psychicznego, którzy przyjmują nowych pacjentów, ale można znaleźć świadczeniodawców innej opieki zdrowotnej.
- Plan zdrowotny nie obejmuje stacjonarnego zdrowia psychicznego ani leczenia uzależnień ani intensywnej opieki ambulatoryjnej, ale dotyczy innych schorzeń.
Powszechnie odmawiane rodzaje opiekiNiektóre rodzaje usług leczenia w zakresie zdrowia psychicznego są odrzucane po wyższych stawkach niż w przypadku innych schorzeń. Jeśli odmówiono Ci następujących świadczeń i usług, a uważasz, że masz do nich prawo w ramach planu zdrowotnego, możesz rozważyć złożenie odwołania.
- Stacjonarne leczenie chorób psychicznych
- Średnie poziomy opieki, takie jak intensywne leczenie ambulatoryjne, rehabilitacja psychologiczna, częściowa hospitalizacja i asertywne leczenie środowiskowe (ACT)
- Interwencje diagnostyczne i terapeutyczne w gabinecie, takie jak oceny diagnostyczne, standardowe testy, takie jak Kwestionariusz Zdrowia Pacjenta 9 (PHQ-9), który mierzy depresję, oraz inne usługi, takie jak psychoterapia
Federalne Centrum Usług Medicaid i Medicare (CMS) może również egzekwować parytet, jeśli stany nie egzekwują prawa. Jeśli masz obawy, że Twój plan ubezpieczeniowy nie jest zgodny z parytetem, skontaktuj się z linią pomocy CMS pod numerem 1-877-267-2323, wewnętrzny 6-1565.
Jeśli masz plan samoubezpieczenia — plan, w którym pracodawca przyjmuje ryzyko finansowe związane z zapewnieniem świadczeń opieki zdrowotnej swoim pracownikom — Departament Pracy Stanów Zjednoczonych (DOL) ma prawo egzekwować parytet. Aby dowiedzieć się więcej, zadzwoń pod bezpłatny numer DOL pod numer 1-866-444-3272 lub skontaktuj się z doradcą ds. świadczeń w jednym z biur regionalnych DOL .
Jeśli masz plan zdrowotny w ramach Medicare lub Medicaid, istnieją różne procedury odwoławcze. Skontaktuj się ze swoim planem, aby uzyskać szczegółowe informacje.
How to Prepare for an Insurance Treatment Review / Jak przygotować się do przeglądu leczenia ubezpieczeniowego
(w tłumaczeniu Google)
25 czerwca 2019
https://www.icanotes.com/2019/06/25/how-to-prepare-for-an-insurance-treatment-review/
Jako specjalista ds. zdrowia behawioralnego chcesz zapewnić swoim klientom najlepszą opiekę i nie musieć ograniczać ich opieki ze względu na kwestie ubezpieczeniowe. To zrozumiałe, jeśli czujesz się przytłoczony oczekującą weryfikacją, ale istnieją sposoby, aby przejąć kontrolę nad sytuacją. Jeśli wiesz, jak przygotować się do przeglądu leczenia, będziesz gotowy bronić opieki nad swoim klientem, abyś mógł kontynuować leczenie zgodnie z planem - ze spokojem. Jest wiele informacji na temat recenzji leczenia ubezpieczeniowego i mnóstwo pytań, które należy zadać. W tym poście odpowiemy na często zadawane pytania, pokażemy, jak przygotować się do przeglądu ubezpieczenia i udzielimy wskazówek, jak radzić sobie z odrzuceniem roszczenia.
Spis treści
- Co to jest przegląd leczenia ubezpieczeniowego?
- Często zadawane pytania dotyczące recenzji leczenia zdrowia psychicznego
- Przygotowanie do przeglądu leczenia
- Poruszanie się po przeglądzie leczenia
- Co mogę zrobić, jeśli moja firma ubezpieczeniowa odrzuci moje roszczenie o zwrot kosztów?
- Jak walczyć z odrzuceniem roszczenia ubezpieczeniowego?
Przegląd leczenia, zwany także przeglądem wykorzystania, ma miejsce wtedy, gdy firma ubezpieczeniowa kontaktuje się z terapeutą lub innym dostawcą opieki behawioralnej, aby zadać mu pytania dotyczące leczenia klienta. Celem recenzenta jest ustalenie, czy leczenie jest konieczne z medycznego punktu widzenia i czy stanowi część akceptowalnego i skutecznego planu leczenia. Ubezpieczyciel zdecyduje następnie, czy będzie nadal zwracał koszty behawioralnych usług zdrowotnych objętych przeglądem. W większości przypadków, zwłaszcza w przypadku usług w zakresie zdrowia psychicznego, przegląd jest standardowym oczekiwaniem i jest rutynowo planowany na określone dni/godziny (w przypadku kontaktu telefonicznego) i przypada w określonych terminach (w przypadku korzystania z poczty elektronicznej) w ramach tego konkretnego cyklu leczenia, a to został zorganizowany przez członka personelu (telefoniczny/elektroniczny) nawiązywania pierwszego kontaktu w celu ustalenia, czy dana osoba jest tam w celu wykonania usług, oraz powodu, dla którego muszą tam być.
Często zadawane pytania dotyczące recenzji leczenia zdrowia psychicznego
Recenzje leczenia mogą wydawać się zniechęcające, jeśli nie wiesz, czego się spodziewać lub jak się przygotować. Przyjrzyjmy się często zadawanym pytaniom dotyczącym przeglądów ubezpieczeń i różnych rodzajów planów, dzięki czemu będziesz lepiej przygotowany do mówienia językiem ubezpieczycieli.
1. Kto określa konieczność medyczną?
Chociaż rządy federalne i stanowe tworzą pewne wytyczne, których muszą przestrzegać firmy ubezpieczeniowe, w przeciwnym razie ubezpieczyciel decyduje, co jest uważane za konieczność medyczną. Jeśli firma ubezpieczeniowa zdecyduje, że usługa nie jest konieczna z medycznego punktu widzenia, może odrzucić roszczenie.
2. Co służy do określenia konieczności medycznej?
Kryteria konieczności medycznej różnią się w zależności od polityki. Jednak niektóre usługi są zwykle uważane za konieczne lub niepotrzebne z medycznego punktu widzenia. Na przykład Medicare definiuje medycznie niezbędne usługi lub materiały potrzebne do zdiagnozowania lub leczenia stanu, który spełnia „akceptowane standardy medycyny”. Jednak Medicare nie obejmuje usług zbędnych z medycznego punktu widzenia, takich jak:
- Usługi oceny i zarządzania wykraczające poza te uznane za niezbędne z medycznego punktu widzenia
- Nadmierna terapia lub procedury diagnostyczne
- Egzaminy, testy przesiewowe i terapie, które nie odnoszą się do objawów klienta
Prywatni ubezpieczyciele mogą ustalać własne kryteria, o ile przestrzegają stanowych i federalnych przepisów dotyczących opieki zdrowotnej. Na przykład Aetna wymienia następujące kryteria konieczności medycznej dla planów organizacji utrzymania zdrowia (HMO):
- Usługa świadczona jest zgodnie z ogólnie przyjętymi standardami praktyki lekarskiej.
- Usługa jest klinicznie odpowiednia pod względem rodzaju, częstotliwości, zakresu i czasu trwania.
- Usługa nie służy przede wszystkim wygodzie pacjenta lub usługodawcy.
- Usługa nie jest droższa niż usługa alternatywna.
3. Czym różni się przegląd od wniosku o rejestrację?
Twoja praktyka może otrzymywać listy od firm ubezpieczeniowych z prośbą o dokumentację pacjenta. Mogą nazwać żądanie rekordu audytem korekty ryzyka lub gromadzeniem danych. Centers for Medicare and Medicaid Services (CMS) stosuje audyty korekty ryzyka w celu określenia odpowiednich składek. Ogólnie rzecz biorąc, celem wniosku o rejestrację jest ustalenie stanu zdrowia beneficjentów, aby ubezpieczyciele mogli określić, gdzie przelać środki. Prośba o dokumentację nie dotyczy określenia konieczności medycznej ani przeglądu planów leczenia. W przypadku prośby o rejestrację możesz zadzwonić do ubezpieczyciela i zapytać dokładnie, czego potrzebują do gromadzenia danych i sprawdzić stanowe przepisy dotyczące udostępniania rekordów. Nie ma potrzeby publikowania prywatnych notatek z psychoterapii .
4. Czym różni się przegląd od audytu?
Podczas gdy przegląd leczenia koncentruje się na konieczności i skuteczności planu leczenia twojego klienta, audyt zwykle przegląda dokumentację, aby potwierdzić, że przestrzegasz wymagań dotyczących dokumentacji planu ubezpieczeniowego. Firmy ubezpieczeniowe często losowo wybierają świadczeniodawców do przeglądania wykresów i innych form dokumentacji. Audyt nie ma nic wspólnego z oceną skuteczności Twojego leczenia. Możesz uzyskać listę wymagań dokumentacyjnych dla dowolnego planu ubezpieczeniowego, który udostępniasz, aby zawsze być przygotowanym na wyrywkowy audyt.
5. Czym jest izba rozliczeniowa w opiece zdrowotnej?
Mówiąc najprościej, izba rozliczeniowa opieki zdrowotnej odgrywa rolę pośrednika między Twoją praktyką a ubezpieczycielem. Kiedy jesteś gotowy do złożenia wniosku o zwrot kosztów, możesz złożyć wniosek do izby rozrachunkowej, a nie bezpośrednio do ubezpieczyciela. Izba rozliczeniowa sprawdzi błędy, aby upewnić się, że wniosek zostanie zaakceptowany. Współpraca z izbą rozliczeniową może poprawić wydajność i uprościć proces rozliczeniowy.
6. Umowa z opłatą za usługę vs. Kapitalizacja: jaka jest różnica?
Plan opłaty za usługę (FFS Fee-For-Service) to tradycyjny plan ubezpieczeniowy, w którym ubezpieczyciel płaci bezpośrednio lekarzowi lub innemu podmiotowi świadczącemu opiekę zdrowotną lub zwraca klientowi koszty po złożeniu przez niego roszczenia. Z drugiej strony kapitalizacja obejmuje stałe miesięczne płatności uzgodnione w umowie między świadczeniodawcą a firmą ubezpieczeniową. W przypadku umowy kapitacyjnej lekarz otrzymuje uzgodnione płatności na pacjenta objętego planem zdrowotnym. Opłaty ustalane są z rocznym wyprzedzeniem i pozostają takie same przez cały rok, bez względu na to, jak często pacjent korzysta z usług. Kapitalizacja pomaga towarzystwom ubezpieczeń zdrowotnych kontrolować koszty, zniechęcając lekarzy do zapewniania większej opieki niż to konieczne. Główną korzyścią dla lekarzy jest mniej prowadzenia księgowości i brak konieczności oczekiwania na zwrot kosztów.
7. Opłata za usługę vs. Oparte na wartości: jaka jest różnica?
Opieka zdrowotna oparta na wartościach ma miejsce wtedy, gdy lekarze są wynagradzani na podstawie wyników leczenia pacjentów . Dlatego dostawcy są nagradzani za pomaganie pacjentom w prowadzeniu zdrowszego i szczęśliwszego życia. Opieka oparta na wartości różni się zarówno od podejścia kapitałowego, jak i FFS, ponieważ koncentruje się bardziej na jakości opieki niż na ilości. Ten typ modelu ma na celu zapewnienie niższych kosztów i lepszych wyników dla pacjentów, wyższą satysfakcję pacjentów dla świadczeniodawców i zdrowszą populację z mniejszą liczbą zgłoszeń.
Plany zdrowotne w Stanach Zjednoczonych coraz częściej odchodzą od tradycyjnego systemu płatności za usługę (ang. fee-for-service) w kierunku modelu opieki opartej na wartości (ang. value-based care), który w swoim założeniu powinien prowadzić do zwiększenia jakości usług, a nie ich ilości. Podobne zmiany obserwuje się w rodzaju płatności za usługi z zakresu zdrowia psychicznego. Świadczeniodawcy w związku z wprowadzanymi zmianami stają się odpowiedzialni za jakość, wynki i całkowity koszt opieki. Podstawą wprowadzenia opieki opartej na wartości powinno być określenie przez płatnika odpowiednich skal i miar zawartych w umowach o płatności, które dostosowują zwrot kosztów świadczeniodawcy w oparciu o wyniki w zakresie zdrowia psychicznego.
TRANSFORMING MENTAL HAELTH CARE IN THE UNITED STATES
by Ryan K. McBain, Nicole K. Eberhart, Joshua Breslau, Lori Frank, M. Audrey Burnam, Vishnupriya Kareddy, Molly M. Simmons
RAND Corporation, 2021
https://www.rand.org/pubs/research_briefs/RBA889-1.html
The U.S. mental health system has reached a moment when a historic transformation to address persistent problems appears realistic. These problems include high levels of unmet need for care, underdevelopment of community-based supports that can help avoid unnecessary emergency care or police engagement, and disparities in access and quality of services.
Reforming the U.S. mental health system has received strong bipartisan support at both the federal and state levels.Against this background, a RAND research team sought to identify goals for transforming the U.S. mental health care system and to pinpoint opportunities to drive systemic improvements. To develop these recommendations, the team interviewed mental health experts throughout the country—including government officials, public administrators, health system executives, and academicians. In parallel, the team conducted a comprehensive review of the scientific literature to identify best practices and recent innovations in mental health care.
The overarching goals of these recommendations appear below.
Goals for a Mental Health System Centered on the Patient Journey
1. Finding a doorway to care: promote pathways to care
Too often, people with mental health needs do not even make contact with mental health providers. This is partly attributable to a system in which individuals are unaware of available resources, fear the repercussions and stigma associated with mental illness, and fail to receive screenings and diagnoses. High-need populations, such as those with a pattern of homelessness or criminal justice involvement, may also require shepherding to services that best meet their needs.
2. Getting through the door: improve access to care
Once a patient is identified as needing care, several barriers may obstruct actual receipt of services. These include the cost to the consumer (affordability), the capacity of the system to provide adequate care in a timely manner (availability), the location of services (accessibility), and the suitability of services from the consumer's perspective (appropriateness). All four barriers must be removed for patients to use services.
3. Once you're inside: establish an evidence-based continuum of care
Once patients are inside the system, uncertainty remains. Will the care be evidence-based? Will it correspond to the patient's level of need? Will it be provided in a timely and consistent manner? There is no guarantee that mental health systems can answer "yes" to these questions and, ultimately, improve patient outcomes. For this to happen, the internal mechanics of systems need to be recalibrated, and rewards need to be established to align services with patient needs.
With these three goals as a framework, the team recommends 15 strategies for transforming mental health care in the United States into a patient-centered system.
Goal 1: Promote Pathways to Care
We need to ensure that people come into contact with care, and their needs are identified through screening and diagnosis by appropriately trained professionals.
Making sure that people have access to care means more than overcoming geographic barriers. It means ensuring that care is affordable, available, accessible, and appropriate.
Goal 3: Establish a Continuum of Evidence-Based Care
Once patients are in care, it is the responsibility of the health system to make sure that patients are receiving care that meets their level of need and that all providers are on the same page.
by Ryan K. McBain, Nicole K. Eberhart, Joshua Breslau, Lori Frank, M. Audrey Burnam, Vishnupriya Kareddy, Molly M. Simmons
RAND Corporation, 2021
https://www.rand.org/pubs/research_briefs/RBA889-1.html
The U.S. mental health system has reached a moment when a historic transformation to address persistent problems appears realistic. These problems include high levels of unmet need for care, underdevelopment of community-based supports that can help avoid unnecessary emergency care or police engagement, and disparities in access and quality of services.
Reforming the U.S. mental health system has received strong bipartisan support at both the federal and state levels.Against this background, a RAND research team sought to identify goals for transforming the U.S. mental health care system and to pinpoint opportunities to drive systemic improvements. To develop these recommendations, the team interviewed mental health experts throughout the country—including government officials, public administrators, health system executives, and academicians. In parallel, the team conducted a comprehensive review of the scientific literature to identify best practices and recent innovations in mental health care.
The overarching goals of these recommendations appear below.
Goals for a Mental Health System Centered on the Patient Journey
1. Finding a doorway to care: promote pathways to care
Too often, people with mental health needs do not even make contact with mental health providers. This is partly attributable to a system in which individuals are unaware of available resources, fear the repercussions and stigma associated with mental illness, and fail to receive screenings and diagnoses. High-need populations, such as those with a pattern of homelessness or criminal justice involvement, may also require shepherding to services that best meet their needs.
2. Getting through the door: improve access to care
Once a patient is identified as needing care, several barriers may obstruct actual receipt of services. These include the cost to the consumer (affordability), the capacity of the system to provide adequate care in a timely manner (availability), the location of services (accessibility), and the suitability of services from the consumer's perspective (appropriateness). All four barriers must be removed for patients to use services.
3. Once you're inside: establish an evidence-based continuum of care
Once patients are inside the system, uncertainty remains. Will the care be evidence-based? Will it correspond to the patient's level of need? Will it be provided in a timely and consistent manner? There is no guarantee that mental health systems can answer "yes" to these questions and, ultimately, improve patient outcomes. For this to happen, the internal mechanics of systems need to be recalibrated, and rewards need to be established to align services with patient needs.
With these three goals as a framework, the team recommends 15 strategies for transforming mental health care in the United States into a patient-centered system.
Goal 1: Promote Pathways to Care
We need to ensure that people come into contact with care, and their needs are identified through screening and diagnosis by appropriately trained professionals.
- Promote systematic mental health education. Mental health education should be considered a key part of a comprehensive health education curriculum. Schools have the potential to destigmatize mental health and improve attitudes, enhance the knowledge and skills needed for prevention, and promote increased help-seeking.
- Integrate mental health expertise into general health care settings. Mental health conditions are often unrecognized in general health care settings. Integrated, whole-person care approaches are effective in connecting people to care but are underutilized.
- Link homeless individuals with mental illness to supportive housing. Supportive housing programs help homeless people with mental health needs begin recovery by starting from a foundation of stable housing. Stable housing not only improves individuals' quality of life and chances for recovery; it can also save the health care system money by reducing the need for recurring care. Administrators at all levels of government should expand supportive housing programs, particularly for individuals with serious mental illness.
- Develop a mental health diversion strategy centered on community mental health. Correctional facilities are one of the largest providers of mental health care in the United States. Yet, in this setting, many with mental health conditions might not receive the care they need. An evidence-based program that diverts people away from the criminal justice system and into community-based mental health services would benefit this population.
Making sure that people have access to care means more than overcoming geographic barriers. It means ensuring that care is affordable, available, accessible, and appropriate.
- Strengthen mental health parity regulation and enforcement. Although mandated by law, mental health parity has still not been fully achieved. Governments can institute laws and regulations that set clear standards for assessing parity compliance, require mental health coverage from a broader range of insurance plans, and strengthen enforcement of existing state and federal parity laws.
- Reimburse evidence-based mental health treatments at their true cost. Establishing Medicaid reimbursement rates that are commensurate with the costs of providing care should encourage providers to offer evidence-based treatments that now are often unavailable. Improving access within Medicaid would particularly benefit Americans with low incomes and those with serious mental illnesses.
- Establish an evidence-based mental health crisis response system. Many communities lack an adequate mental health crisis response system. Poor crisis care results in missed opportunities to direct individuals into treatment and sometimes ends in suicide that might have been prevented. Building an evidence-based response system that swiftly identifies individual mental health needs and efficiently triages individuals into appropriate care should reduce unnecessary suffering.
- Establish a national strategy to finance and disseminate evidence-based early interventions for serious mental illness. Growing evidence points to the effectiveness of programs that deliver coordinated clinical and supportive services early in the course of schizophrenia and related disorders. These programs, as well as emerging early interventions for serious mental illnesses, fall outside the Medicaid-based public mental health system and require a national strategy to fund and disseminate them widely.
- Expand scholarships and loan repayment programs to stimulate workforce growth. Expanding the recruitment pipeline for mental health specialty workers, such as psychiatrists and psychologists, will help meet the needs of underserved areas. Policies for doing this include expanding scholarship, fellowship, and loan forgiveness programs that attract more individuals, support more-diverse students, and require a commitment to practicing in high-need settings.
- Improve the availability and quality of peer-support services. Peer-support specialists are people who have experienced mental health or substance use problems and have been trained to join teams caring for those struggling with mental health conditions, psychological trauma, or substance use disorders. These specialists have been proven highly effective in improving patient outcomes. Expanding access to training, credentialing, and reimbursement for peer support has the potential to improve access to high-quality peer-support care.
- Expand access to digital and telehealth services for mental health. Digital and telehealth services can extend access to mental health care throughout the United States, particularly in rural communities that face shortages of providers. Stimulated by the COVID-19 pandemic, state and federal policymakers should codify expansion of these services by ensuring that insurers cover them, that clinicians are adequately reimbursed, and that consumers know how to use the technologies.
- Include patient-important outcomes in treatment planning and assessments of care quality. The current system is seldom organized to deliver patient-centered care or to provide access to the full range of community supportive services. As a result, provider-based goals often misalign with patient-based goals. Including patient outcomes, such as social functioning and occupational goals, in care planning can improve this alignment and enhance the patient-centeredness of mental health care.
Goal 3: Establish a Continuum of Evidence-Based Care
Once patients are in care, it is the responsibility of the health system to make sure that patients are receiving care that meets their level of need and that all providers are on the same page.
- Define and institutionalize a continuum of care in states and communities. Individuals with mental health needs often fall through the cracks because of a lack of clarity regarding who should provide care, at what level of intensity, and in what settings over time. Available clinical guidelines provide an explicit framework for resolving these questions about level of care and can help optimize mental health spending within communities. State Medicaid systems should mandate their use.
- Launch a national care-coordination initiative. Care coordination involves integrating mental health providers, care managers, and other providers into coordinated teams, often in primary care settings. The effectiveness of coordination has been demonstrated in various evidence-based models, but few practices are using it. A national initiative led by the Centers for Medicare & Medicaid Services that provides technical assistance, implementation tools, and learning support for implementing practices would help transition practices to evidence-based models.
- Form a learning collaborative for Medicaid mental health financing. Collaborations between Medicaid officials, advocates, and state policymakers can help ensure that emerging evidence on innovative financing and service delivery models drive improvement in mental health care systems, especially for Americans with low incomes or serious mental illness.
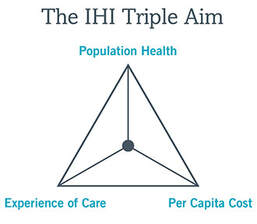
THE TRIPLE AIM
The Triple Aim is a framework developed by the Institute for Healthcare Improvement (IHI) in 2007. Its purpose is to assist healthcare systems in optimizing performance by addressing three key areas:
The Triple Aim is a framework developed by the Institute for Healthcare Improvement (IHI) in 2007. Its purpose is to assist healthcare systems in optimizing performance by addressing three key areas:
- Improving patient experience: The goal is to enhance the overall experience patients have when interacting with the healthcare system. This involves assessing community health, identifying areas of risk, and implementing initiatives to improve communication between providers. Examples include electronic health records (EHR), accountable care organizations (ACOs), and patient-centered care coordination teams.
- Reducing the per capita costs of health care: The United States has the most expensive healthcare system globally, accounting for 17% of the GDP. The Triple Aim aims to increase the quality of care while decreasing costs. Achieving this balance is essential for sustainable healthcare.
- Improving the health of populations overall: Healthcare organizations should consider the unique needs of their communities and identify at-risk populations. By measuring progress and tracking impact, they can work toward better population health beyond hospitals and clinics.
TRIPLE AIM STRATEGIES TO IMPROVE BEHAVIORAL HEALTH CARE
Americal Hospital Association, 2016
The Triple Aim And BehAviorAl heAlTh Effectively addressing behavioral health issues in the community calls for hospitals and health systems to:
1) integrate behavioral and physical health care services;
2) build networks or partnerships with community stakeholders—other hospitals or health systems, clinics, social service agencies, and local and state organizations—to coordinate care; and
3) implement alternative payment models to sustain needed services. This approach aligns with the Triple Aim to improve the patient experience of care, improve the health of populations and reduce the per capita cost of health care.
Americal Hospital Association, 2016
The Triple Aim And BehAviorAl heAlTh Effectively addressing behavioral health issues in the community calls for hospitals and health systems to:
1) integrate behavioral and physical health care services;
2) build networks or partnerships with community stakeholders—other hospitals or health systems, clinics, social service agencies, and local and state organizations—to coordinate care; and
3) implement alternative payment models to sustain needed services. This approach aligns with the Triple Aim to improve the patient experience of care, improve the health of populations and reduce the per capita cost of health care.
IMPROVE THE PATIENT EXPERIENCE OF CARE:
Integrate behavioral and physical health care services
Despite the high rate of comorbidities among people with behavioral health disorders, behavioral health care historically has been separated from physical health care, with minimal coordination of care. This fragmentation of the health care system can lead to ineffective, disjointed and redundant care, as well as gaps in care.
Unaddressed behavioral health issues can lead to unnecessary emergency department visits and uncontrolled chronic diseases, increasing the cost of care.
True behavioral and physical health integration is the preferred model of care to achieve the best outcomes. Coordinated care and co-located care, while positive, are less desirable and often achieve suboptimal outcomes, which can frustrate providers.
STAGES OF BEHAVIORAL HEALTH INTEGRATION
COORDINATED - Behavioral and physical health clinicians prectice separately within their respective systems. Information regarding mutual patients may be exchanged as needed, and collaboration is limited outside of initial referral.
CO-LOCATED - Behavioral and physical health clinicians deliver care in the same practice. Co-location is more of a description of where services are provided rather than a specific service. Patient care is often still siloed to each clinician's area of expertise.
INTEGRATED - Behavioral and physical health clinicians work together to design and implement a patient care plan. Tightly integrated, on-site teamwork with a unified care plan. Often connotes close organizational integration as well, perhaps involving social and other services.
IMPROVE THE HEALTH OF POPULATIONS:
Build Networks or Partnerships with Community Stakeholders to Coordinate Care
For hospitals and health systems, an important element in integrating and improving access to behavioral health services is building community networks and partnerships to decrease care fragmentation and address gaps in care.
Examples of networks and partnerships include:
Action steps
Recommended steps to start the work toward aligning efforts and building community networks or partnerships to improve behavioral health include:
1. Bring together community stakeholders to work toward one goal of improving behavioral health and overall health.
Establish a strategic mission and vision for health shared by all the community partners so that all partners have a sense of ownership. Conducting a community health needs assessment that includes survey questions about behavioral health issues will help the stakeholders identify and prioritize health needs.
2. Involve a variety of community stakeholders as partners. It is important to recognize the quality of the community partners and what strengths each partner brings to the table to align toward the vision and goals. Stakeholders may include primary care providers, pediatricians, emergency medical personnel, law enforcement agencies, community mental health agencies, housing authority agencies, homeless shelters, patients, family members, community members, independent mental health providers, relevant state agencies, local businesses, rural health clinics, federally qualified health clinics, peer counselors, local NAMI (National Association of Mental Illness) chapters, United Way, Salvation Army, schools and universities.
3. Ensure the engagement and participation of patients and their families.
4. Get buy-in as well as mutual investment by community partners, at a level appropriate for each partner’s size. Investment can include in-kind services, staffing, facility resources as well as financial and other types of support. Clarify the roles and responsibilities of each partner.
5. Develop a multiyear, multiorganization plan that is updated biennially to address community needs. This plan describes
the strategic mission and vision and identifies potential barriers and opportunities unique to the community.
6. Focus on the data. Collect and report behavioral health metrics related to quality of care and patient access. At hospitals and health systems, multidisciplinary teams may need to help customize the electronic health record system for behavioral health. Clinicians can use registries and data tracking tools to manage the care of patients with chronic diseases, and to monitor screening and health maintenance activities.
Metrics
To evaluate the effectiveness of community networks and partnerships established to integrate and improve behavioral health care and achieve the Triple Aim, the participating organizations and the network or partnership should track specific measures, such as:
REDUCE THE PER CAPITA COST OF HEALTH CARE:
Implement Alternative Payment Models to Sustain Needed Services
Delivering better integrated behavioral health care can be impeded by policies that may separate the payment of physical and behavioral health services. Separate payment structures compel some providers to operate within professional silos. Behavioral health interventions in an integrated model can reduce costs and readmissions. Savings from reduced costs could be accrued and reapplied to behavioral health to support providers’ services. An integrated model focuses on total value across the care continuum, across any setting. Care should be integrated not only within health care settings but also with community partners, to provide the best care in the right setting at the best value.
Payment reform
The current health care payment model—fee for service—is becoming outdated as government entities, payers, consumers and providers move to value-based payment models. Hospitals and health systems will need to adapt and deploy a variety of payment models that best fit within the structure of their organization. New payment methods can assist in better financing and sustaining integrated behavioral health care. For example, many health care organizations bundle payments for specific illnesses or episodes of care. Others are moving toward global payment models for primary care that could include behavioral health. Improving care, reducing costs. Research studies confirm that an integrated care model that includes behavioral health has a significantly positive effect on the patient’s health and reduces the total cost of care. Examples of integrated models are accountable care organizations, community care organizations, integrated delivery systems, clinically integrated networks and patient-centered medical homes. These models raise the quality of care and reduce costs, and they also include some form of a global or capitated payment system that allows a hospital or health system to recover costs, given reductions in the use of more expensive services.
Health care providers and payers can work toward structuring medical care payment policy to promote behavioral health interventions, linking with supportive resources and organizations in the community and rewarding efforts to improve population health. Financial incentives also may be tied to promoting healthy behaviors and community initiatives. Future guides may address strategies and recommendations and highlight case studies about these topics.
Conclusion
The rapidly changing health care field demands a well-coordinated, accessible, affordable and accountable system for providing quality care to patients. By integrating behavioral and physical health care services, building networks or partnerships with community stakeholders to coordinate patient care and implementing alternative payment models to sustain needed
services, hospitals and health systems can achieve the Triple Aim. All these efforts will improve the patient experience of care, improve population health and reduce per capita cost.
Integrate behavioral and physical health care services
Despite the high rate of comorbidities among people with behavioral health disorders, behavioral health care historically has been separated from physical health care, with minimal coordination of care. This fragmentation of the health care system can lead to ineffective, disjointed and redundant care, as well as gaps in care.
Unaddressed behavioral health issues can lead to unnecessary emergency department visits and uncontrolled chronic diseases, increasing the cost of care.
True behavioral and physical health integration is the preferred model of care to achieve the best outcomes. Coordinated care and co-located care, while positive, are less desirable and often achieve suboptimal outcomes, which can frustrate providers.
STAGES OF BEHAVIORAL HEALTH INTEGRATION
COORDINATED - Behavioral and physical health clinicians prectice separately within their respective systems. Information regarding mutual patients may be exchanged as needed, and collaboration is limited outside of initial referral.
CO-LOCATED - Behavioral and physical health clinicians deliver care in the same practice. Co-location is more of a description of where services are provided rather than a specific service. Patient care is often still siloed to each clinician's area of expertise.
INTEGRATED - Behavioral and physical health clinicians work together to design and implement a patient care plan. Tightly integrated, on-site teamwork with a unified care plan. Often connotes close organizational integration as well, perhaps involving social and other services.
IMPROVE THE HEALTH OF POPULATIONS:
Build Networks or Partnerships with Community Stakeholders to Coordinate Care
For hospitals and health systems, an important element in integrating and improving access to behavioral health services is building community networks and partnerships to decrease care fragmentation and address gaps in care.
Examples of networks and partnerships include:
- Coordination with local organizations and stakeholders
- Collaboration in a structured network with many community stakeholders
- Contractual affiliations, such as joint ventures
Action steps
Recommended steps to start the work toward aligning efforts and building community networks or partnerships to improve behavioral health include:
1. Bring together community stakeholders to work toward one goal of improving behavioral health and overall health.
Establish a strategic mission and vision for health shared by all the community partners so that all partners have a sense of ownership. Conducting a community health needs assessment that includes survey questions about behavioral health issues will help the stakeholders identify and prioritize health needs.
2. Involve a variety of community stakeholders as partners. It is important to recognize the quality of the community partners and what strengths each partner brings to the table to align toward the vision and goals. Stakeholders may include primary care providers, pediatricians, emergency medical personnel, law enforcement agencies, community mental health agencies, housing authority agencies, homeless shelters, patients, family members, community members, independent mental health providers, relevant state agencies, local businesses, rural health clinics, federally qualified health clinics, peer counselors, local NAMI (National Association of Mental Illness) chapters, United Way, Salvation Army, schools and universities.
3. Ensure the engagement and participation of patients and their families.
4. Get buy-in as well as mutual investment by community partners, at a level appropriate for each partner’s size. Investment can include in-kind services, staffing, facility resources as well as financial and other types of support. Clarify the roles and responsibilities of each partner.
5. Develop a multiyear, multiorganization plan that is updated biennially to address community needs. This plan describes
the strategic mission and vision and identifies potential barriers and opportunities unique to the community.
6. Focus on the data. Collect and report behavioral health metrics related to quality of care and patient access. At hospitals and health systems, multidisciplinary teams may need to help customize the electronic health record system for behavioral health. Clinicians can use registries and data tracking tools to manage the care of patients with chronic diseases, and to monitor screening and health maintenance activities.
Metrics
To evaluate the effectiveness of community networks and partnerships established to integrate and improve behavioral health care and achieve the Triple Aim, the participating organizations and the network or partnership should track specific measures, such as:
- Number of patients referred from a hospital and successfully connected with treatment in the community
- Increase in percentage of patients who keep their initial, scheduled appointment »
- Percentage of patients screened for depression and Screening, Brief Intervention, and Referral to Treatment (SBIRT) is an evidence-based practice used to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol and illicit drugs – and referred to treatment if needed
- Percentage of patients not improving that received case review and psychiatric recommendations and referral to
- psychiatric services, and received same
- Percentage of patients not improving who are referred to and treated by a specialty behavior health provider
- Reduction in total number of psychiatric emergency department visits by people with a primary psychiatric/addiction disorder and by those with physical health disorders and comorbid behavioral health disorders
- Reduction of inpatient days after admission to a community mental health center intensive outpatient program, residential treatment center, partial hospitalization program or other appropriate post-acute treatment services
- Reduction in six-month hospital readmissions of patients with a primary psychiatric/addiction disorder and by those with physical health disorders and comorbid behavioral health disorders
- Patient improvement on the Global Assessment of Functioning scale at oneyear follow-up appointment
- Return on investment, based on average Medicaid claim cost savings per patient annually for all health care services
REDUCE THE PER CAPITA COST OF HEALTH CARE:
Implement Alternative Payment Models to Sustain Needed Services
Delivering better integrated behavioral health care can be impeded by policies that may separate the payment of physical and behavioral health services. Separate payment structures compel some providers to operate within professional silos. Behavioral health interventions in an integrated model can reduce costs and readmissions. Savings from reduced costs could be accrued and reapplied to behavioral health to support providers’ services. An integrated model focuses on total value across the care continuum, across any setting. Care should be integrated not only within health care settings but also with community partners, to provide the best care in the right setting at the best value.
Payment reform
The current health care payment model—fee for service—is becoming outdated as government entities, payers, consumers and providers move to value-based payment models. Hospitals and health systems will need to adapt and deploy a variety of payment models that best fit within the structure of their organization. New payment methods can assist in better financing and sustaining integrated behavioral health care. For example, many health care organizations bundle payments for specific illnesses or episodes of care. Others are moving toward global payment models for primary care that could include behavioral health. Improving care, reducing costs. Research studies confirm that an integrated care model that includes behavioral health has a significantly positive effect on the patient’s health and reduces the total cost of care. Examples of integrated models are accountable care organizations, community care organizations, integrated delivery systems, clinically integrated networks and patient-centered medical homes. These models raise the quality of care and reduce costs, and they also include some form of a global or capitated payment system that allows a hospital or health system to recover costs, given reductions in the use of more expensive services.
Health care providers and payers can work toward structuring medical care payment policy to promote behavioral health interventions, linking with supportive resources and organizations in the community and rewarding efforts to improve population health. Financial incentives also may be tied to promoting healthy behaviors and community initiatives. Future guides may address strategies and recommendations and highlight case studies about these topics.
Conclusion
The rapidly changing health care field demands a well-coordinated, accessible, affordable and accountable system for providing quality care to patients. By integrating behavioral and physical health care services, building networks or partnerships with community stakeholders to coordinate patient care and implementing alternative payment models to sustain needed
services, hospitals and health systems can achieve the Triple Aim. All these efforts will improve the patient experience of care, improve population health and reduce per capita cost.
Medicaid Data Show Wide Differences in Mental Health Care in the United States
March 23, 2023
K. John McConnell, Ph.D. , and colleagues at Oregon Health and Science University examined data from millions of Americans aged 19–64 years enrolled in Medicaid in 2018. The study represents the first extensive use of a new database of national Medicaid claims, known as the Transformed Medicaid Statistical Information System Analytic Files , designed to provide reliable, deidentified data for research purposes.
Medicaid claims showed variations in rates of emergency department visits for mental health conditions between states and between economic areas within states. For instance, the state with the most emergency department visits had almost five times more visits than the state with the fewest visits. Similarly, within many states, there was a wide range between the economic areas with the highest and lowest number of emergency department visits.
There was also large geographic variation in outpatient mental health visits, which were positively, but only moderately, correlated with emergency department visits. In general, economic areas with high rates of emergency department visits also had high rates of outpatient care. However, there were also areas with high rates of emergency department visits but low outpatient mental health visits, and vice versa. Frequent use of emergency services for mental health treatment might reflect a high degree of need in those areas and, in the absence of available outpatient care, a high degree of unmet need.
As a final step, the researchers compared emergency department visits for certain types of mental health conditions:
Together, the findings highlight the nationwide use of emergency departments for mental health care, while emphasizing wide variations in rates of use between states and between mental disorders. The frequent use of emergency services for mental health care shown in this study might, in some cases, indicate a high degree of unmet need or a lack of access to outpatient mental health services.
Regional differences in Medicaid recipients’ mental health care experiences also demonstrate the importance of tailoring strategies to specific populations. The authors emphasize the need for context-specific, local solutions, which might start with looking at how mental health benefits are administered by state Medicaid agencies, determining the availability of local mental health providers, or identifying the most common types of mental disorders in communities.
March 23, 2023
K. John McConnell, Ph.D. , and colleagues at Oregon Health and Science University examined data from millions of Americans aged 19–64 years enrolled in Medicaid in 2018. The study represents the first extensive use of a new database of national Medicaid claims, known as the Transformed Medicaid Statistical Information System Analytic Files , designed to provide reliable, deidentified data for research purposes.
Medicaid claims showed variations in rates of emergency department visits for mental health conditions between states and between economic areas within states. For instance, the state with the most emergency department visits had almost five times more visits than the state with the fewest visits. Similarly, within many states, there was a wide range between the economic areas with the highest and lowest number of emergency department visits.
There was also large geographic variation in outpatient mental health visits, which were positively, but only moderately, correlated with emergency department visits. In general, economic areas with high rates of emergency department visits also had high rates of outpatient care. However, there were also areas with high rates of emergency department visits but low outpatient mental health visits, and vice versa. Frequent use of emergency services for mental health treatment might reflect a high degree of need in those areas and, in the absence of available outpatient care, a high degree of unmet need.
As a final step, the researchers compared emergency department visits for certain types of mental health conditions:
- Anxiety disorders compared to schizophrenia and other psychotic disorders
- Depressive disorders compared to suicidal ideation and intentional self-harm
Together, the findings highlight the nationwide use of emergency departments for mental health care, while emphasizing wide variations in rates of use between states and between mental disorders. The frequent use of emergency services for mental health care shown in this study might, in some cases, indicate a high degree of unmet need or a lack of access to outpatient mental health services.
Regional differences in Medicaid recipients’ mental health care experiences also demonstrate the importance of tailoring strategies to specific populations. The authors emphasize the need for context-specific, local solutions, which might start with looking at how mental health benefits are administered by state Medicaid agencies, determining the availability of local mental health providers, or identifying the most common types of mental disorders in communities.
UTILIZATION MANAGEMENT IN HEALTHCARE
https://www.smartsheet.com/content/utilization-management
Utilization management (UM) is a complex process that works to improve healthcare quality, reduce costs, and improve the overall health of the population.
What Is Utilization Management in Healthcare?
Utilization management (UM) is a process that evaluates the efficiency, appropriateness, and medical necessity of the treatments, services, procedures, and facilities provided to patients on a case-by-case basis. This process is run by — or on behalf of — purchasers of medical services (i.e., insurance providers) rather than by doctors. Hospitals, medical staff, insurers, and patients are all affected by UM.
Types of Utilization Management
UM has three main types of reviews: prospective, concurrent, and retrospective. This structure is comparable to the Donabedian model of healthcare quality, developed in the late 20th century by Avedis Donabedian. Each kind of review can impact the process differently.
A prospective review is an analysis of a patient’s case and their proposed treatment. Its main purpose is to eliminate unneeded, ineffective, or duplicate treatments. A prospective review is used during routine referrals and urgent referrals, but not for ER admissions. The review can occur before or after admission to a facility, but always before treatment begins. In some cases, a doctor’s orders may be overridden, which can cause resentment in the medical staff and patients.
Prospective reviews may also be known as precertification, preadmission certification, admission certification, prior authorization preservice review, or preprocedure review.
Concurrent Review
A concurrent review occurs while treatment is in progress and usually starts within 24-72 hours of admission to a hospital. The main focuses of the review are to track utilization of resources and the patient's progress, and to reduce denials of coverage after the treatment is complete. The following are included in the review:
A concurrent review can also be referred to as a continued stay review or an admission review.
Retrospective Review
A retrospective review is generally performed after treatment is complete. Its purpose is to assess the appropriateness, effectiveness, and timing of treatments, as well as the setting in which they were delivered.
The goal of a retrospective review is to see what treatments work best, so that those can be prescribed to similar patients in the future. It allows reviewers to find problems and successes, and send that data back to caregivers. You can also use this data in education and during contract negotiations between insurers and hospitals.
If proven treatments are not used, and a claim is denied, the financial burden falls on the caregiver. The process also looks to ensure that reimbursements are accurate, or if a claim should be denied. The review can also be redone if a denial is challenged or to respond to grievances.
A retrospective review can also be used at a key juncture of treatment rather than at the end, and the result may be that the patient’s treatment reverts back to a previous point. This change happens if the patient has not responded or the diagnosis changes, or if a different set of UM criteria comes into play (for example, if the patient’s insurance coverage changes).
Why Utilization Management Is Important
Utilization management began in the 1970s, but became prevalent in the 1980s, as healthcare costs started to rise more significantly than they had in past decades. Insurers and employers were looking for ways to control costs — and one of the key goals of UM is to keep costs down.
Utilization management looks at the effectiveness of treatments for each patient, both while they are occurring and after they are over. This analysis contributes to the second and third goals of UM, which are improving patient care and increasing the overall health of the population.
Reviewing treatments also contributes to the final goal of utilization management, which is to reduce denials. By using data gathered in a retrospective review, you can evaluate the effectiveness of treatments. When caregivers prescribe these treatments, insurers are more likely to approve them.
Below are a few other reasons that utilization management is important for patients, healthcare providers, and insurance companies:
Benefits of Utilization Management
A well-run utilization management program has benefits for all parties involved: patients, healthcare providers, and insurers. The pros for each are as follows:
In utilization management, treatment is evaluated and approved either proactively (during prospective review) or while in progress (during concurrent review), creating fewer reasons to deny claims.
For example, after a primary care physician informs a patient that their diagnosis requires surgery (as well as referral to a surgeon), a patient contacts her employer’s insurance provider. The insurance provider contacts the surgeon to discuss the following options:
How Utilization Management Can Improve Care
In a fee-for-service healthcare model, patients will receive unnecessary and inefficient treatment. During the retrospective process of utilization management, examine the results of treatments and compare them to other treatments. Next, evaluate the data collected during this process and apply the findings to future patients in similar situations.
Here is another example of how utilization management improves care: A hospital admits a heart attack patient after they have been stabilized in the ER. The hospital contacts the patient’s insurance provider and they discuss the options for treatment and the optimal length of stay. The insurance provider checks in for progress reports regularly. The doctor says that the original treatment plan is not getting the expected results, so they change to a different treatment that has shown promise in similar patients.
Since the insurance company and doctor worked together to evaluate progress, they were able to find a course of treatment that could yield better results.
How Utilization Management Can Help Contain Costs
As doctors try new treatments, each are evaluated for efficacy compared to existing options. Treatments that get results will be covered in the future; those that don’t will not be covered going forward. The costs associated with running a UM program are small compared with the savings that one can achieve.
In addition, the following actions by insurance providers can also contribute to the goal of reducing costs:
Challenges in Utilization Management
Like any process, utilization management isn’t perfect. There are issues that can create resistance and anger among both patients and healthcare professionals, including the following:
The UM process is complex. Requirements will vary by location, partners, and focus of the medical organization. It’s impossible to map a process flow that will apply generally, but you can start by following the steps in the prospective, concurrent, and retrospective review.
Steps in Utilization Management
In this section, you’ll learn the basic steps that occur in the prospective, concurrent, and retrospective reviews. Not all steps will happen for all patients (for example, an emergency room admittance for a heart attack will most likely not have any prospective review steps), and you may need to repeat some of these steps if you appeal a declined treatment.
Prospective Review
Utilization Management versus Utilization Review
The two terms are occasionally used as synonyms. Utilization review (UR) is a process in which patient records are reviewed for accuracy and completion of treatment, after the treatment is complete. UR, a separate activity, can be a part of UM (specifically during retrospective review), and can drive changes to the UM process.
Utilization Management versus Case Management
Professionals can’t always agree on the definition of case management, but according to the Case Management Body of Knowledge, it’s “...a professional and collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual’s health needs.”
Case management promotes patient health, service quality, and cost-effective outcomes.
Introduction to the Case Management Body of Knowledge
https://cmbodyofknowledge.com/content/introduction-case-management-body-knowledge
People and Entities Involved in Utilization Management
In addition to the nurses, doctors, hospitals (from small town clinics to well-known facilities like the Mayo Clinic), their staff (including program managers, medical directors, and referral coordinators), private insurance companies (e.g., Aetna and Allstate), there are a number of other entities that are important to UM.
https://www.smartsheet.com/content/utilization-management
Utilization management (UM) is a complex process that works to improve healthcare quality, reduce costs, and improve the overall health of the population.
What Is Utilization Management in Healthcare?
Utilization management (UM) is a process that evaluates the efficiency, appropriateness, and medical necessity of the treatments, services, procedures, and facilities provided to patients on a case-by-case basis. This process is run by — or on behalf of — purchasers of medical services (i.e., insurance providers) rather than by doctors. Hospitals, medical staff, insurers, and patients are all affected by UM.
Types of Utilization Management
UM has three main types of reviews: prospective, concurrent, and retrospective. This structure is comparable to the Donabedian model of healthcare quality, developed in the late 20th century by Avedis Donabedian. Each kind of review can impact the process differently.
- Prospective Review: Performed before or at the onset of treatment, on a case-by-case basis, this review is designed to eliminate unneeded services. The chosen treatment should be considered contingent, and may be changed later.
- Concurrent Review: This type of review occurs during the course of treatment and tracks a patient’s progress and resource consumption; which may cause in-process care procedures to stop.
- Retrospective Review: Conducted after treatment is done, the review assess the appropriateness and efficacy of the treatment in order to provide data for future patients.
A prospective review is an analysis of a patient’s case and their proposed treatment. Its main purpose is to eliminate unneeded, ineffective, or duplicate treatments. A prospective review is used during routine referrals and urgent referrals, but not for ER admissions. The review can occur before or after admission to a facility, but always before treatment begins. In some cases, a doctor’s orders may be overridden, which can cause resentment in the medical staff and patients.
Prospective reviews may also be known as precertification, preadmission certification, admission certification, prior authorization preservice review, or preprocedure review.
Concurrent Review
A concurrent review occurs while treatment is in progress and usually starts within 24-72 hours of admission to a hospital. The main focuses of the review are to track utilization of resources and the patient's progress, and to reduce denials of coverage after the treatment is complete. The following are included in the review:
- Care Coordination: Syncing the delivery of a patient’s health care when it comes from multiple providers or specialists.
- Discharge Planning: Determining what needs or milestones need to be met for a patient to leave the hospital.
- Care Transition: When a patient moves from one level of care to another (for example, from ICU to standard care).
A concurrent review can also be referred to as a continued stay review or an admission review.
Retrospective Review
A retrospective review is generally performed after treatment is complete. Its purpose is to assess the appropriateness, effectiveness, and timing of treatments, as well as the setting in which they were delivered.
The goal of a retrospective review is to see what treatments work best, so that those can be prescribed to similar patients in the future. It allows reviewers to find problems and successes, and send that data back to caregivers. You can also use this data in education and during contract negotiations between insurers and hospitals.
If proven treatments are not used, and a claim is denied, the financial burden falls on the caregiver. The process also looks to ensure that reimbursements are accurate, or if a claim should be denied. The review can also be redone if a denial is challenged or to respond to grievances.
A retrospective review can also be used at a key juncture of treatment rather than at the end, and the result may be that the patient’s treatment reverts back to a previous point. This change happens if the patient has not responded or the diagnosis changes, or if a different set of UM criteria comes into play (for example, if the patient’s insurance coverage changes).
Why Utilization Management Is Important
Utilization management began in the 1970s, but became prevalent in the 1980s, as healthcare costs started to rise more significantly than they had in past decades. Insurers and employers were looking for ways to control costs — and one of the key goals of UM is to keep costs down.
Utilization management looks at the effectiveness of treatments for each patient, both while they are occurring and after they are over. This analysis contributes to the second and third goals of UM, which are improving patient care and increasing the overall health of the population.
Reviewing treatments also contributes to the final goal of utilization management, which is to reduce denials. By using data gathered in a retrospective review, you can evaluate the effectiveness of treatments. When caregivers prescribe these treatments, insurers are more likely to approve them.
Below are a few other reasons that utilization management is important for patients, healthcare providers, and insurance companies:
- In the U.S., health insurance is mainly provided by employers. Increases in healthcare costs impact the profitability and competitiveness of the companies that provide these benefits. The private sector pays for the healthcare of most people under 65 (whether employer or individuals); effective treatments help sick or injured people get back to being productive, and also save money.
- Companies that self-insure assume the financial risk of health costs of their employees and dependants. Utilization management can help prevent one person’s health problems from negatively impacting the resources available for other people.
- The costs associated with running a utilization management program are small compared to the savings it can achieve.
- The effectiveness of new and experimental treatments are evaluated and made more available if they are better or cheaper than existing ones.
- Unnecessary or harmful treatments can be discovered and stopped.
- The average age of the population is rising, and so is the demand for effective treatment.
Benefits of Utilization Management
A well-run utilization management program has benefits for all parties involved: patients, healthcare providers, and insurers. The pros for each are as follows:
- Patients: Get lower costs, more effective treatments, and fewer claim denials.
- Healthcare Providers: Get fewer claim denials, lower costs, more effective treatments, better data, and better resource deployment.
- Insurers: Get lower costs, better data, and the evaluation of the effectiveness of new treatments and protocols.
In utilization management, treatment is evaluated and approved either proactively (during prospective review) or while in progress (during concurrent review), creating fewer reasons to deny claims.
For example, after a primary care physician informs a patient that their diagnosis requires surgery (as well as referral to a surgeon), a patient contacts her employer’s insurance provider. The insurance provider contacts the surgeon to discuss the following options:
- In discussing inpatient versus outpatient surgery, they see that inpatient procedures have fewer complications, so they opt for that.
- They determine that pre-surgical tests can be performed on an outpatient basis.
- Based on those conclusions, they settle on the anticipated post-surgery recovery time and scheduled release date.
How Utilization Management Can Improve Care
In a fee-for-service healthcare model, patients will receive unnecessary and inefficient treatment. During the retrospective process of utilization management, examine the results of treatments and compare them to other treatments. Next, evaluate the data collected during this process and apply the findings to future patients in similar situations.
Here is another example of how utilization management improves care: A hospital admits a heart attack patient after they have been stabilized in the ER. The hospital contacts the patient’s insurance provider and they discuss the options for treatment and the optimal length of stay. The insurance provider checks in for progress reports regularly. The doctor says that the original treatment plan is not getting the expected results, so they change to a different treatment that has shown promise in similar patients.
Since the insurance company and doctor worked together to evaluate progress, they were able to find a course of treatment that could yield better results.
How Utilization Management Can Help Contain Costs
As doctors try new treatments, each are evaluated for efficacy compared to existing options. Treatments that get results will be covered in the future; those that don’t will not be covered going forward. The costs associated with running a UM program are small compared with the savings that one can achieve.
In addition, the following actions by insurance providers can also contribute to the goal of reducing costs:
- Incentives for doctors to prescribe less-costly treatments
- Education and feedback for doctors about effective care standards and practices
- Gatekeeping to manage patient referrals away from expensive services and specialists
- Patient education
- Design benefits to reward patients and healthcare providers that opt for less expensive treatments
- Contracts with providers that have proven records of cost containment
Challenges in Utilization Management
Like any process, utilization management isn’t perfect. There are issues that can create resistance and anger among both patients and healthcare professionals, including the following:
- Costs can fall on patients if post-treatment reviews result in a denial of benefits.
- Patients may have to bear costs if they don’t follow the treatment guidelines of the insurer.
- Patients may sue when coverage is denied, or if an experimental treatment is not permitted.
- Physicians don’t always have the insurer’s medical necessity guidelines as their first consideration when delivering care.
- Concurrent and prospective reviews may overturn wishes of primary care physicians.
- The number of reviews are rising, as are denials of coverage.
- The process steps required by insurers can be perceived as red tape or unnecessary by healthcare workers.
- Physicians may not well-receive the results of retrospective reviews.
- Even with UM in place, the cost of care is still high, so it may be seen as ineffective.
- There is non-response or non-payment from an insurer (sometimes called de facto denial).
- Some tests may reduce uncertainty about the patient’s diagnosis, but not add any information that helps determine if a treatment is effective or not. Doctors may see these tests as important, but insurers might not have the same view.
- The number of insurance providers and the coverage available may cause costs to fluctuate.
- There may be a difference between the best practice and most cost-effective treatment, which can create a conflict between doctors and insurance companies.
- The process can be burdensome on medical staff, taking them away from time that could be better spent with patients.
- Review criteria are often hidden from doctors and patients, so they may not know why coverage is denied.
- UM may not have as big an effect as was once thought. In the same 2002 paper, Wickizer and Lessler found that “evaluations of UM have generated mixed findings, with some studies showing reductions in utilization and costs and others showing little effect.”
- Contract exclusions, including services that aren’t covered or having services performed at facilities that aren't in an insurer’s network.
- Prescribed treatments that are unproven or investigational. (However, treatments are constantly under evaluation, so something denied today may be covered in the future.)
- Lack of medical necessity of a treatment.
- Technical errors in the documentation, such as missing or incomplete information.
The UM process is complex. Requirements will vary by location, partners, and focus of the medical organization. It’s impossible to map a process flow that will apply generally, but you can start by following the steps in the prospective, concurrent, and retrospective review.
Steps in Utilization Management
In this section, you’ll learn the basic steps that occur in the prospective, concurrent, and retrospective reviews. Not all steps will happen for all patients (for example, an emergency room admittance for a heart attack will most likely not have any prospective review steps), and you may need to repeat some of these steps if you appeal a declined treatment.
Prospective Review
- Verify the patient’s coverage and eligibility of the proposed treatment.
- Collect the patient’s clinical information to determine the level of care needed and if the proposed treatment is medically necessary.
- Approve the treatment if criteria are met; deny it if not.
- If denied, the physician can appeal.
- Continue to collect patient’s progress, prognosis, cost, and resource usage.
- Insurer reviews data.
- Approve to continue or request to change treatment.
- If a change is requested, the physician can appeal.
- Insurer reviews a patient’s records.
- Based on the results, the insurer may update their criteria for covered treatments.
- In some cases, coverage will be denied at this point.
- If denied, the physician or patient can appeal.
Utilization Management versus Utilization Review
The two terms are occasionally used as synonyms. Utilization review (UR) is a process in which patient records are reviewed for accuracy and completion of treatment, after the treatment is complete. UR, a separate activity, can be a part of UM (specifically during retrospective review), and can drive changes to the UM process.
Utilization Management versus Case Management
Professionals can’t always agree on the definition of case management, but according to the Case Management Body of Knowledge, it’s “...a professional and collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual’s health needs.”
Case management promotes patient health, service quality, and cost-effective outcomes.
Introduction to the Case Management Body of Knowledge
https://cmbodyofknowledge.com/content/introduction-case-management-body-knowledge
People and Entities Involved in Utilization Management
In addition to the nurses, doctors, hospitals (from small town clinics to well-known facilities like the Mayo Clinic), their staff (including program managers, medical directors, and referral coordinators), private insurance companies (e.g., Aetna and Allstate), there are a number of other entities that are important to UM.
- Medicare: A government-run insurance program for people 65 and older.
- Medicaid: A government-run insurance program for low income people.
- Prefered Provider Organization (PPOs): An example of managed care. They are health insurance companies that contract with healthcare providers for reduced rates.
- Health Maintenance Organization (HMOs): Another type of managed care that provides both insurance and healthcare, or works with closely-affiliated entities for healthcare.... HMOs are sometimes called integrated delivery systems, and they drove the growth of UM in the 1980s. HMOs generally have higher quality and lower costs than PPOs.
- URAC: An organization that accredits utilization management programs and provides education as well.
- National Association of Insurance Commissioners (NAIC): An entity that sets standards and defines regulations for the insurance industry, including how to implement UM.
- American Hospital Association (AHA): A professional association that is one of the drivers behind UM, and acts as a clearinghouse for national healthcare data for their members.
- Iowa Hospital Association (IHA): A regional version of the AHA.
- American Physical Therapy Association (APTA): An entity that provides information and guidance about UM to its members.
- National Academy of Medicine (NAM): Formerly known as IOM (Institute of Medicine), NAM is affiliated with the National Academy of Science. The organization provides information and advice about health and health policy. It ran an advisory board called the Committee on Utilization Management by Third Parties, which helped improve the effectiveness of UM.
- Recovery Audit Contractors: These people review claims for Medicare and Medicaid to find and correct errors, improper reimbursement, incorrect coding of services, non-covered services, and duplicate services. They are partly reimbursed based on the improper payments they identify.
- Centers for Medicare and Medicaid Services (CMS): A federal agency that is involved with the administration of those programs, plus CHIP (Children’s Health Insurance Program), the federal health insurance marketplace, and HIPAA (Health Insurance Portability and Accountability Act) program. CMS provides data on healthcare quality and costs to the public.
- Peer Review Organizations (PROs): Groups of local doctors mandated by the 1982 Tax Equity and Fiscal Responsibility Act that look at the quality and cost of services to ensure they meet Medicare requirements for quality and cost.
- Independent Practice Association (IPA): An association of independent physicians that contracts with care delivery organizations to provide services to managed care organizations like HMOs and PPOs.
- Managed Care Resources: A nurse-owned organization that works with managed care organizations.
- Envolve Healthcare: A private company that provides services to insurance companies and medical service providers to help them manage their UM programs
- UM Reviewers: People who help resolve conflicts that come up when case decisions are disputed or challenged.
- Utilization Management Nurses: Nurses who work for insurers or hospitals, and are involved in deciding the type of treatment patients receive.
- Clinical Documentation Improvement (CDI) Specialists: People who examine documentation used to communicate with insurers to look for any red flags or enhancement opportunities.
- Physician Advisors: People who review cases for which the proposed treatment may not be approved, and make recommendations to improve the chances of approval. They are sometimes tasked with running the overall UM program.
- Independent Review Organizations (IROs): Organizations that can be tasked with looking at denied claims and supporting or overturning the denials.
INTRODUCTION TO THE CASE MANAGEMENT BODY OF KNOWLEDGE
https://cmbodyofknowledge.com/content/introduction-case-management-body-knowledge
Definition of Case Management
There is no one standardized or nationally recognized or even widely accepted definition of case management. An Internet search for the definition of the term case management will result in thousands of references. Such results are confusing for case managers and others who are interested in case management practice. You may be unable to discern which definition is most credible or relevant.
Despite the large search outcome, experts would agree that there are no more than 20 or so definitions of case management considered appropriate. These definitions are available in peer-reviewed professional case management literature or on websites and in other formal documents of case management (or case management–related) organizations, societies, and government or nongovernment agencies.
The Case Management Knowledge Framework
“Case management is a professional and collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual’s health needs. It uses communication and available resources to promote health, quality, and cost-effective outcomes in support of the ‘Triple Aim,’ of improving the experience of care, improving the health of populations, and reducing per capita costs of health care.” (CCMC, 2015, p. 4)
Case Management Philosophy and Guiding Principles
Case management is a specialty practice within the health and human services profession. Everyone directly or indirectly involved in healthcare benefits when healthcare professionals and especially case managers appropriately manage, efficiently provide, and effectively execute a client’s care. The underlying guiding principles of case management services and practices of the CMBOK follow:
Principal Terms Used in the Case Management
Benefit programs
The sum of services offered by a health insurance plan, government agency, or employer to individuals based on some sort of an agreement between the parties (e.g., employer and employee). Benefits vary based on the plan and may include physician and hospital services, prescriptions, dental and vision care, workers’ compensation, long-term care, mental and behavioral health, disability and accidental death, counseling, and other therapies such as chiropractic care.
Benefits
The type of health and human services covered by a health insurance plan (sometimes referred to as health insurance benefits, health benefits, or benefits plan) and as agreed upon between an insurance company and an individual enrollee or participant. The term also refers to the amount payable by an insurance company to a claimant or beneficiary under the claimant’s specific coverage as stipulated in the health insurance plan.
Caregiver
The person responsible for caring for a client in the home setting and can be a family member, friend, volunteer, or an assigned healthcare professional.
Case manager
The health and human services professional responsible for coordinating the overall care delivered to an individual client or a group of clients, based on the client’s health or human services issues, needs, and interests.
Case management plan of care
A comprehensive plan of care for an individual client that describes:
Case Management Process
The process through which case managers provide health and human services to clients/support systems. The process consists of several phases that are iterative, cyclical, and recursive rather than linear and that are applied until clients’ needs and interests are met.
The phases of the process are:
Case management program (Also referred to as case management department.)
An organized approach to the provision of case management services to clients and their support systems. The program is usually described in terms of:
Client
The recipient of case management as well as health and human services. “This individual can be a patient, beneficiary, injured worker, claimant, enrollee, member, college student, resident, or health care consumer of any age group. In addition, [use of] the term client may also infer the inclusion of the client’s support [system]” (CMSA, 2016, p. 32).
NOTE: the term client is sometimes intended to include the client’s support system.
Client’s support system
The person or persons identified by each individual client to be directly or indirectly involved in the client’s care. It “may include biological relatives [family members], a spouse, a partner, friends, neighbors, colleagues, a health care proxy, or any individual who supports the client [caregivers, volunteers, and clergy or spiritual advisors]” (CMSA, 2016, p. 32).
Community services and resources
Healthcare programs that offer specific services and resources in a community-based environment as opposed to an institutional setting (i.e., outside the confines of healthcare facilities such as hospitals and nursing homes). These programs either are publicly or privately funded or are charitable in nature.
Health
An individual’s physical, functional, mental, behavioral, emotional, psychosocial, and cognitive condition. It refers to the presence or absence of illness, disability, injury, or limitation that requires special management and resolution, including the use of health and human services-type interventions or resources.
NOTE: the term health implies all aspects of health as described in the principal term, reflecting a holistic view of the client’s condition or situation.
Health and human services continuum
The range of care that matches the ongoing needs of clients as they are served over time by the Case Management Process and case managers. It includes the appropriate levels and types of care – health, medical, financial, legal, psychosocial, and behavioral – across one or more care settings. The levels of care vary in complexity and intensity of healthcare services and resources, including individual providers, organizations, and agencies.
NOTE: the term healthcare refers to and incorporates “health and human services,” reflecting the broader community of professionals who serve clients and the continuum of services they provide.
Knowledge domain
A collection of information topics associated with health and human services and related subjects. These topics are organized around common themes (domains) to form high-level/abstract concepts that are considered to be essential for effective and competent performance of case managers. Examples of case management knowledge domains are Quality and Outcomes Evaluation and Measurement, and Care Delivery and Reimbursement Methods.
Level of care
The intensity and effort of health and human services and care activities required to diagnose, treat, preserve, or maintain clients’ health. Level of care may vary from least to most complex, least to most intense, or prevention and wellness to acute care and services.
Community services and resources
Healthcare programs that offer specific services and resources in a community-based environment as opposed to an institutional setting (i.e., outside the confines of healthcare facilities such as hospitals and nursing homes). These programs either are publicly or privately funded or are charitable in nature.
Payor
The person, agency, or organization that assumes responsibility for funding the health and human services and resources consumed by a client. Payors may be clients themselves, a member of the client’s support system, an employer, a government benefit program (e.g., Medicare, Medicaid, or TriCare), a commercial insurance agency, or a charitable organization.
Practice setting(Also referred to as practice site, care setting, or work setting.)
The organization or agency at which case managers are employed and execute their roles and responsibilities. The practice of case management extends across all settings of the health and human services continuum. These may include, but are not limited to, payor, provider, government, employer, community, independent/private, workers’ compensation, or a client’s home environment.
Professional discipline
Case managers’ formal education, training, and specialization or professional background that is necessary and prerequisite for consideration as health and human services practitioners. Also refers to the professional background – such as nursing, medicine, social work, or rehabilitation – that case managers bring with them into the practice of case management.
ServicesInterventions, medical treatments, diagnostics, and other activities implemented to manage clients’ conditions, including health and human services issues and needs. The types of services implemented can be found in an individual client’s case management plan of care, medical treatment plan, or other related documents as applicable to the healthcare setting and the professional discipline of the provider of care and services.
NOTE: The term services is used to include the various types of care and services described above.
The Case Management Process
The Case Management Process consists of nine phases through which case managers provide care to their clients: Screening, Assessing, Stratifying Risk, Planning, Implementing (Care Coordination), Following-Up, Transitioning (Transitional Care), Communicating Post Transition, and Evaluating. The overall process is iterative, nonlinear, and cyclical, its phases being revisited as necessary until the desired outcome is achieved.
Centering on a client and the client’s support system, the Case Management Process is holistic in its approach to the management of the client’s situation and that of the client’s support system. It is adaptive both to the case manager’s practice setting and to the healthcare setting in which the client receives services.
Client Source
Before looking more closely at the phases of the Case Management Process, first consider what triggers the process. You begin with the identification of a client. Without a client found to be in need of case management services, you have no need to launch the Case Management Process.
The client source – that is, how you, as case managers, come in contact with clients and/or their support systems – varies based on your practice setting.
Examples of Client Sources (Care/Practice Setting)
Payor-based case manager
May implement the Case Management Process for a client upon direct contact via the telephone by the client/support system or upon referral from other professionals working for the payor organization such as a medical director, a claims adjuster, a clerical person, or a quality/performance improvement specialist.
Acute care setting–based case manager
May implement the Case Management Process for a client after referral from any of the healthcare team members, including the physician, primary nurse, social worker, consultant, specialist, therapist, dietitian, or manager.In some organizations, case managers may visit every new admission and conduct a high-level review of the client’s situation for the purpose of identifying whether the client would benefit from case management services.
Community care setting–based case manager
May implement the Case Management Process for a client after referral from the primary care provider or specialty care provider.
In some instances, the case manager may initiate the process based on a request from the client/support system or based on a regulatory obligation such as health home requirement for Medicare or Medicaid beneficiaries participating in an accountable care organization or federally qualified healthcare center.
Vocational rehabilitation– or workers’ compensation–based case manager
May implement the Case Management Process for a client after referral from the acute- or community-based case manager or other healthcare providers who have identified the client would benefit from vocational rehabilitation case management services.In some instances, an employer may refer a client (e.g., on-the-job injured worker) for vocational rehabilitation as part of the return-to-work plan of care.
https://cmbodyofknowledge.com/content/introduction-case-management-body-knowledge
Definition of Case Management
There is no one standardized or nationally recognized or even widely accepted definition of case management. An Internet search for the definition of the term case management will result in thousands of references. Such results are confusing for case managers and others who are interested in case management practice. You may be unable to discern which definition is most credible or relevant.
Despite the large search outcome, experts would agree that there are no more than 20 or so definitions of case management considered appropriate. These definitions are available in peer-reviewed professional case management literature or on websites and in other formal documents of case management (or case management–related) organizations, societies, and government or nongovernment agencies.
The Case Management Knowledge Framework
“Case management is a professional and collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet an individual’s health needs. It uses communication and available resources to promote health, quality, and cost-effective outcomes in support of the ‘Triple Aim,’ of improving the experience of care, improving the health of populations, and reducing per capita costs of health care.” (CCMC, 2015, p. 4)
Case Management Philosophy and Guiding Principles
Case management is a specialty practice within the health and human services profession. Everyone directly or indirectly involved in healthcare benefits when healthcare professionals and especially case managers appropriately manage, efficiently provide, and effectively execute a client’s care. The underlying guiding principles of case management services and practices of the CMBOK follow:
- Case management is not a profession unto itself. Rather, it is a cross-disciplinary and interdependent specialty practice.
- Case management is a means for improving clients’ health and promoting wellness and autonomy through advocacy, communication, education, identification of service resources, and facilitation of service.
- Case management is guided by the ethical principles of autonomy, beneficence, nonmaleficence, veracity, equity, and justice.
- Case managers come from different backgrounds within health and human services professions, including nursing, medicine, social work, rehabilitation counseling, workers’ compensation, and mental and behavioral health.
- The primary function of case managers is to advocate for clients/support systems. Case managers understand the importance of achieving quality outcomes for their clients and commit to the appropriate use of resources and empowerment of clients in a manner that is supportive and objective.
- Case managers’ first duty is to their clients – coordinating care that is safe, timely, effective, efficient, equitable, and client-centered.
- Case management services are offered according to the clients’ benefits as stipulated in their health insurance plans, where applicable.
- The Case Management Process is centered on clients/support systems. It is holistic in its handling of clients’ situations (e.g., addressing medical, physical, functional, emotional, financial, psychosocial, behavioral, spiritual, and other needs), as well as those of their support systems.
- The Case Management Process is adaptive to case managers’ practice settings and the settings where clients receive health and human services.
- Case managers approach the provision of case-managed health and human services in a collaborative manner. Professionals from within or across healthcare organizations (e.g., provider, employer, payor, and community agencies) and settings collaborate closely for the benefit of clients/support systems.
- The goals of case management are first and foremost focused on improving the client’s clinical, functional, emotional, and psychosocial status.
- The healthcare organizations for which case managers work may also benefit from case management services. They may realize lowered health claim costs (if payor-based), shorter lengths of stay (if acute care–based), or early return to work and reduced absenteeism (if employer-based).
- All stakeholders benefit when clients reach their optimum level of wellness, self-care management, and functional capability. These stakeholders include the clients themselves, their support systems, and the healthcare delivery systems, including the providers of care, the employers, and the various payor sources.
- Case management helps clients achieve wellness and autonomy through advocacy, comprehensive assessment, planning, communication, health education and engagement, resource management, service facilitation, and use of evidence-based guidelines or standards.
- Based on the cultural beliefs, values, and needs of clients/support systems and in collaboration with all service providers (both healthcare professionals and paraprofessionals), case managers link clients/support systems with appropriate providers of care and resources throughout the continuum of health and human services and across various care settings. They do so while ensuring that the care provided is safe, effective, client-centered, timely, efficient, and equitable. This approach achieves optimum value and desirable outcomes for all stakeholders.
- Case management services are optimized when offered in a climate that allows direct, open, and honest communication and collaboration among the case manager, the client/support system, the payor, the primary care provider (PCP), the specialty care provider (SCP), and all other service delivery professionals and paraprofessionals.
- Case managers enhance the case management services and their associated outcomes by maintaining clients’ privacy, confidentiality, health, and safety through advocacy and adherence to ethical, legal, accreditation, certification, and regulatory standards and guidelines, as appropriate to the practice setting.
- Case managers must possess the education, skills, knowledge, competencies, and experiences needed to effectively render appropriate, safe, and quality services to their clients/support systems.
- Case managers must demonstrate a sense of commitment and obligation to maintain current knowledge, skills, and competencies. They also must disseminate their practice innovations and findings from research activities to the case management community for the benefit of advancing the field of case management.
Principal Terms Used in the Case Management
Benefit programs
The sum of services offered by a health insurance plan, government agency, or employer to individuals based on some sort of an agreement between the parties (e.g., employer and employee). Benefits vary based on the plan and may include physician and hospital services, prescriptions, dental and vision care, workers’ compensation, long-term care, mental and behavioral health, disability and accidental death, counseling, and other therapies such as chiropractic care.
Benefits
The type of health and human services covered by a health insurance plan (sometimes referred to as health insurance benefits, health benefits, or benefits plan) and as agreed upon between an insurance company and an individual enrollee or participant. The term also refers to the amount payable by an insurance company to a claimant or beneficiary under the claimant’s specific coverage as stipulated in the health insurance plan.
Caregiver
The person responsible for caring for a client in the home setting and can be a family member, friend, volunteer, or an assigned healthcare professional.
Case manager
The health and human services professional responsible for coordinating the overall care delivered to an individual client or a group of clients, based on the client’s health or human services issues, needs, and interests.
Case management plan of care
A comprehensive plan of care for an individual client that describes:
- The client’s problems, needs, and desires, as determined from the findings of the client’s assessment.
- The strategies – such as treatments and interventions – to be instituted to address the client’s problems and needs.
- The measurable goals – including specific outcomes – to be achieved to demonstrate resolution of the client’s problems and needs, the time frame(s) for achieving them, the resources available and to be used to realize the outcomes, and the desires/motivation of the client that may have an impact on the plan (CMSA, 2016, p. 32).
Case Management Process
The process through which case managers provide health and human services to clients/support systems. The process consists of several phases that are iterative, cyclical, and recursive rather than linear and that are applied until clients’ needs and interests are met.
The phases of the process are:
- Screening
- Assessing
- Stratifying Risk
- Planning
- Implementing (Care Coordination)
- Following-Up
- Transitioning (Transitional Care)
- Communicating Post Transition
- Evaluating
Case management program (Also referred to as case management department.)
An organized approach to the provision of case management services to clients and their support systems. The program is usually described in terms of:
- Vision, mission, purpose, goals, strategic objectives, and target outcomes
- Number and type of staff, including roles, responsibilities, and expectations of each
- A specific model or conceptual framework that delineates the key case management functions within the program or department
- Reporting structure within the organization
- How the program or department connect with or relate to other programs or departments within the healthcare organization
- The process and metrics applied in the evaluation or the program or department and its contribution to the healthcare organization, especially its bottom line
Client
The recipient of case management as well as health and human services. “This individual can be a patient, beneficiary, injured worker, claimant, enrollee, member, college student, resident, or health care consumer of any age group. In addition, [use of] the term client may also infer the inclusion of the client’s support [system]” (CMSA, 2016, p. 32).
NOTE: the term client is sometimes intended to include the client’s support system.
Client’s support system
The person or persons identified by each individual client to be directly or indirectly involved in the client’s care. It “may include biological relatives [family members], a spouse, a partner, friends, neighbors, colleagues, a health care proxy, or any individual who supports the client [caregivers, volunteers, and clergy or spiritual advisors]” (CMSA, 2016, p. 32).
Community services and resources
Healthcare programs that offer specific services and resources in a community-based environment as opposed to an institutional setting (i.e., outside the confines of healthcare facilities such as hospitals and nursing homes). These programs either are publicly or privately funded or are charitable in nature.
Health
An individual’s physical, functional, mental, behavioral, emotional, psychosocial, and cognitive condition. It refers to the presence or absence of illness, disability, injury, or limitation that requires special management and resolution, including the use of health and human services-type interventions or resources.
NOTE: the term health implies all aspects of health as described in the principal term, reflecting a holistic view of the client’s condition or situation.
Health and human services continuum
The range of care that matches the ongoing needs of clients as they are served over time by the Case Management Process and case managers. It includes the appropriate levels and types of care – health, medical, financial, legal, psychosocial, and behavioral – across one or more care settings. The levels of care vary in complexity and intensity of healthcare services and resources, including individual providers, organizations, and agencies.
NOTE: the term healthcare refers to and incorporates “health and human services,” reflecting the broader community of professionals who serve clients and the continuum of services they provide.
Knowledge domain
A collection of information topics associated with health and human services and related subjects. These topics are organized around common themes (domains) to form high-level/abstract concepts that are considered to be essential for effective and competent performance of case managers. Examples of case management knowledge domains are Quality and Outcomes Evaluation and Measurement, and Care Delivery and Reimbursement Methods.
Level of care
The intensity and effort of health and human services and care activities required to diagnose, treat, preserve, or maintain clients’ health. Level of care may vary from least to most complex, least to most intense, or prevention and wellness to acute care and services.
Community services and resources
Healthcare programs that offer specific services and resources in a community-based environment as opposed to an institutional setting (i.e., outside the confines of healthcare facilities such as hospitals and nursing homes). These programs either are publicly or privately funded or are charitable in nature.
Payor
The person, agency, or organization that assumes responsibility for funding the health and human services and resources consumed by a client. Payors may be clients themselves, a member of the client’s support system, an employer, a government benefit program (e.g., Medicare, Medicaid, or TriCare), a commercial insurance agency, or a charitable organization.
Practice setting(Also referred to as practice site, care setting, or work setting.)
The organization or agency at which case managers are employed and execute their roles and responsibilities. The practice of case management extends across all settings of the health and human services continuum. These may include, but are not limited to, payor, provider, government, employer, community, independent/private, workers’ compensation, or a client’s home environment.
Professional discipline
Case managers’ formal education, training, and specialization or professional background that is necessary and prerequisite for consideration as health and human services practitioners. Also refers to the professional background – such as nursing, medicine, social work, or rehabilitation – that case managers bring with them into the practice of case management.
ServicesInterventions, medical treatments, diagnostics, and other activities implemented to manage clients’ conditions, including health and human services issues and needs. The types of services implemented can be found in an individual client’s case management plan of care, medical treatment plan, or other related documents as applicable to the healthcare setting and the professional discipline of the provider of care and services.
NOTE: The term services is used to include the various types of care and services described above.
The Case Management Process
The Case Management Process consists of nine phases through which case managers provide care to their clients: Screening, Assessing, Stratifying Risk, Planning, Implementing (Care Coordination), Following-Up, Transitioning (Transitional Care), Communicating Post Transition, and Evaluating. The overall process is iterative, nonlinear, and cyclical, its phases being revisited as necessary until the desired outcome is achieved.
Centering on a client and the client’s support system, the Case Management Process is holistic in its approach to the management of the client’s situation and that of the client’s support system. It is adaptive both to the case manager’s practice setting and to the healthcare setting in which the client receives services.
Client Source
Before looking more closely at the phases of the Case Management Process, first consider what triggers the process. You begin with the identification of a client. Without a client found to be in need of case management services, you have no need to launch the Case Management Process.
The client source – that is, how you, as case managers, come in contact with clients and/or their support systems – varies based on your practice setting.
Examples of Client Sources (Care/Practice Setting)
Payor-based case manager
May implement the Case Management Process for a client upon direct contact via the telephone by the client/support system or upon referral from other professionals working for the payor organization such as a medical director, a claims adjuster, a clerical person, or a quality/performance improvement specialist.
Acute care setting–based case manager
May implement the Case Management Process for a client after referral from any of the healthcare team members, including the physician, primary nurse, social worker, consultant, specialist, therapist, dietitian, or manager.In some organizations, case managers may visit every new admission and conduct a high-level review of the client’s situation for the purpose of identifying whether the client would benefit from case management services.
Community care setting–based case manager
May implement the Case Management Process for a client after referral from the primary care provider or specialty care provider.
In some instances, the case manager may initiate the process based on a request from the client/support system or based on a regulatory obligation such as health home requirement for Medicare or Medicaid beneficiaries participating in an accountable care organization or federally qualified healthcare center.
Vocational rehabilitation– or workers’ compensation–based case manager
May implement the Case Management Process for a client after referral from the acute- or community-based case manager or other healthcare providers who have identified the client would benefit from vocational rehabilitation case management services.In some instances, an employer may refer a client (e.g., on-the-job injured worker) for vocational rehabilitation as part of the return-to-work plan of care.
GUIDE TO PROCEDURE CODES FOR SPECIALTY MENTAL HEALTH SERVICES
Los Angeles County Department of Mental Health
Effective May 28, 2021
INTRODUCTION
This Guide, prepared by DMH, lists and defines the compliant codes that DMH believes reflects the services it provides throughout its system, whether by directly-operated, contracted organizational providers, or individual/group network providers. This analysis does not, however, absolve Providers, whether individuals or agencies from their responsibility to be familiar with nationally compliant codes and to inform and dialogue with DMH should they believe differences exist.
Brief History
Since the inception of the DMH’s first computer system in 1982, DMH directly-operated and contract staff have reported services using Activity Codes. These Activity Codes were then translated into the types of mental health services for which DMH could be reimbursed through a variety of funding sources. On April 14, 2003, health care providers throughout the Country implemented the HIPAA Privacy rules. This brought many changes to DMH’s way of managing Protected Health Information (PHI), but did not impact the reporting/claiming codes. On October 16, 2003, all health care providers throughout the USA are required to implement the HIPAA Transaction and Codes Sets rules or be able to demonstrate good faith efforts to that end. These rules require that providers of health care services anywhere in the USA must use nationally recognized Procedure Codes to claim services.
HIPAA Objectives and Compliant Coding Systems
One of the objectives of HIPAA is to enable providers of health care throughout the country to be able to be conversant with each other about the services they were providing through the use of a single coding system that would include any service provided. In passing HIPAA, Legislators were also convinced that a single national coding system would simplify the claims work of insurers of health.
STRUCTURE OF GUIDE
Activity: Title of the procedure code which defines the activity the practitioner provided.
Method of Delivery: Identifies the allowable ways in which the practitioner may conduct the activity.
In person
Telephone
Telehealth
N/A
Service Contact: Identifies the allowable person or persons for whom the practitioner may claim their time
of contact. The Service Contact may or may not be the client, but all claimed services must ultimately be
directed toward serving the client.
Client
Significant Support Person
N/A
Service Function Code (SFC): Utilized for Cost Report information systems, identifies the specific type of
service provided under a Mode of Service. Service Function Codes are necessary for classifying services
provided and service cost data at a specific level.
Allowable Discipline(s): Identifies the disciplines permitted to use the procedure code as well as the applicable taxonomies associated with that discipline. Not all staff listed in the Allowable Discipline(s) column may claim to Medicare and/or other private insurance. Refer to Discipline/Categories/Taxonomies Section for additional information about allowable disciplines.
Other Items:
Except for those services funded entirely by CGF or Mental Health Services Act (MHSA), there are no codes that identify payer information, such as PATH. Payer information will be maintained by funding plan/funding source.
Medicare does not reimburse for travel and documentation time, so in order to appropriately claim to both Medicare and Medi-Cal total service time for the Practitioner must be broken out into face-to-face and other time for most services. Face-to-face time is the time spent providing a service directed towards the client with the client present.
Only the psychotherapy codes are selected based on face-to-face time.
Psychological Testing, Evaluation & Management Medication Support Services and Group Services (with the exception of Collateral Group) all require face-to-face time.
No other Mental Health, Medication Support, or Targeted Case Management Services require face-to-face time, but if it occurs, it should be indicated.
Collateral and No-Contact – Report Writing should always be reported with “0” face-to-face time.
Face-to-face time is always “0” for telephone contacts.
Telemental health services are considered face-to-face given that the client is visually present.
These services are claimed in minutes or days...
Los Angeles County Department of Mental Health
Effective May 28, 2021
INTRODUCTION
This Guide, prepared by DMH, lists and defines the compliant codes that DMH believes reflects the services it provides throughout its system, whether by directly-operated, contracted organizational providers, or individual/group network providers. This analysis does not, however, absolve Providers, whether individuals or agencies from their responsibility to be familiar with nationally compliant codes and to inform and dialogue with DMH should they believe differences exist.
Brief History
Since the inception of the DMH’s first computer system in 1982, DMH directly-operated and contract staff have reported services using Activity Codes. These Activity Codes were then translated into the types of mental health services for which DMH could be reimbursed through a variety of funding sources. On April 14, 2003, health care providers throughout the Country implemented the HIPAA Privacy rules. This brought many changes to DMH’s way of managing Protected Health Information (PHI), but did not impact the reporting/claiming codes. On October 16, 2003, all health care providers throughout the USA are required to implement the HIPAA Transaction and Codes Sets rules or be able to demonstrate good faith efforts to that end. These rules require that providers of health care services anywhere in the USA must use nationally recognized Procedure Codes to claim services.
HIPAA Objectives and Compliant Coding Systems
One of the objectives of HIPAA is to enable providers of health care throughout the country to be able to be conversant with each other about the services they were providing through the use of a single coding system that would include any service provided. In passing HIPAA, Legislators were also convinced that a single national coding system would simplify the claims work of insurers of health.
STRUCTURE OF GUIDE
Activity: Title of the procedure code which defines the activity the practitioner provided.
Method of Delivery: Identifies the allowable ways in which the practitioner may conduct the activity.
In person
Telephone
Telehealth
N/A
Service Contact: Identifies the allowable person or persons for whom the practitioner may claim their time
of contact. The Service Contact may or may not be the client, but all claimed services must ultimately be
directed toward serving the client.
Client
Significant Support Person
N/A
Service Function Code (SFC): Utilized for Cost Report information systems, identifies the specific type of
service provided under a Mode of Service. Service Function Codes are necessary for classifying services
provided and service cost data at a specific level.
Allowable Discipline(s): Identifies the disciplines permitted to use the procedure code as well as the applicable taxonomies associated with that discipline. Not all staff listed in the Allowable Discipline(s) column may claim to Medicare and/or other private insurance. Refer to Discipline/Categories/Taxonomies Section for additional information about allowable disciplines.
Other Items:
Except for those services funded entirely by CGF or Mental Health Services Act (MHSA), there are no codes that identify payer information, such as PATH. Payer information will be maintained by funding plan/funding source.
Medicare does not reimburse for travel and documentation time, so in order to appropriately claim to both Medicare and Medi-Cal total service time for the Practitioner must be broken out into face-to-face and other time for most services. Face-to-face time is the time spent providing a service directed towards the client with the client present.
Only the psychotherapy codes are selected based on face-to-face time.
Psychological Testing, Evaluation & Management Medication Support Services and Group Services (with the exception of Collateral Group) all require face-to-face time.
No other Mental Health, Medication Support, or Targeted Case Management Services require face-to-face time, but if it occurs, it should be indicated.
Collateral and No-Contact – Report Writing should always be reported with “0” face-to-face time.
Face-to-face time is always “0” for telephone contacts.
Telemental health services are considered face-to-face given that the client is visually present.
These services are claimed in minutes or days...
Understanding Coding and Payment for Psychiatrists’ Services: How We Got Here and Where We’re Going
Naakesh A. Dewan, M.D., Ronald M. Burd, M.D., Allan A. Anderson, M.D., M.B.A., Eileen S. Carlson, R.N., J.D., Gregory G. Harris, M.D., M.P.H., Ellen Jaffe, Jeremy S. Musher, M.D., and Rebecca K. Yowell
Focus (Am Psychiatr Publ). Fall 2018; 16(4): 407–414.
The APA Committee on RBRVS, Codes, and Reimbursement authored this article to help psychiatrists gain a better understanding of the current coding and reimbursement structure for psychiatric services, including how it evolved and what the future holds.
Abstract
Psychiatrists often have difficulty understanding how to document, code, and bill for their services in a way that expedites adequate payment and avoids billing problems or future issues. This is very understandable because many psychiatrists in small or solo practices do their own billing without any formal training in the vagaries of coding and reimbursement policies. For many years, the American Psychiatric Association (APA) has devoted substantial resources to guiding psychiatrists through this maze, with direct member assistance and resources publicly available at www.psychiatry.org. APA staff, councils, and committees have also been working for many years to improve coding and reimbursement for psychiatric services. Current and former members and staff of the APA Committee on RBRVS, Codes, and Reimbursement have authored this article to help psychiatrists gain a better understanding of the current coding and reimbursement structure for psychiatric services, including how it evolved and what the future holds.
At the time of its inception in 1966, Medicare based physician payment on “customary, prevailing, and reasonable” charges (Figure 1). Physician payments were—and still are—covered under Medicare Part B, and hospital charges were and are covered under Part A, with separate rules for each.
Over the 25 years that followed, paying physicians on the basis of the amorphous idea of what was “customary, prevailing, and reasonable” created a number of problems, including inconsistent reimbursement patterns and policies, unsustainable growth in program costs, wage and price freezes put in place to stanch these costs, and a general compensation structure that overvalued new technology and procedures while devaluing the traditional care of increasingly complex patients.
1980s
In the mid-1980s, policy makers considered a variety of solutions to controlling the escalating cost of Part B payments, which eventually included the concept of a relative value scale (RVS). Although there was no absolute metric for all medical services, there was consensus among physicians that one service could be compared with another and found to be relatively more or less difficult. Policy makers had some experience with establishing the relative values of medical services by application of this concept, especially in California. Eventually, this scale came to include both the resources associated with delivering the service and the difficulty of the work, which allowed magnitude comparison among various services. Although this concept has reasonable face validity within services provided by a single specialty, there are doubts about validity when the service is provided by multiple specialties and even greater difficulties when comparisons are sought among different services provided by different specialties.
In 1985, a national study of Medicare reimbursement was undertaken at Harvard University, funded by the Health Care Financing Administration (HCFA; now known as the Centers for Medicare and Medicaid Services [CMS]). The study involved a resource-based relative value scale (RBRVS). Phase 1 of the study was completed in 1988, and a report was submitted to HCFA (1), with relative value units (RVUs) for the work of physicians in each medical service covered by Medicare. Psychiatry was one of the 18 specialties that participated in phase I to establish these values.
More about RVUs What Are RVUs? - AAPC
In 1989, Congress enacted the Omnibus Budget Reconciliation Act (OBRA) (2). It mandated that, beginning in 1992, Medicare payments would be based on an RBRVS. In 2000, the RBRVS was expanded to account for practice expenses (in practice expense RVUs) and the cost of malpractice and professional liability insurance (in professional liability RVUs), along with the level of physician work RVUs.
The sum of these three RVUs is the total RVUs for each code. This total represents a ratio or percentage, which is multiplied by the conversion factor for that year. In this manner, reimbursement rates are readjusted each year, even when the service RVUs have not changed. There are separate facility rates for services in hospitals and other facilities, and there are nonfacility rates for services in physician offices and other nonfacility settings. In addition, a geographic adjustment (the geographic practice cost index), applied to the total RVUs, accounts for regional variations in the costs of providing services. The OBRA required that each Current Procedural Terminology (CPT) code be reviewed at least every five years (in a five-year review) to correct any errors and to take into account any changes in technology or practice changes and any other events that would require adjustments.
1997
In 1997, as part of the Balanced Budget Act (3) of that year, Congress established something called the sustainable growth rate (SGR) in an attempt to control the growth in spending for physician-based services; no such law was passed for the hospital-based services. The SGR mandated that a Part B spending target be established each year on the basis of the gross domestic product. If more Part B services are being used, then the conversion factor for the next year’s fees (the number multiplied by the RVUs assigned to each service to determine the Medicare payment) must go down.
The SGR ignores all the drivers of demand for physician-based services that might account for an increased demand. This budgetary limit creates a “zero sum game,” whereby when the codes change in value or codes are added, the number of work RVUs in place changes, and the conversion factor, which establishes how much an RVU is worth, must also change to maintain neutrality. When the total of RVUs increases in number and value, the conversion factor goes down. This set up an annual intervention by Congress whereby every year since 2003 Congress passed a law to override what would have been a negative adjustment to the conversion factor. The “doc fix” ensured that physician income for Part B services would remain stable but did nothing to address the mounting debt associated with the increase in spending, which would need to be repaid at some unknown date in the future, by some unknown method.
2015
In April 2015, Congress passed the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) (4), which established a new way to determine payments to physicians. The MACRA repealed the flawed SGR formula that triggered deep cuts in payments for physician services, year after year. In its place, the law requires annual, across-the-board “updates” in Medicare Part B payments, which generally equate to a modest annual increase or at least a freeze of current rates. In addition, the MACRA replaced current quality-reporting programs with a new Merit-Based Incentive Payment System (MIPS), which provides upward or downward payment adjustments, depending on performance, as well as bonuses for participation in certain alternative payment models (APMs). The changes are designed to reward physicians for demonstrating a high level of quality of care or participating in new models of care that reward quality and efficiency.
The current codes and reimbursement rates for psychiatric and mental health services were adopted in 2013 and implemented in 2014, and they fundamentally transformed the business of psychiatric practice. Under Medicare Part B, physician work is codified (Figure 2) according to the American Medical Association’s (AMA’s) CPT (5), which provides the taxonomy used to document medical services provided in the United States. The CPT editorial panel develops codes that describe and delineate specific health services provided by individual clinicians (Figure 3). The codes for each year appear in the annual CPT Codebook, issued by the AMA.
The AMA issued the first CPT codes in 1966, and CMS adopted these in 1983 as the basis for reporting physician services under Medicare. Initially, these codes included only services by physicians. In 1997, however, these codes came to include the services of nonphysicians, including psychologists, social workers, occupational therapists, podiatrists, chiropractors, and others. The Health Insurance Portability and Accountability Act of 1996 (6) mandates that claims for all medical services must be submitted with CPT codes. The CPT editorial panel meets three times a year, taking input from specialty societies for new codes and revising the code structure to more accurately describe medical services as they are currently provided. More information about the CPT process and editorial panel is available on the AMA website at https://www.ama-assn.org/search/ama-assn/CPT.
New procedures often begin as Category III codes, temporary tracking codes to describe new work or new technology. Once practitioners have sufficient experience with the Category III code, it can be reviewed by the CPT Editorial Panel and designated a Category I, or a standard CPT code. The values of category III codes are set by the individual Medicare contractors (“carrier pricing”), whereas the values of Category I CPT codes are set by the CMS on the basis of multiple sources of information including recommendations from the AMA/Specialty Society Relative Value Scale (RVS) Update Committee (RUC) (see below).
The codes within CPT contain a large category of evaluation and management (E/M) codes. The E/M codes are further grouped by site of service, whether a patient is new or established, and the level of intensity or complexity of the service delivered. There are also more than 7,000 CPT codes for specific surgical and nonsurgical procedures, as well as codes for medical interventions. For example, these include the codes for electroconvulsive therapy (ECT) and transcranial magnetic stimulation (TMS). Many codes for surgical procedures bundle together the hospital days and the outpatient testing and follow-up appointments that occur within a particular “global period.” The global periods are generally 90 days, 30 days, or even 0 days (when all relevant services occur the same day).
Two specific observations are worth mentioning at this point. The first is that the CPT codebook directs the provider to “select the name of the procedure or service that accurately identifies the service performed. Do not select a CPT code that merely approximates the service provided. If no such specific code exists, then report the service using the appropriate unlisted procedure or service code” (5). The second is that the CPT codes are intentionally crafted not to be provider or specialty specific (e.g., the code for ECT does not specify that it should be administered by a psychiatrist).
The Process of Valuing Services
Codes enter the CPT or RUC process through several doors. First, the CPT editorial panel describes a new procedure (e.g., TMS), then eventually through the RUC process, the specialty society providers determine where the work of the new procedure fits compared with other, previously valued procedures. Many existing codes are reviewed at the request of CMS, according to several “screens” developed by the RUC or CMS or even required by Congress. The purpose of these is to identify codes that may be misvalued. One example of a screen is rapid growth in the total utilization of a code. A society may bring a code forward for review, but it must provide proof that the code was previously misvalued and must meet the “compelling evidence” standards of the RUC before a review of the code is even considered. Individuals can also request review of specific codes by sending a request to CMS.
The RUC was established in 1991 to recommend values to CMS for new and revised codes (Figure 4). The RUC generally meets three times a year, usually in January, April, and October. Special meetings may be called as well. The membership of the RUC includes representatives appointed by major national specialty societies, including the American Psychiatric Association (APA). Of the 31 voting RUC members, 21 are appointed in this manner, and four are elected to rotating seats. The remaining six seats include the RUC chair; the cochair of the Health Care Professionals Advisory Council (HCPAC), which represents nonphysician practitioners; the chair of the Practice Expense Subcommittee; and representatives of the AMA, the American Osteopathic Association, and the CPT editorial panel. Representatives from CMS also attend the RUC meetings as nonvoting guests. Additional information about the RUC composition, process, and procedures is available on the AMA website at https://www.ama-assn.org/practice-management/rbrvs-resource-based-relative-value-scale.
The RUC develops recommended values for codes and submits these recommendations to CMS. CMS staff review the recommendations as they prepare the next year’s Medicare physician fee schedule; decide which to adopt and which to reject or tweak; and then finalize the RVUs as part of the Final Rule, which is released in late fall each year. This advisory role for the RUC is intended to avoid a situation in which physicians might be seen to be setting their own prices. Federal antitrust law specifically prohibits the provider of a good or service who has a monopoly from setting the price for that good or service—and physicians are defined as having such a monopoly.
The RUC Advisory Committee is made up of advisors from the 118 specialty societies that are part of the AMA House of Delegates. The role of the RUC advisor (often working along with an RVS committee within his or her specialty) is to advise and help develop recommendations for consideration by the RUC for the work values, times, and practice expenses of new and revised codes as well as codes that have been identified as being misvalued or in other screens applied by CMS or the RUC. As codes come up to be valued or revalued, the RUC queries each of the societies as to their level of interest in participating in the valuation process. Those societies whose members perform the services may participate in a survey process and present recommendations to the RUC, help inform that process, or opt not to participate at all.
The RUC members appointed by the specialty societies to sit at the table and deliberate valuation proposals are not allowed to advocate for their particular specialty or society. Rather, they serve as impartial participants who thoughtfully consider, as physicians, the recommendations being presented to ensure that the codes are fairly valued relative to existing services. The specialty societies’ advisors, conversely, are the advocates, presenting valuation proposals for formal review by the RUC and making the case for valuation in front of the voting RUC representatives.
The survey process, conducted by the specialty societies whose members will be using the codes, includes the work of developing a “vignette” (description of the service and a typical patient) for each code under review, identifying a random sample of the specialty to be surveyed on this code, developing a list of services (by CPT code) that are similar to the work under review (which helps in determining a relative value), and administering the survey. The AMA RUC staff have developed a standard RUC survey instrument. The RUC Research Subcommittee is charged with review and approval of changes to the standard RUC survey, so the subcommittee may be involved if problems are anticipated.
The purpose of the survey is to get data on the time and effort it takes to do the work described in treating the typical patient. This includes identifying a service that is similar to the one being surveyed and comparing the two. Once the survey results are back, the societies prepare recommendations for the RUC, typically including time spent on patient care before the provider sees the patient (preservice time), during the actual visit (intraservice time), and after the visit concludes (postservice time), as well as hospital visits, outpatient visits, and work RVU for the service in question. The societies also prepare recommendations for the practice expense, which includes expenses for staff and supplies. The AMA RUC staff require prior approval of education regarding the RUC survey process for potential survey participants.
The RUC is charged with making recommendations on valuation proposals for services provided by physicians. (The HCPAC is composed of representatives of specialty societies for nonphysician practitioners who may be enrolled in Medicare. One of the HCPAC cochairs is from the AMA. The HCPAC considers and makes recommendations regarding valuation proposals for services performed exclusively—or primarily—by nonphysician Medicare providers.)
Prior to each RUC meeting, the valuation proposals for each group of codes are organized into a “tab” that is assigned to two or three RUC members for review and comment. As the RUC meeting begins, the first presentation for that tab is made to the Practice Expense Subcommittee, which goes over a line-by-line accounting of clinical staff and supply expenses for each code under consideration. After that, presenters for each tab (often the RUC advisors of the interested societies) make their way to the table and present their recommendations to the RUC on physician work on each code. The RUC members assigned to review that tab lead the discussion of the code, including making comments or asking questions about the data that were presented. All 31 voting RUC members participate in this process, having previously received not only the recommendations of the societies but also the reviewer’s comments. Eventually the RUC votes regarding whether to accept the society’s recommended values.
If the time and work recommendations pass, then the chair of the Practice Expense Subcommittee presents his or her recommendations for practice expenses, which the full RUC also votes on. If the time and work recommendations fail, they are often assigned to a facilitation committee, and each member of the RUC is asked to submit written comments and recommendations to facilitate an appropriate valuation. Each facilitation committee is composed of a number of RUC members (and experienced RUC advisors) who meet with the presenters and take into account the RUC’s written comments to craft a recommendation for the RUC to reconsider. The facilitation committee chair presents a report to the entire RUC, detailing the committee’s recommendations, which the RUC then votes on. Following acceptance of the facilitation committee report, the RUC votes on the practice expense recommendation.
The RUC uses a variety of methods in developing its recommendations. The most important is the survey. The RBRVS at the heart of Medicare physician payment by its nature requires comparison of the relative value of new (and revised) codes for services, as compared with existing codes and services. The fundamental concept behind valuation is magnitude estimation, which basically compares the code under review and determines whether it is bigger or smaller or how much more or less it is worth than services that have been valued previously.
A method that the surgical societies have used frequently is the intensity of work per unit of time. This calculation creates a number as a surrogate for an intensity measure. It appears to be valid when one compares similar services within the same family but presents challenges when used across families, particularly because some services actually have a negative number. Comparing the values of different codes is particularly problematic if they have different (or no) global periods. In addition to the ongoing workload of valuing individual codes, the RUC members, subcommittees, and participating societies have also been involved in developing and discussing alternative valuation methodology, alternative physician payment models, and other emerging issues.
As the ultimate decision maker regarding the Medicare valuation of physician services, CMS has an integral, although not always transparent, role in this process (Figure 5). As a payer, CMS is accountable to ensure that the services billed for were provided. Although the CPT editorial panel established the framework for the E/M codes, CMS published specific E/M documentation guidelines in 1995 to enable auditors to determine whether the service for the particular charge had actually been delivered. The guidelines established eight elements for defining the depth of a history taken, specifically delineated the elements that constituted a comprehensive exam, and provided a method for quantifying the degree of the cognitive work (medical decision making) required for the code.
CMS defined the elements of the history, which are not unfamiliar to physicians but unfortunately do not always translate well into the work of psychiatry. They include location, duration, quality, severity, timing, context, modifying factors, and associated signs and symptoms. A high-level history requires four of the above elements or comments on three chronic conditions the patient has.
In the 1995 CMS guidelines for a comprehensive examination, the highest level only acknowledged a general physical exam, which was problematic for many specialties (including psychiatry) because it included elements (breast, pelvic, and rectal) not appropriate to the specialty. CMS attempted to correct for this problem by publishing new guidelines in 1997 that defined single-system examinations for specialties that could be used to fulfill the requirements for a comprehensive examination. The structure of these single-system exams is similar, with all including vital signs and general appearance, after which they narrow slightly. The single-system psychiatry exam includes elements of the neurologic and musculoskeletal exam as well as elements specific to psychiatry (e.g., hallucinations and delusions).
"Elements of Psychiatric Examination:
- Description of speech including: rate; volume; articulation; coherence; and spontaneity with notation of abnormalities (eg, perseveration, paucity of language)
- Description of thought processes including: rate of thoughts; content of thoughts (eg, logical vs. illogical, tangential); abstract reasoning; and computation
- Description of associations (eg, loose, tangential, circumstantial, intact)
- Description of abnormal or psychotic thoughts including: hallucinations; delusions; preoccupation with violence; homicidal or suicidal ideation; and obsessions
- Description of the patient’s judgment (eg, concerning everyday activities and social situations) and insight (eg, concerning psychiatric condition)
- Orientation to time, place and person
- Recent and remote memory
- Attention span and concentration
- Language (eg, naming objects, repeating phrases)
- Fund of knowledge (eg, awareness of current events, past history, vocabulary) Mood and affect (eg, depression, anxiety, agitation, hypomania, lability)
Unfortunately, the structure of the psychiatric specialty examination, as described in the CMS documentation guidelines, is not consistent with the way most psychiatrists conceptualize psychiatric function. The guidelines specify how many of the elements listed must be included for the exam to be defined as limited, detailed, or comprehensive, whether or not those specific elements are pertinent to the problem at hand. Despite this, CMS, as well as the AMA and other specialty societies, has been resistant to restructuring the psychiatric specialty examination, out of concern that to do so would precipitate a wholesale revision of the E/M codes.
Attempting to quantify the medical decision making has been even more problematic. The current model identifies three dimensions that determine the difficulty of the medical decision making. These are
- the nature and number of problems or management options,
- the quantity and complexity of data, and
- the risk of the intervention.
Although the E/M codes have, in concept, been available for psychiatrists to use since their inception, they generally were not used in outpatient care before 2013, in part because many states and payers did not include them in the fee schedules for psychiatrists. Historically, psychiatric services were bundled together, which resulted in a small number of CPT codes to describe psychiatric services (7). For example, one of the earliest CPT codes, 90841 (individual medical psychotherapy by a physician, with continuing medical diagnostic evaluation, and drug management when indicated, including insight oriented, behavior modifying or supportive psychotherapy; time unspecified) included four different services (psychotherapy, medical diagnostic evaluation, psychiatric evaluation, and drug management). This provided a limited number of options for psychiatrists billing their services.
As a result of this structure, psychiatrists were not allowed to bill for an E/M service and a psychotherapy visit on the same day. Instead, they had the option of billing for “medical psychotherapy” or a medication management service, depending on the nature of the work (8). Early revisions included adding timeframes to the codes. These codes were quite basic: 90801 for initial evaluations, 90843 for services of 20–30 minutes, and 90844 for services of 45–50 minutes.
In 1995, as part of the regular RUC review process at the time, APA requested a review of the codes in the psychiatry section on the basis of the vast changes in work that had occurred since the codes were initially valued. HCFA was moving to incorporate all professional services, including those of psychologists and social workers, in the Medicare physician fee schedule and “asked” APA to include those groups in any survey process. A joint survey was completed, (although not without APA voicing concerns), and the recommendations, which included an increase in RVUs for five services, were put forward to the RUC. HCFA, however, dismissed the compelling evidence arguments and declined to adopt the changes.
Following significant advocacy by the APA, CMS introduced a series of Healthcare Common Procedure Coding System (HCPCS) codes beginning with the letter G (G-codes), to take effect in January 1997, that provided greater granularity. These codes divided up the work by site (inpatient versus outpatient), duration of service, and whether E/M services were delivered (Figure 6). Psychologists and social workers would no longer be able to bill the medical psychotherapy codes but rather would bill a psychotherapy code that did not include any medical evaluation or medical management services. The CPT codes (90804–90829) went to the RUC, and the standard procedure was launched to determine appropriate recommendations for the valuation of the new codes.
Unfortunately for psychiatry, the results of the surveys undertaken to determine value were not particularly helpful. Survey respondents not only were unfamiliar with the survey tool, they also were unfamiliar with the new coding structure and the codes they used for comparison. Also, the surveying groups (psychiatrists, psychologists, and social workers) did very different kinds of work and saw very different patients from one another. Nonetheless, the expectation was that a recommendation be made, so, by a methodology of regression analysis, values were determined, recommended to, and accepted (with some reductions) by CMS, and they became the standard with the 1999 Medicare physician fee schedule.
As time passed, it became apparent to psychiatrists that the value of the codes used by psychiatrists and other mental health providers was slowly drifting down. This was occurring due to the fixed sum for physician services under Medicare, such that for every new procedure valued or increase in the value of an existing service, the conversion factor applied to all other codes (including the extant psychiatric codes) decreased. Furthermore, increases in the value of the E/M codes distorted the original crosswalk that had existed between the E/M codes and the codes most frequently used by psychiatrists. Another development was increasing concern that the code most frequently used by psychiatrists (90862, medication management) was overvalued and should be resurveyed.
In anticipation of the 2010 five-year review of RVUs and the opportunity presented to address the misvaluation, the board of trustees of the APA approved efforts by the Committee on RBRVS, Codes, and Reimbursement to seek change. Representatives of APA, the AACAP, the American Psychological Association, the National Association of Social Workers, the American Nurses Association, and the American Psychiatric Nurses Association met and determined to have those procedure codes representing their work included in that review. They drafted a group letter to CMS laying forth their case of compelling evidence that the codes had been inappropriately valued.
CMS agreed to a review by the RUC. That review started at the research committee of the RUC, which recommended to the RUC that instead of just a revaluation of the existing codes, the entire family of psychiatric procedure codes should be referred back to CPT to be restructured. The RUC agreed to that recommendation and moved the family of codes to CPT for restructuring.
Within weeks, a CPT work group had been formed to begin this work, with representatives from the CPT editorial panel and of the groups noted above. The group struggled to define parameters measuring the specifics of work done by mental health practitioners that would not create onerous documentation requirements. When the chair of the original work group was given a new assignment, the work group was dissolved, and a new work group formed with new leadership. This new group struggled with the same issues as the previous one but eventually was able to craft a compromise framework that was accepted by CPT.
This compromise saw the elimination of 90862 and the separation of the diagnostic evaluation into two new initial evaluation codes, including one that included the assessment of the patient’s medical (physical health) status, differentiating between physician and nonphysician work. In addition, different methodology was now used for defining the E/M work and psychotherapy work in a psychiatric encounter, with the use of the standard physician E/M codes to record the E/M work and an “add-on” psychotherapy code. (An add-on code is a service that is always performed with another service and must never be reported as a stand-alone code. In this case, the primary service is an E/M service, and the psychotherapy is considered secondary for coding purposes.) Other additions included an interactive add-on code, codes for crisis interventions, and a code that those few psychologists licensed to prescribe could use when prescribing (in states with scope-of-practice laws permitting this).
The new codes were sent from the CPT editorial panel to the RUC to be valued, and the APA and other mental health provider societies began their work, as described above. Dr. Jeremy Musher was the spokesperson for the APA at CPT and led the presentations at the RUC on both practice expense and work and time recommendations. The family of codes went through prefacilitation, and, in the end, the values for the codes were approved as the societies had recommended.
The RUC recommendations were forwarded to CMS for consideration as they reviewed valuations for the 2013 Medicare physician fee schedule. CMS chose not to accept the value recommendations for 2013, citing that the entire family had not yet been surveyed. Instead, for 2013 CMS created interim values for the new code structure.
Unfortunately, when they did so, they did not apply consistent logic, especially regarding practice expense. The components included in the practice expense values had recently been revisited for all societies through an AMA survey. The survey results showed that psychiatrists did not “typically” (defined as more than 50% of the respondents) have clinical staff in their offices. Given the nature of the services provided, psychiatrists have limited medical equipment and medical supplies in their offices. Costs attributed to work performed by clinical staff were the largest component of the practice expense values up to this point.
Unable to combat the AMA survey results, the RUC stripped that category from the values, and substantially lower practice expense values were attributed to psychiatric services. CMS chose to add those new, lower practice expense values to the new psychiatric initial evaluation with medical services (90792). However, the old, higher practice expense values continued to be attached to the new nonmedical initial evaluation, which resulted in a greater value for the nonmedical code. All attempts by the APA to have this corrected failed, and this anomaly ended up in the Final Rule for 2013.
The remaining codes were surveyed in 2013, which enabled CMS to go forward with final values for all of the codes. Late in 2013, the Final Rule for 2014 was released, and the values recommended by the RUC that the APA and its partners had championed were now applied by CMS, with one exception. CMS chose not to value or cover the CPT code for pharmacologic management when done by a psychologist.
The timeframe of these changes was no different than for other coding changes that occur every year. However, the private payers struggled to implement the new fee schedule in 2013 because of the extent and nature of the change in the coding framework. The APA’s board of trustees continues to direct current activities in this area, including the continued efforts of the APA Committee on RBRVS, Codes, and Reimbursement regarding new codes, ongoing efforts by the committee to educate members about coding changes and correct coding and documentation, work done directly with payers regarding payment policy, and the consideration of potential legal action to prevent payer policies that violate federal laws requiring parity between payment for mental health and medical services.
The Future
For a number of years, we have been hearing about the paradigm shift in the way physician and other medical services are provided to patients as well as the way such services will be reimbursed. When physicians try to redesign the ways they deliver services to provide higher quality patient care at a lower cost, they find that barriers in current payment systems prevent them from doing so. Barriers include the lack of payment or inadequate payment for high-valued services and financial penalties for delivering a different mix of services.
Alternative payment models (APMs) can provide a way of overcoming the barriers in current payment systems so that physicians can deliver higher quality care for patients at lower costs for purchasers in ways that are financially feasible for physician practices. Characteristics of successful APMs include flexibility in care delivery, adequacy of payment, and accountability for costs and quality. MACRA encourages the creation of APMs and provides incentives for physicians to participate in them. MACRA explicitly encourages the development of “physician-focused payment models,” with no single approach that will work for all physicians and for their patients.
APMs span condition-based payment, multispecialty bundled payment, physician-facility bundled payment, and episode payment for a procedure. (APM obejmują płatność uzależnioną od stanu, opłatę łączoną wielospecjalistyczną, opłatę łączoną między lekarzem a placówką oraz opłatę za odcinek za zabieg.) The hope is that APMs will allow recognized savings through reduction of emergency department visits and hospital admissions, reduction of unnecessary tests and treatments, more efficient service delivery, use of lower cost sites of service, and the prevention of serious conditions. If APMs are constructed well, we should see savings for the payer and increased physician practice revenue.
With MACRA legislation, CMS has enacted bonus reward systems and penalties. Physicians who are qualifying participants in accountable care organizations (ACOs) and certain other qualifying APMs are rewarded with bonuses and higher annual updates. It should be noted that not all ACOs have been effective, and many have ceased to function. MACRA offers physicians a choice between two payment pathways: a new quality program known as the MIPS that offers substantial bonuses for high performance, or involvement in an “advanced” APM, such as an ACO. The majority of practicing psychiatrists likely fall under the MIPS provision.
Most psychiatrists who participate in Medicare and cross the threshold, in terms of either absolute number of Medicare-insured patients or annual income from Medicare, need to meet the components of MIPS to avoid penalties, unless they meet the qualifications for being in an acceptable APM. MIPS has four components: quality reporting (formerly the Physician Quality Reporting System), cost (formerly the value-based payment modifier), advancing care information (formerly meaningful use), and the new category of improvement activities. Through a combination of weighting of these categories and addition of scores based on physician performance, there will be future increases or decreases in Medicare payments to physicians. Physicians who participate in advanced APMs do not have to participate with MIPS and will receive a 5% bonus from Medicare from 2019 through 2024, as well as higher annual updates in later years. The APA has been actively involved in creating a national mental health registry, known as PsychPRO, that will allow psychiatrists to participate. By doing so, they will meet many of the MIPS requirements to avoid penalties and to realize bonuses. PsychPRO has been approved by CMS for MIPS reporting as a qualified clinical data registry. Participation in PsychPRO is free to APA members.
APMs are already shaping psychiatric practice and the role of psychiatrists. There are now new billing codes (99492-99494) for collaborative care model (CoCM) services. These are for reimbursement of a team consisting of a primary care provider who submits the code, a behavioral health care manager employed by the primary care provider, and a consulting psychiatrist. The consulting psychiatrist contracts directly with the primary care provider. The psychiatrist provides regular case management through discussions with the care manager and, on occasion, directly with the primary care provider. There is the option for some direct face-to-face contact between the patient and the psychiatrist, and this service is billed separately. CMS approved codes for these services, as well as Medicare coverage and payment, starting in January 2017. For more information on these service, visit https://www.psychiatry.org/psychiatrists/practice/professional-interests/integrated-care/learn.
More than 80 randomized, clinical trials have demonstrated that care provided by this model improves access, improves quality of care, and decreases cost. Use of technology such as telemedicine may further expand this model. Certainly, other innovative models can be expected in the future. We are certainly entering a phase during which physicians and health systems will be challenged to provide cost-effective, evidence-based, high-quality patient- and population-based care.
Whatever the future holds, one trend that will likely continue is psychiatrists who select employment contracts, as opposed to a private practice model. With all of the implications of MIPS as well as the increasing complexity of navigating the system of payment for services, this may be a prudent choice. A challenge, however, is the dearth of psychiatrists and other physicians in leadership in larger organizations. It seems imperative to help guide those psychiatrists interested in administrative positions to engage in such leadership roles.
Footnotes
The authors are former and current members of the American Psychiatric Association (APA) Committee on RBRVS, Codes, and Reimbursement or are APA staff (Ms. Carlson, Ms. Jaffe, and Ms. Yowell). All authors are members of or advisors to the American Medical Association/Specialty Society RVS Update Committee.
The authors report no financial relationships with commercial interests.
Figures and Tables
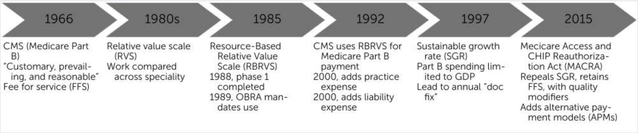
FIGURE 1.The Evolution of the Medicare Physician Payment
CMS, Centers for Medicare and Medicaid Services; OBRA, Omnibus Budget Reconciliation Act; GDP, gross domestic product.
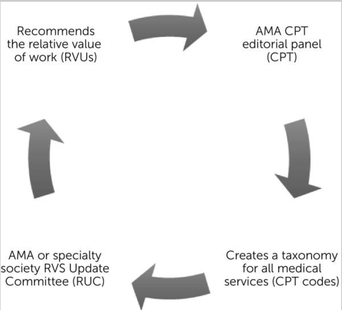
FIGURE 2.Role of Organized Medicine
AMA, American Medical Association; CPT, Current Procedural Terminology.
AMA, American Medical Association; CPT, Current Procedural Terminology.

FIGURE 3.Current Procedural Terminology (CPT) Codes and CPT Editorial Panel
CMS, Centers for Medicare and Medicaid Services; RUC, American Medical Association/Specialty Society Relative Value Scale Update Committee; RVU, relative value unit.
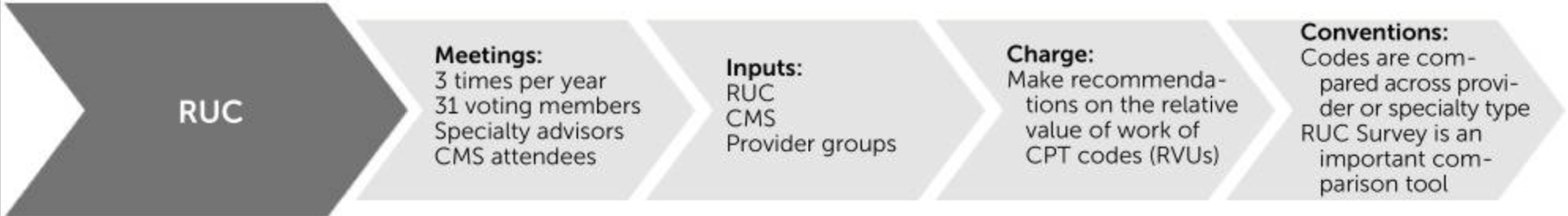
FIGURE 4.AMA/Specialty Society RVS Update Committee (RUC)
RUC, American Medical Association/Specialty Society Relative Value Scale Update Committee; CMS, Centers for Medicare and Medicaid Services; CPT, Current Procedural Terminology; RVU, relative value unit.
RUC, American Medical Association/Specialty Society Relative Value Scale Update Committee; CMS, Centers for Medicare and Medicaid Services; CPT, Current Procedural Terminology; RVU, relative value unit.

FIGURE 5.Integral Role of the Centers for Medicare and Medicaid Services (CMS) in Organized Medicine and Government Accountability E/M, evaluation and management; APM, alternative payment model; MACRA, Medicare Access and CHIP Reauthorization Act; FFS, fee for service.
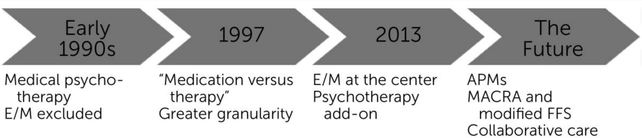
FIGURE 6.History of the Current Codes for Psychiatric and Mental Health Services
CMS, Centers for Medicare and Medicaid Services; CPT, Current Procedural Terminology; RUC, American Medical Association/Specialty Society Relative Value Scale Update Committee; RVU, relative value unit; E/M, evaluation and management.
ALTERNATIVE PAYMENT MODEL (APM) FRAMEWORK
the Work Group understands person centered care to mean high quality care that is both evidence based and delivered in an efficient manner, and where patients’ and caregivers’ individual preferences, needs, and values are paramount.
The Work Group believes that person centered care, so defined, rests upon three pillars:
• Quality: This term indicates that patients receive appropriate and timely care that not only is consistent with evidence based guidelines and patient goals, but also results in optimal patient outcomes and patient experience. Ideally, quality should be evaluated using a harmonized set of appropriately adjusted process, outcome, patient reported outcome, and patient experience measures that both provide an accurate and comprehensive assessment of clinical and behavioral health, and that report results that can be meaningfully accessed, understood, and used by patients and consumers.
• Cost Effectiveness: This term indicates a level of severity adjusted total costs (and, when relevant, unit prices) that reflect benchmarked best achievable results, and that are consistent with robust and competitive health insurance marketplaces as characterized by the deployment of multiple affordable, attractive products across employer group, individual commercial, and government programs sectors. Care that is less expensive than expected, but that results in poor clinical outcomes, is not considered cost effective. Conversely, care that is costly but that results in dramatic improvements in patient outcomes could be considered cost effective. Affordable health care services are vital to ensuring that the nation can support investments in education, housing, and other social determinants that can independently improve population health.
• Patient Engagement: This term encompasses the important aspects of care that improve patient experience, enhance shared decision making, and ensure that patients and consumers achieve their health goals. Patient engagement should occur at all levels of care delivery, with patients and caregivers serving as partners when setting treatment plans and goals at the point of care; when designing and redesigning delivery and payment models; on governance boards and decision making bodies; and when identifying and establishing connections to social support services. Engaged patients and consumers are informed of their health status and share in their own care; they are easily able to access appointments and clinical opinions; they seek care at the appropriate site; they possess the information they need to identify high value providers and to tailor treatment plans to individual health goals; they provide ongoing feedback that providers can use to improve patient experience; they are able to obtain transparent price information about services and their value for patients and consumers; and they can move seamlessly among providers that are engaged in different aspects of their care. Routine communication with family caregivers and other support members is also a critical part of comprehensive, person centered care.
the Work Group understands person centered care to mean high quality care that is both evidence based and delivered in an efficient manner, and where patients’ and caregivers’ individual preferences, needs, and values are paramount.
The Work Group believes that person centered care, so defined, rests upon three pillars:
• Quality: This term indicates that patients receive appropriate and timely care that not only is consistent with evidence based guidelines and patient goals, but also results in optimal patient outcomes and patient experience. Ideally, quality should be evaluated using a harmonized set of appropriately adjusted process, outcome, patient reported outcome, and patient experience measures that both provide an accurate and comprehensive assessment of clinical and behavioral health, and that report results that can be meaningfully accessed, understood, and used by patients and consumers.
• Cost Effectiveness: This term indicates a level of severity adjusted total costs (and, when relevant, unit prices) that reflect benchmarked best achievable results, and that are consistent with robust and competitive health insurance marketplaces as characterized by the deployment of multiple affordable, attractive products across employer group, individual commercial, and government programs sectors. Care that is less expensive than expected, but that results in poor clinical outcomes, is not considered cost effective. Conversely, care that is costly but that results in dramatic improvements in patient outcomes could be considered cost effective. Affordable health care services are vital to ensuring that the nation can support investments in education, housing, and other social determinants that can independently improve population health.
• Patient Engagement: This term encompasses the important aspects of care that improve patient experience, enhance shared decision making, and ensure that patients and consumers achieve their health goals. Patient engagement should occur at all levels of care delivery, with patients and caregivers serving as partners when setting treatment plans and goals at the point of care; when designing and redesigning delivery and payment models; on governance boards and decision making bodies; and when identifying and establishing connections to social support services. Engaged patients and consumers are informed of their health status and share in their own care; they are easily able to access appointments and clinical opinions; they seek care at the appropriate site; they possess the information they need to identify high value providers and to tailor treatment plans to individual health goals; they provide ongoing feedback that providers can use to improve patient experience; they are able to obtain transparent price information about services and their value for patients and consumers; and they can move seamlessly among providers that are engaged in different aspects of their care. Routine communication with family caregivers and other support members is also a critical part of comprehensive, person centered care.
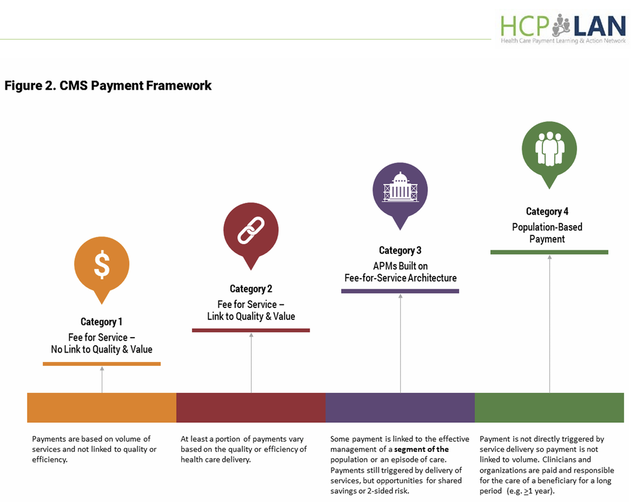
The CMS Framework assigns payments from plans to health care providers to four Categories, such that movement from Category 1 to Category 4 involves increasing provider accountability for both quality and total cost of care, with a greater focus on population health management (as opposed to payment for specific services).
1. Fee for Service with No Link to Quality & Value (Category 1):
Payment models classified in Category 1 utilize traditional FFS payments (i.e., payments are made for units of service) that are adjusted to account for neither infrastructure investments, nor provider reporting of quality data, nor for provider performance on cost and quality metrics. Additionally, it is important to note that diagnosis related groups (DRGs) that are not linked to quality and value are classified in Category 1. This is because the Work Group has determined that DRGs are used to reimburse a group of services delivered within a hospitalization, and while DRGs drive efficiencies in inpatient care, hospitals typically bill DRGs in much the same way that physicians bill services that are paid on a fee schedule. In both instances, the provider's incentive may be to bill for additional services because they are paid more for more volume.
Payments in Category 1 are distinguished from those in Category 2 in that the latter incentivizes infrastructure investments and/or involves some method of reporting or assessing the quality of the care delivered. Unlike payments made in Category 1, payments made in Category 2 are influenced by whether a provider invests in infrastructure, reports quality data, or achieves quality targets.
2. Fee for Service Linked to Quality & Value (Category 2):
Payment models classified in Category 2 utilize traditional FFS payments (i.e., payments that are made for units of service), but these payments are subsequently adjusted based on infrastructure investments to improve care or clinical services, whether providers report quality data, or how well they perform on cost and quality metrics.
The Work Group has split Category 2 into subcategories A, B, C, and D as outlined below:
• Payments placed into Category 2A involve payments for infrastructure investments that can improve the quality of patient care, even though payment rates are not adjusted in accordance with performance on quality metrics. For example, payments designated for staffing a care coordination nurse or upgrading to electronic health records would fall under Category 2A. Because investments in these and similar delivery enhancements will likely improve patient experience and quality of care, the Work Group considers these types of FFS or per member per month (PMPM) payments an important—though preliminary—step toward payment reform.
• Payments placed into Category 2B provide positive or negative incentives to report quality data to the health plan and—preferably—to the public. Providers may have initial difficulties reporting clinical data accurately. Participation in a pay for reporting program therefore gives providers an opportunity to familiarize themselves with performance metrics, build internal resources to collect data, and better navigate a health plan’s reporting system. Because pay for reporting does not link payment to quality performance, the Work Group maintains that participation in Category 2B payment models should be time limited and that participation in Category 2B payment models will often evolve into subsequent categories.
• Payments are placed into Category 2C if they provide rewards for high performance on clinical quality measures. Much like pay for reporting programs, pay for performance programs that only reward high performance on quality metrics give providers an opportunity to acclimate themselves to the applicable reporting systems and measures before they are subject to penalties for low performance. In some instances, these programs have an extensive set of performance measures that assess clinical outcomes, such as a reduction in emergency room visits for individuals with chronic illnesses or a reduction in a hospital acquired infections.
• Payments placed into Category 2D reward providers that perform well on quality metrics and/or penalize providers that do not perform well, thus providing a significant linkage between payment and quality. For example, providers may receive lower updates to their FFS baseline or may receive a percent reduction on all claims paid if they do not meet quality goals. (Please note that payments in this subcategory are not subject to rewards or penalties for provider performance against aggregate cost targets, but may take into account performance on a more limited set of cost measures.)
In addition to their capacity to stimulate and focus quality improvement initiatives, investments in quality performance assessment are also valuable because they can drive the development and expansion of health information technology (HIT). Although the Work Group was not tasked with developing specific recommendations on HIT and data sharing, it believes that providers should invest in interoperable systems; that administrative reporting requirements should be minimized as much as possible; that patients and caregivers should have free and ready access to patient records; and that HIT should be used to maintain patient registries and contribute to the development of clinical measures and guidelines.
Payments that fall under Category 2 are distinguished from those that fall under Category 3 in two respects. First, Category 2 payments do not involve arrangements in which providers assume either shared savings or shared losses based on established cost targets. Second, FFS based payments in Category 3 reflect, to a greater degree, care that is provided longitudinally, such that multiple providers are responsible for the cost and quality associated with a particular set of procedures or services. By contrast, Category 2 payments are limited to specific providers.
3 APMs Built on Fee for Service Architecture (Category 3):
Payment models classified in Category 3 are based on an FFS architecture, while providing mechanisms for the effective management of a set of procedures, an episode of care, or all health services provided for individuals. In addition to taking quality considerations into account (as in Category 2), Category 3 payments are based on cost performance against a target, irrespective of how the financial benchmark is established, updated, or adjusted. For APMs in Category 3, providers that meet their cost and quality targets are eligible for shared savings, and those that do not may be held financially accountable.
Additionally, payments in Category 3 are structured to encourage providers to deliver effective and efficient care. Episode based and other types of bundled payments encourage care coordination because they cover a complete set of related services for a procedure that may be delivered by multiple providers. Clinical episode payments fall into Category 3 if they are tied to specific procedures, such as hip replacement or back surgery.
The Work Group has split Category 3 into subcategories A and B as outlined below:
• Category 3A gives providers an opportunity to share in the savings they generate. If a provider participating in a Category 3A APM meets quality targets but does not meet cost targets, then the provider is not held financially responsible for excess spending.
• Payments in Category 3B involve both upside gainsharing (i.e., positive payment adjustments) and downside risk (i.e., negative payment adjustments) based on performance on cost measures.
The Work Group believes payments in Category 3 will advance clinical integration and affordability to a greater extent than payments in Category 2 because risk sharing arrangements provide stronger incentives to manage health care costs and reward care coordination across the span of care.
The most important distinction between Category 3 and Category 4 payments is that the latter (category 4) involve a single payment that encompasses a broad array of services, whereas providers participating in Category 3 models are eligible for only a portion of the losses and/or savings they generate. Additional conditions must be met before a payment model can be placed into Category 4. Specifically, Category 4 payments reflect the total cost of care for treating a primary (typically chronic) condition, or for maintaining the health and managing the illness of an entire population. By contrast, even if they are fully capitated, payments that cover a more limited set of specialty services (including primary care) would be classified in Category 3. For example, a Category 4 model for pediatric care would have to cover a wide range of medical, preventive, and developmental services, whereas a population based payment model for primary care would fall under Category 3 if it did not hold primary care providers accountable for care coordination and the appropriate utilization of specialty services. Similarly, clinical episode payments tied to conditions (e.g., diabetes or cancer) fall under Category 4, whereas clinical episode payments tied to procedures (e.g., hip replacement or back surgery) fall under Category 3, even if they are made on a per member per month basis. As such, Category 4 payments are more person focused, insofar as they include stronger incentives to promote health and wellness throughout the care continuum.
4. Population Based Payment (Category 4):
Payment models classified as Category 4 involve population based payments, structured in a manner that encourages providers to deliver well-coordinated, high quality person level care within a defined (4A) or overall (4B) budget. This holds providers accountable for meeting quality and, increasingly, person centered care goals for a population of patients or members. Payments within Category 4 are intended to cover a wide range of preventive health, health maintenance, and health improvement services, and these payments will likely require care delivery systems to establish teams of health professionals to provide enhanced access and coordinated care. Additionally, and in contrast to capitated arrangements in Category 4N, providers participating in Category 4A and 4B APMs are held accountable for delivering high quality, clinically necessary, and appropriate care.
The Work Group has split Category 4 into subcategories A and B as outlined below:
• Category 4A payments are limited to certain sets of condition specific services (e.g., asthma, diabetes, or cancer), but they remain person focused in the sense that they hold providers accountable for the total cost and quality of care related to that condition. For example, bundled payments for cancer care fall under Category 4A if providers are responsible for the total cost and quality of care for a patient, rather than covering only chemotherapy payments. The Work Group recognizes that in certain instances patient care will predominantly revolve around the management of particular types of conditions, such as cancer or heart disease. In such cases, we recognize that Category 4A may become a suitable and justifiable endpoint, especially for smaller provider organizations which may never be able to deliver certain types of care (such as transplants). Nevertheless, the Work Group maintains that providers should ideally be paid to maintain health and manage illness for an entire population, rather than compartmentalizing payments according to particular conditions. We also believe that condition specific payments should, in time, become part of a comprehensive approach to improving health and reducing costs for an entire population. For highly integrated delivery systems, the Work Group envisions that Category 4A payments will evolve into Category 4B.
• Payments in Category 4B are capitated or population based for all of the individual’s health care needs. Category 4B encompasses a broad range of financing and delivery system arrangements with varying degrees of integration between plans and provider groups. On one end of the spectrum, plans and providers in Category 4B models may be virtually integrated. On the other end of the spectrum are highly integrated arrangements that are characterized by vertical integration of financing and care delivery, common ownership, and strong linkage across strategy, clinical performance, quality, and resource use. These groups may also have a higher percentage of salaried physicians. After reviewing the literature and discussing these highly integrated arrangements with people who operate within them, the Work Group has reached the conclusion that they can be ideally suited for delivering person centered care because they:
1) force transformational thinking about delivery system reform;
2) optimize coordination of infrastructure investments;
3) most fully remove financial incentives for volume; and
4) expedite community investment and engagement.
Although the underlying payment approaches were not sufficiently distinct to warrant the creation of a separate subcategory for highly integrated payment and delivery systems, the Work Group believes that these arrangements yield key benefits and efficiencies, because they have a greater impact on organizational responses to quality and value incentives.
1. Fee for Service with No Link to Quality & Value (Category 1):
Payment models classified in Category 1 utilize traditional FFS payments (i.e., payments are made for units of service) that are adjusted to account for neither infrastructure investments, nor provider reporting of quality data, nor for provider performance on cost and quality metrics. Additionally, it is important to note that diagnosis related groups (DRGs) that are not linked to quality and value are classified in Category 1. This is because the Work Group has determined that DRGs are used to reimburse a group of services delivered within a hospitalization, and while DRGs drive efficiencies in inpatient care, hospitals typically bill DRGs in much the same way that physicians bill services that are paid on a fee schedule. In both instances, the provider's incentive may be to bill for additional services because they are paid more for more volume.
Payments in Category 1 are distinguished from those in Category 2 in that the latter incentivizes infrastructure investments and/or involves some method of reporting or assessing the quality of the care delivered. Unlike payments made in Category 1, payments made in Category 2 are influenced by whether a provider invests in infrastructure, reports quality data, or achieves quality targets.
2. Fee for Service Linked to Quality & Value (Category 2):
Payment models classified in Category 2 utilize traditional FFS payments (i.e., payments that are made for units of service), but these payments are subsequently adjusted based on infrastructure investments to improve care or clinical services, whether providers report quality data, or how well they perform on cost and quality metrics.
The Work Group has split Category 2 into subcategories A, B, C, and D as outlined below:
• Payments placed into Category 2A involve payments for infrastructure investments that can improve the quality of patient care, even though payment rates are not adjusted in accordance with performance on quality metrics. For example, payments designated for staffing a care coordination nurse or upgrading to electronic health records would fall under Category 2A. Because investments in these and similar delivery enhancements will likely improve patient experience and quality of care, the Work Group considers these types of FFS or per member per month (PMPM) payments an important—though preliminary—step toward payment reform.
• Payments placed into Category 2B provide positive or negative incentives to report quality data to the health plan and—preferably—to the public. Providers may have initial difficulties reporting clinical data accurately. Participation in a pay for reporting program therefore gives providers an opportunity to familiarize themselves with performance metrics, build internal resources to collect data, and better navigate a health plan’s reporting system. Because pay for reporting does not link payment to quality performance, the Work Group maintains that participation in Category 2B payment models should be time limited and that participation in Category 2B payment models will often evolve into subsequent categories.
• Payments are placed into Category 2C if they provide rewards for high performance on clinical quality measures. Much like pay for reporting programs, pay for performance programs that only reward high performance on quality metrics give providers an opportunity to acclimate themselves to the applicable reporting systems and measures before they are subject to penalties for low performance. In some instances, these programs have an extensive set of performance measures that assess clinical outcomes, such as a reduction in emergency room visits for individuals with chronic illnesses or a reduction in a hospital acquired infections.
• Payments placed into Category 2D reward providers that perform well on quality metrics and/or penalize providers that do not perform well, thus providing a significant linkage between payment and quality. For example, providers may receive lower updates to their FFS baseline or may receive a percent reduction on all claims paid if they do not meet quality goals. (Please note that payments in this subcategory are not subject to rewards or penalties for provider performance against aggregate cost targets, but may take into account performance on a more limited set of cost measures.)
In addition to their capacity to stimulate and focus quality improvement initiatives, investments in quality performance assessment are also valuable because they can drive the development and expansion of health information technology (HIT). Although the Work Group was not tasked with developing specific recommendations on HIT and data sharing, it believes that providers should invest in interoperable systems; that administrative reporting requirements should be minimized as much as possible; that patients and caregivers should have free and ready access to patient records; and that HIT should be used to maintain patient registries and contribute to the development of clinical measures and guidelines.
Payments that fall under Category 2 are distinguished from those that fall under Category 3 in two respects. First, Category 2 payments do not involve arrangements in which providers assume either shared savings or shared losses based on established cost targets. Second, FFS based payments in Category 3 reflect, to a greater degree, care that is provided longitudinally, such that multiple providers are responsible for the cost and quality associated with a particular set of procedures or services. By contrast, Category 2 payments are limited to specific providers.
3 APMs Built on Fee for Service Architecture (Category 3):
Payment models classified in Category 3 are based on an FFS architecture, while providing mechanisms for the effective management of a set of procedures, an episode of care, or all health services provided for individuals. In addition to taking quality considerations into account (as in Category 2), Category 3 payments are based on cost performance against a target, irrespective of how the financial benchmark is established, updated, or adjusted. For APMs in Category 3, providers that meet their cost and quality targets are eligible for shared savings, and those that do not may be held financially accountable.
Additionally, payments in Category 3 are structured to encourage providers to deliver effective and efficient care. Episode based and other types of bundled payments encourage care coordination because they cover a complete set of related services for a procedure that may be delivered by multiple providers. Clinical episode payments fall into Category 3 if they are tied to specific procedures, such as hip replacement or back surgery.
The Work Group has split Category 3 into subcategories A and B as outlined below:
• Category 3A gives providers an opportunity to share in the savings they generate. If a provider participating in a Category 3A APM meets quality targets but does not meet cost targets, then the provider is not held financially responsible for excess spending.
• Payments in Category 3B involve both upside gainsharing (i.e., positive payment adjustments) and downside risk (i.e., negative payment adjustments) based on performance on cost measures.
The Work Group believes payments in Category 3 will advance clinical integration and affordability to a greater extent than payments in Category 2 because risk sharing arrangements provide stronger incentives to manage health care costs and reward care coordination across the span of care.
The most important distinction between Category 3 and Category 4 payments is that the latter (category 4) involve a single payment that encompasses a broad array of services, whereas providers participating in Category 3 models are eligible for only a portion of the losses and/or savings they generate. Additional conditions must be met before a payment model can be placed into Category 4. Specifically, Category 4 payments reflect the total cost of care for treating a primary (typically chronic) condition, or for maintaining the health and managing the illness of an entire population. By contrast, even if they are fully capitated, payments that cover a more limited set of specialty services (including primary care) would be classified in Category 3. For example, a Category 4 model for pediatric care would have to cover a wide range of medical, preventive, and developmental services, whereas a population based payment model for primary care would fall under Category 3 if it did not hold primary care providers accountable for care coordination and the appropriate utilization of specialty services. Similarly, clinical episode payments tied to conditions (e.g., diabetes or cancer) fall under Category 4, whereas clinical episode payments tied to procedures (e.g., hip replacement or back surgery) fall under Category 3, even if they are made on a per member per month basis. As such, Category 4 payments are more person focused, insofar as they include stronger incentives to promote health and wellness throughout the care continuum.
4. Population Based Payment (Category 4):
Payment models classified as Category 4 involve population based payments, structured in a manner that encourages providers to deliver well-coordinated, high quality person level care within a defined (4A) or overall (4B) budget. This holds providers accountable for meeting quality and, increasingly, person centered care goals for a population of patients or members. Payments within Category 4 are intended to cover a wide range of preventive health, health maintenance, and health improvement services, and these payments will likely require care delivery systems to establish teams of health professionals to provide enhanced access and coordinated care. Additionally, and in contrast to capitated arrangements in Category 4N, providers participating in Category 4A and 4B APMs are held accountable for delivering high quality, clinically necessary, and appropriate care.
The Work Group has split Category 4 into subcategories A and B as outlined below:
• Category 4A payments are limited to certain sets of condition specific services (e.g., asthma, diabetes, or cancer), but they remain person focused in the sense that they hold providers accountable for the total cost and quality of care related to that condition. For example, bundled payments for cancer care fall under Category 4A if providers are responsible for the total cost and quality of care for a patient, rather than covering only chemotherapy payments. The Work Group recognizes that in certain instances patient care will predominantly revolve around the management of particular types of conditions, such as cancer or heart disease. In such cases, we recognize that Category 4A may become a suitable and justifiable endpoint, especially for smaller provider organizations which may never be able to deliver certain types of care (such as transplants). Nevertheless, the Work Group maintains that providers should ideally be paid to maintain health and manage illness for an entire population, rather than compartmentalizing payments according to particular conditions. We also believe that condition specific payments should, in time, become part of a comprehensive approach to improving health and reducing costs for an entire population. For highly integrated delivery systems, the Work Group envisions that Category 4A payments will evolve into Category 4B.
• Payments in Category 4B are capitated or population based for all of the individual’s health care needs. Category 4B encompasses a broad range of financing and delivery system arrangements with varying degrees of integration between plans and provider groups. On one end of the spectrum, plans and providers in Category 4B models may be virtually integrated. On the other end of the spectrum are highly integrated arrangements that are characterized by vertical integration of financing and care delivery, common ownership, and strong linkage across strategy, clinical performance, quality, and resource use. These groups may also have a higher percentage of salaried physicians. After reviewing the literature and discussing these highly integrated arrangements with people who operate within them, the Work Group has reached the conclusion that they can be ideally suited for delivering person centered care because they:
1) force transformational thinking about delivery system reform;
2) optimize coordination of infrastructure investments;
3) most fully remove financial incentives for volume; and
4) expedite community investment and engagement.
Although the underlying payment approaches were not sufficiently distinct to warrant the creation of a separate subcategory for highly integrated payment and delivery systems, the Work Group believes that these arrangements yield key benefits and efficiencies, because they have a greater impact on organizational responses to quality and value incentives.
Key Principles for the APM Framework
The Work Group’s Framework is predicated on several key principles. To provide context for understanding the APM Framework and the Work Group’s recommendations, these principles are delineated and explained below.
Principle 1: Changing the financial reward to providers is only one way to stimulate and sustain innovative approaches to the delivery of person centered care. In the future, it will be important to monitor progress in initiatives that empower patients to have a voice in model design, to seek care from high value providers (via performance metrics, financial incentives, and other means), and to become active participants in shared decision making.
Principle 2: As delivery systems evolve, the goal is to drive a shift towards shared risk and population based payment models that incentivize improvements in the quality and efficiency of person centered care.
Principle 3: To the greatest extent possible, value based incentives should reach providers across the care team that directly delivers care.
Principle 4: Payment models that do not take quality and value into account will be classified within the appropriate category with a designation that distinguishes them as a payment model that is not value based. They will not be considered APMs for the purposes of tracking progress towards payment reform.
Principle 5: In order to reach the LAN’s goals for health care reform, value based incentives should be intense enough for providers to invest in and implement delivery reforms, and they should increase over time. However, the strength of incentives does not affect the classification of APMs in the APM Framework.
Principle 6: For tracking purposes, when health plans adopt hybrid payment models that incorporate multiple APMs, the payment dollars will count towards the category of the most dominant APM. This will avoid double counting payments through APMs.
Principle 7: Centers of excellence, patient centered medical homes, and accountable care organizations are delivery models, not payment models. In many instances, these delivery models have an infrastructure to support care coordination and have succeeded in advancing quality. They enable APMs and need the support of APMs, but none of them are synonymous with a specific APM. Accordingly, they appear in multiple categories of the APM Framework, depending on the underlying payment model that supports them.
Conclusion
As set forth in this document, the Work Group is committed to the concept that transitioning from FFS to population based payments is critical for health care transformation. Keeping in mind the underlying principles, the APM Framework provides a high level mapping of payment approaches, as well as a pathway for payment reform and a foundation for measuring progress. The Work Group envisions that these mappings will be useful for all stakeholders and prove enduring as they navigate the health care ecosystem. While the Work Group believes that this Framework identifies and encompasses all models of payment reform and will be enduring, Work Group members hope to return to the White Paper at a later date to take into account new developments in the health care sector. Nevertheless, the Work Group intends the APM Framework to be robust enough to accommodate foreseeable changes, and it strongly believes that this should become the overarching framework for discussing and evaluating payments in the U.S. health care system. The LAN intends to continue compiling and periodically releasing case studies of payment models. (See APM Framework White Paper Addendum.) The Work Group believes this is important because it will disseminate lessons learned and provide the nation with models to consider as public and private plans align around common payment approaches.
The Work Group’s Framework is predicated on several key principles. To provide context for understanding the APM Framework and the Work Group’s recommendations, these principles are delineated and explained below.
Principle 1: Changing the financial reward to providers is only one way to stimulate and sustain innovative approaches to the delivery of person centered care. In the future, it will be important to monitor progress in initiatives that empower patients to have a voice in model design, to seek care from high value providers (via performance metrics, financial incentives, and other means), and to become active participants in shared decision making.
Principle 2: As delivery systems evolve, the goal is to drive a shift towards shared risk and population based payment models that incentivize improvements in the quality and efficiency of person centered care.
Principle 3: To the greatest extent possible, value based incentives should reach providers across the care team that directly delivers care.
Principle 4: Payment models that do not take quality and value into account will be classified within the appropriate category with a designation that distinguishes them as a payment model that is not value based. They will not be considered APMs for the purposes of tracking progress towards payment reform.
Principle 5: In order to reach the LAN’s goals for health care reform, value based incentives should be intense enough for providers to invest in and implement delivery reforms, and they should increase over time. However, the strength of incentives does not affect the classification of APMs in the APM Framework.
Principle 6: For tracking purposes, when health plans adopt hybrid payment models that incorporate multiple APMs, the payment dollars will count towards the category of the most dominant APM. This will avoid double counting payments through APMs.
Principle 7: Centers of excellence, patient centered medical homes, and accountable care organizations are delivery models, not payment models. In many instances, these delivery models have an infrastructure to support care coordination and have succeeded in advancing quality. They enable APMs and need the support of APMs, but none of them are synonymous with a specific APM. Accordingly, they appear in multiple categories of the APM Framework, depending on the underlying payment model that supports them.
Conclusion
As set forth in this document, the Work Group is committed to the concept that transitioning from FFS to population based payments is critical for health care transformation. Keeping in mind the underlying principles, the APM Framework provides a high level mapping of payment approaches, as well as a pathway for payment reform and a foundation for measuring progress. The Work Group envisions that these mappings will be useful for all stakeholders and prove enduring as they navigate the health care ecosystem. While the Work Group believes that this Framework identifies and encompasses all models of payment reform and will be enduring, Work Group members hope to return to the White Paper at a later date to take into account new developments in the health care sector. Nevertheless, the Work Group intends the APM Framework to be robust enough to accommodate foreseeable changes, and it strongly believes that this should become the overarching framework for discussing and evaluating payments in the U.S. health care system. The LAN intends to continue compiling and periodically releasing case studies of payment models. (See APM Framework White Paper Addendum.) The Work Group believes this is important because it will disseminate lessons learned and provide the nation with models to consider as public and private plans align around common payment approaches.
MIPS for psychologists
Psychologists who serve Medicare beneficiaries are eligible (and sometimes required) to participate in the Merit-based Incentive Payment System (MIPS), one of two payment models within Medicare’s Quality Payment Program established to reward health care practitioners for the value and quality of services provided instead of the volume of patients seen.
For more information on psychologists’ participation in the program for 2022, please explore the following resources:
Psychologists who serve Medicare beneficiaries are eligible (and sometimes required) to participate in the Merit-based Incentive Payment System (MIPS), one of two payment models within Medicare’s Quality Payment Program established to reward health care practitioners for the value and quality of services provided instead of the volume of patients seen.
For more information on psychologists’ participation in the program for 2022, please explore the following resources:
Position Statement on Core Principles for Alternative Payment Models for Behavioral Health
Approved by the Assembly, November 2021
Approved by the Assembly, November 2018
American Psychiatric Association (APA) position:
Future alternative payment models (APMs) for mental health care should follow a core set of general principles to avoid unintended consequences that could harm patients, psychiatrists, and other mental health professionals and clinicians, including:
• Setting predominant goals as increasing access, improving health equity, and improving quality of care for individuals with mental health and substance use disorders (MH/SUDs), in order to improve outcomes;
• Covering the cost of providing services based on the true costs of care;
• Incentivizing the care of underserved populations through the use of evidence-based treatments, efficient use of resources, and tracking of outcomes using validated measures;
• Flexible and inclusive design specifically tailored to the care of individuals with MH/SUDs to support individual treatment options and to meet the diverse needs of this heterogeneous patient population;
• Development with substantive input from a racially diverse representation of practicing psychiatrists and other mental health clinicians;
• Voluntary, not mandatory participation in Behavioral Health APMs;
• Improved reimbursement to psychiatrists, other mental health professionals, and systems of care, utilizing value-based payment;
• Addressing many psychiatrists’ lack of access to certified electronic health record technology (CEHRT), the expense and administrative burden of data reporting, and the limited availability of well-validated behavioral mental health quality measures;
• Service delivery using telepsychiatry; and
• including evidence-based programs, outcomes, and incentives to achieve healthy equity and eliminate health disparities.
Approved by the Assembly, November 2021
Approved by the Assembly, November 2018
American Psychiatric Association (APA) position:
Future alternative payment models (APMs) for mental health care should follow a core set of general principles to avoid unintended consequences that could harm patients, psychiatrists, and other mental health professionals and clinicians, including:
• Setting predominant goals as increasing access, improving health equity, and improving quality of care for individuals with mental health and substance use disorders (MH/SUDs), in order to improve outcomes;
• Covering the cost of providing services based on the true costs of care;
• Incentivizing the care of underserved populations through the use of evidence-based treatments, efficient use of resources, and tracking of outcomes using validated measures;
• Flexible and inclusive design specifically tailored to the care of individuals with MH/SUDs to support individual treatment options and to meet the diverse needs of this heterogeneous patient population;
• Development with substantive input from a racially diverse representation of practicing psychiatrists and other mental health clinicians;
• Voluntary, not mandatory participation in Behavioral Health APMs;
• Improved reimbursement to psychiatrists, other mental health professionals, and systems of care, utilizing value-based payment;
• Addressing many psychiatrists’ lack of access to certified electronic health record technology (CEHRT), the expense and administrative burden of data reporting, and the limited availability of well-validated behavioral mental health quality measures;
• Service delivery using telepsychiatry; and
• including evidence-based programs, outcomes, and incentives to achieve healthy equity and eliminate health disparities.
Recognizing and Seizing the Opportunities That Value Based Payment Models Offer Behavioral Health Care
Psychiatric Services 2021; 72:732
https://ps.psychiatryonline.org/doi/10.1176/appi.ps.202000044
Since the passage of the Affordable Care Act, investments in accountable care organizations (ACOs) and other value based payment (VBP) models have accelerated markedly, seeking to address all three aspects of the “triple aim” for the U.S. health care system:
Many early ACOs did not adequately prioritize behavioral health, and those that did often replicated the existing fragmentation between general medical and behavioral health (1).
ACOs that have prioritized behavioral health have identified several financial and logistical barriers, including difficulties sustaining funding for innovative models of care as well as challenges coordinating care because of behavioral health carveouts in ACO contracts(2). (stanowi wyzwanie dla koordynowania opieki ze względu na odstępstwa w zakresie zdrowia behawioralnego w umowach ACO)
Although some health systems have shown promising cost and quality improvements within an ACO model, largely through the expansion of integrated care and other innovative models of care delivery (3),
the overall effect of early ACO programs on behavioral health costs and outcomes has been limited (4).
Finally, whereas patients with mental health and substance use disorders are disproportionately disadvantaged in society, it has been noted that existing VBP or pay-for-performance programs disproportionately penalize health systems serving populations of low socioeconomic status,potentially worsening preexisting health disparities caused by unmet social needs (5, 6).
Despite these challenges, a shift from fee-for-service to a VBP model has potential to improve outcomes for those with behavioral health conditions. With greater use of VBP nationally, it is imperative that health systems find economically sustainable ways to operate in these models.
Characteristics of an Early Adopter Health System and Medicaid ACO Contract
Our organization is an integrated public safety-net community health system with a historic focus on primary care and
behavioral health.
Our system was one of the first health systems in the state to adopt an accountable care model under Massachusetts’s 1115 Medicaid waiver and has adapted in a number of ways. After reviewing the options for VBP contracts under state regulations, our health system chose to partner with a local Medicaid managed care plan to carry out the contract and share governance of the ACO with the health plan. Financially, the ACO receives a risk-adjusted capitated payment
from the state Medicaid program for all its members for the given year and shares risk with the health plan. The health system and health plan share savings and losses equally, and if gains or losses exceed a preset percentage of the global budget, the state Medicaid program will also share in them.
Contractually, our ACO bears full risk of health care costs and does not carve out management of behavioral health to another entity, which makes it unique among area ACOs.
This decision was made because of both the known disadvantages of carve-outs (wyłączenia, odstępstwa), including care fragmentation, conflicting goals, and increased administrative costs, and the health system’s strong commitment to behavioral health services.
An integral part of VBP models is quality measurement. Previous behavioral health quality metrics were extremely limited (early Medicare ACOs measured only “screening for depression”) and were therefore unlikely to produce meaningful changes in care (4). The system’s ACO contract includes a more robust set of quality metrics aimed at measurably improving behavioral health care. Some of these, such as follow-up plans after depression screening and depression remission or response, expand on earlier metrics by using a validated measurement instrument. Others, including hospital readmissions, follow-up within 7 days of discharge from a behavioral health hospitalization, and rates of emergency department (ED) visits for patients with behavioral health conditions, focus on utilization. The contract also includes process and health screening metrics, such as metabolic monitoring for patients on antipsychotics, initiation and engagement of substance use disorder treatment, and engagement with community partners who provide care management and coordination designed to promotecommunitybased stabilization. Finally, the amount of funding tied to quality metrics will increase from 5% to 20% of total reimbursement over the life of the contract, thus increasing incentives for the system to meet quality benchmarks.
More recently, the state has increased capitated payments for individuals with substance use disorder or severe mental illness, for unstably housed individuals with behavioral health conditions, and for youths with severe medical or behavioral health conditions. The effects of these changes are not yet known but are welcome because of the high cost of providing high-quality care for individuals with significant social needs and severe behavioral health conditions.
Initial Approach to Value-Based Care
The system is investing in services for populations with three high-risk, high-cost conditions: serious mental illness, substance use disorders, and severe emotional disturbances of children and adolescents. To address the needs of these populations, the ACO has supported services not traditionally reimbursable by insurance, including intensive case management for those who use the ED frequently, peer recovery coaches for individuals with substance use disorders,
and a “reverse integration” behavioral health home for those with psychosis. Rather than restricting access to inpatient
care, the ACO works to coordinate care transitions and engage with individuals with a history of repeated readmissions in order to achieve longer periods of stability in the community. A small team of seasoned clinicians consults with treatment teams and facilitates access to a range of state-funded and community-based services. Preliminary internal analyses suggest that these interventions have reduced inpatient psychiatry readmissions and ED (emergency department) visits for high-risk patients with behavioral health conditions.
To improve the care of patients who have common conditions, the system introduced collaborative care and office-based substance use disorder treatment across its primary care clinics. Risk scores, based on past utilization and built into electronic health records (EHRs), inform determinations about level of care. Individuals deemed to be at lower risk are initially managed using less resource-intensive methods, such as group visits, indirect consultation in primary care, telepsychiatry, or brief time-limited interventions with integrated behavioral health staff. Individuals requiring more intensive levels of care are referred to specialty psychiatry outpatient treatment or community-based care, depending on the clinical assessment and the patient’s historical treatment use patterns. Shared care plans in the EHR serve to integrate treatment decisions across the continuum of care. Preferred provider agreements define how community-based providers will communicate with primary care teams and encourage the use of electronic communication where possible. In addition, claims data and new population-focused utilization tools enable us to track trends in cost and utilization and to provide timely feedback to providers.
Challenges to Implementation and Future Directions
Our health system faced several initial challenges to implementation.
First, although our system has a large outpatient psychiatry department, it does not provide the full continuum of services necessary to manage the population at the appropriate level of care, to provide hospital diversion, or to offer timely access to less intensive care to step patients down from inpatient treatment. This gap has been especially evident in acute substance use treatment services (detoxification, step-down care) as well as in intermediate levels of care and has contributed to readmissions to acute care. This limitation also has created difficulty for patients to access care and follow up on referrals and has made it difficult for providers to communicate efficiently with external providers in the absence of a shared EHR. Additionally, although our ACO could offer a limited supply of inpatient psychiatric beds, demand has continued to exceed supply.
Second, our system has continued to struggle with existing fragmentation among the broader health care delivery system, community-based services, and government agencies, creating challenges in coordinating care and containing costs.
Third, as in many community mental health settings, workforce recruitment and retention has continued to be a challenge because of the high acuity and social needs of the patient population and the attendant stress on clinicians. (podobnie jak w wielu lokalnych placówkach zdrowia psychicznego, rekrutacja i utrzymanie personelu nadal stanowi wyzwanie ze względu na dużą dotkliwość i potrzeby społeczne populacji pacjentów oraz związany z tym stres, jaki odczuwają lekarze)
Finally, the high degree of poverty, societal marginalization, linguistic diversity, and both acute and chronic trauma faced by the population we serve at times has made the effective engagement in and provision of behavioral health care challenging.
Other health systems may also experience the challenge of controlling costs for substance use disorders relative to other mental health conditions. Our health system placed significant initial emphasis on managing care of individuals with mental health conditions who did not have a primary substance abuse diagnosis and has had relative success in lowering costs and shifting avoidable care from inpatient to diversionary and step-down programs for this population.
However, utilization management has proved more challenging for those with primary substance use disorders, for whom acute service utilization and costs have remained stubbornly high, particularly among homeless individuals.
Additionally, although the opioid overdose crisis has received significant nationwide attention, acute service utilization in our system has been largely driven by those with alcohol use disorders. Whereas funding and treatment for opioid use disorders remains critical, there has been comparatively less attention to and investment in prevention and treatment of alcohol use disorders, which has made linkage to community supports more challenging.
Health plan benefits have been expanded to include residential treatment and recovery coaching, but continued creative collaboration with local public and nonprofit agencies will be crucial, as will policy changes to better treat and ultimately prevent substance use disorders.
In response to these initial challenges, the health system is investing in new services, lowering thresholds to access existing services, and attempting to bridge links with community providers. For instance, the system has developed an EHR-based order set for substance use disorder to improve the consistency of treatment and patient safety. Our system is also developing closer relationships with external, preferred medically monitored detoxification and residential treatment services. Where needed resources do not exist, the system is evaluating business opportunities to create or contract for services to fill gaps. Finally, given the high degree of poverty and deprivation in our population and the key role these social determinants of health play in determining health outcomes, all patients are screened for social determinants of health, and patients are referred for case management support to address identified needs.
Conclusions
Implementation of VBP models will be tested by preexisting shortcomings of the behavioral health system and the impact of social determinants of health on our populations. Fragmentation in the behavioral health delivery system and the limited electronic capabilities of community-based providers remain challenges to better integration of care, and broader social pressures historically outside the health system’s control place financial strain on ACO models. Nonetheless, significant opportunities remain for capitalizing on the opportunities of VBP models, given the pivotal role that behavioral health plays in overall health outcomes. These experiments could be viable even in historically underfunded public and safety-net hospitals. Further progress will depend on collaboration between health systems, policy makers, community-based providers, and service users, both on issues directly relevant to health care payment and to the social support and policy changes that will affect the longterm viability of VBP models.
Psychiatric Services 2021; 72:732
https://ps.psychiatryonline.org/doi/10.1176/appi.ps.202000044
Since the passage of the Affordable Care Act, investments in accountable care organizations (ACOs) and other value based payment (VBP) models have accelerated markedly, seeking to address all three aspects of the “triple aim” for the U.S. health care system:
- bending the cost curve,
- improving health outcomes, and
- improving patient experience of care.
Many early ACOs did not adequately prioritize behavioral health, and those that did often replicated the existing fragmentation between general medical and behavioral health (1).
ACOs that have prioritized behavioral health have identified several financial and logistical barriers, including difficulties sustaining funding for innovative models of care as well as challenges coordinating care because of behavioral health carveouts in ACO contracts(2). (stanowi wyzwanie dla koordynowania opieki ze względu na odstępstwa w zakresie zdrowia behawioralnego w umowach ACO)
Although some health systems have shown promising cost and quality improvements within an ACO model, largely through the expansion of integrated care and other innovative models of care delivery (3),
the overall effect of early ACO programs on behavioral health costs and outcomes has been limited (4).
Finally, whereas patients with mental health and substance use disorders are disproportionately disadvantaged in society, it has been noted that existing VBP or pay-for-performance programs disproportionately penalize health systems serving populations of low socioeconomic status,potentially worsening preexisting health disparities caused by unmet social needs (5, 6).
Despite these challenges, a shift from fee-for-service to a VBP model has potential to improve outcomes for those with behavioral health conditions. With greater use of VBP nationally, it is imperative that health systems find economically sustainable ways to operate in these models.
Characteristics of an Early Adopter Health System and Medicaid ACO Contract
Our organization is an integrated public safety-net community health system with a historic focus on primary care and
behavioral health.
Our system was one of the first health systems in the state to adopt an accountable care model under Massachusetts’s 1115 Medicaid waiver and has adapted in a number of ways. After reviewing the options for VBP contracts under state regulations, our health system chose to partner with a local Medicaid managed care plan to carry out the contract and share governance of the ACO with the health plan. Financially, the ACO receives a risk-adjusted capitated payment
from the state Medicaid program for all its members for the given year and shares risk with the health plan. The health system and health plan share savings and losses equally, and if gains or losses exceed a preset percentage of the global budget, the state Medicaid program will also share in them.
Contractually, our ACO bears full risk of health care costs and does not carve out management of behavioral health to another entity, which makes it unique among area ACOs.
This decision was made because of both the known disadvantages of carve-outs (wyłączenia, odstępstwa), including care fragmentation, conflicting goals, and increased administrative costs, and the health system’s strong commitment to behavioral health services.
An integral part of VBP models is quality measurement. Previous behavioral health quality metrics were extremely limited (early Medicare ACOs measured only “screening for depression”) and were therefore unlikely to produce meaningful changes in care (4). The system’s ACO contract includes a more robust set of quality metrics aimed at measurably improving behavioral health care. Some of these, such as follow-up plans after depression screening and depression remission or response, expand on earlier metrics by using a validated measurement instrument. Others, including hospital readmissions, follow-up within 7 days of discharge from a behavioral health hospitalization, and rates of emergency department (ED) visits for patients with behavioral health conditions, focus on utilization. The contract also includes process and health screening metrics, such as metabolic monitoring for patients on antipsychotics, initiation and engagement of substance use disorder treatment, and engagement with community partners who provide care management and coordination designed to promotecommunitybased stabilization. Finally, the amount of funding tied to quality metrics will increase from 5% to 20% of total reimbursement over the life of the contract, thus increasing incentives for the system to meet quality benchmarks.
More recently, the state has increased capitated payments for individuals with substance use disorder or severe mental illness, for unstably housed individuals with behavioral health conditions, and for youths with severe medical or behavioral health conditions. The effects of these changes are not yet known but are welcome because of the high cost of providing high-quality care for individuals with significant social needs and severe behavioral health conditions.
Initial Approach to Value-Based Care
The system is investing in services for populations with three high-risk, high-cost conditions: serious mental illness, substance use disorders, and severe emotional disturbances of children and adolescents. To address the needs of these populations, the ACO has supported services not traditionally reimbursable by insurance, including intensive case management for those who use the ED frequently, peer recovery coaches for individuals with substance use disorders,
and a “reverse integration” behavioral health home for those with psychosis. Rather than restricting access to inpatient
care, the ACO works to coordinate care transitions and engage with individuals with a history of repeated readmissions in order to achieve longer periods of stability in the community. A small team of seasoned clinicians consults with treatment teams and facilitates access to a range of state-funded and community-based services. Preliminary internal analyses suggest that these interventions have reduced inpatient psychiatry readmissions and ED (emergency department) visits for high-risk patients with behavioral health conditions.
To improve the care of patients who have common conditions, the system introduced collaborative care and office-based substance use disorder treatment across its primary care clinics. Risk scores, based on past utilization and built into electronic health records (EHRs), inform determinations about level of care. Individuals deemed to be at lower risk are initially managed using less resource-intensive methods, such as group visits, indirect consultation in primary care, telepsychiatry, or brief time-limited interventions with integrated behavioral health staff. Individuals requiring more intensive levels of care are referred to specialty psychiatry outpatient treatment or community-based care, depending on the clinical assessment and the patient’s historical treatment use patterns. Shared care plans in the EHR serve to integrate treatment decisions across the continuum of care. Preferred provider agreements define how community-based providers will communicate with primary care teams and encourage the use of electronic communication where possible. In addition, claims data and new population-focused utilization tools enable us to track trends in cost and utilization and to provide timely feedback to providers.
Challenges to Implementation and Future Directions
Our health system faced several initial challenges to implementation.
First, although our system has a large outpatient psychiatry department, it does not provide the full continuum of services necessary to manage the population at the appropriate level of care, to provide hospital diversion, or to offer timely access to less intensive care to step patients down from inpatient treatment. This gap has been especially evident in acute substance use treatment services (detoxification, step-down care) as well as in intermediate levels of care and has contributed to readmissions to acute care. This limitation also has created difficulty for patients to access care and follow up on referrals and has made it difficult for providers to communicate efficiently with external providers in the absence of a shared EHR. Additionally, although our ACO could offer a limited supply of inpatient psychiatric beds, demand has continued to exceed supply.
Second, our system has continued to struggle with existing fragmentation among the broader health care delivery system, community-based services, and government agencies, creating challenges in coordinating care and containing costs.
Third, as in many community mental health settings, workforce recruitment and retention has continued to be a challenge because of the high acuity and social needs of the patient population and the attendant stress on clinicians. (podobnie jak w wielu lokalnych placówkach zdrowia psychicznego, rekrutacja i utrzymanie personelu nadal stanowi wyzwanie ze względu na dużą dotkliwość i potrzeby społeczne populacji pacjentów oraz związany z tym stres, jaki odczuwają lekarze)
Finally, the high degree of poverty, societal marginalization, linguistic diversity, and both acute and chronic trauma faced by the population we serve at times has made the effective engagement in and provision of behavioral health care challenging.
Other health systems may also experience the challenge of controlling costs for substance use disorders relative to other mental health conditions. Our health system placed significant initial emphasis on managing care of individuals with mental health conditions who did not have a primary substance abuse diagnosis and has had relative success in lowering costs and shifting avoidable care from inpatient to diversionary and step-down programs for this population.
However, utilization management has proved more challenging for those with primary substance use disorders, for whom acute service utilization and costs have remained stubbornly high, particularly among homeless individuals.
Additionally, although the opioid overdose crisis has received significant nationwide attention, acute service utilization in our system has been largely driven by those with alcohol use disorders. Whereas funding and treatment for opioid use disorders remains critical, there has been comparatively less attention to and investment in prevention and treatment of alcohol use disorders, which has made linkage to community supports more challenging.
Health plan benefits have been expanded to include residential treatment and recovery coaching, but continued creative collaboration with local public and nonprofit agencies will be crucial, as will policy changes to better treat and ultimately prevent substance use disorders.
In response to these initial challenges, the health system is investing in new services, lowering thresholds to access existing services, and attempting to bridge links with community providers. For instance, the system has developed an EHR-based order set for substance use disorder to improve the consistency of treatment and patient safety. Our system is also developing closer relationships with external, preferred medically monitored detoxification and residential treatment services. Where needed resources do not exist, the system is evaluating business opportunities to create or contract for services to fill gaps. Finally, given the high degree of poverty and deprivation in our population and the key role these social determinants of health play in determining health outcomes, all patients are screened for social determinants of health, and patients are referred for case management support to address identified needs.
Conclusions
Implementation of VBP models will be tested by preexisting shortcomings of the behavioral health system and the impact of social determinants of health on our populations. Fragmentation in the behavioral health delivery system and the limited electronic capabilities of community-based providers remain challenges to better integration of care, and broader social pressures historically outside the health system’s control place financial strain on ACO models. Nonetheless, significant opportunities remain for capitalizing on the opportunities of VBP models, given the pivotal role that behavioral health plays in overall health outcomes. These experiments could be viable even in historically underfunded public and safety-net hospitals. Further progress will depend on collaboration between health systems, policy makers, community-based providers, and service users, both on issues directly relevant to health care payment and to the social support and policy changes that will affect the longterm viability of VBP models.
Assessing and Improving the Quality in Mental Health Services
Lampros Samartzis and Michael A. Talias
International Journal of Environmental Research and Public Health 2020, 17, 249
1. Introduction
Evaluation/measurement of existing quality is a prerequisite for its improvement: What cannot be evaluated and measured cannot be improved. The evaluation of the quality of mental health services at the national and international levels is qualitative and quantitative. However, this is a complicated process as there are no common scientific language, objectives, and priorities and there are no common examples in this area, and for most countries—even for those that are developed—there are clearly unmet needs in this area. There are significant differences in the quality of mental health services both between and within countries, which clinically take the form of different distances, within each health system, between the clinical guidelines of international scientific societies and daily clinical practice. Clinical decisions about the same symptom and illness differ from country to country because the systems in place for psychiatry are different, and therefore the resources and opportunities for quality mental health care are different.
In this study, we propose and describe the methodology and procedure for a thorough evaluation of the quality of mental health services at the health system level. Evaluation is based on evaluation criteria, and each criterion has its own specific evaluation indicators. Different criteria mean different problems. The indicators do not suggest a solution to the problem under consideration. Indicators collectively can help to clarify and quantify policy objectives and strategies for an optimized Mental Health System. The purpose of the project is twofold: first, to propose an integrated model of mental health services evaluation, and second to target specific interventions to improve the quality of mental health services at the level of the health system.
2. Materials and Methods
In order to search for criteria, indicators and methodology for evaluating and improving the quality of mental health services and related qualitative and quantitative indicators, a bibliography was searched in large databases PubMed, Google Scholar, CINAHL, using the keywords “mental”, “health”, “quality”, “indicators”, alone or in combinations thereof. Peer review journals were searched with English keywords for articles published in peer-reviewed journals possessing an English abstract without setting restrictions for the languages of the main text. Mental health databases maintained by Eurostat, WHO, and OECD were also searched.
To evaluate and measure the quality of mental health services, we propose and describe an eight-dimensional model in this study. Each dimension is an independent, quality assessment criterion. The model comes from the Canadian Health System General Rating System but is modified and enriched by the author specifically for mental health services and includes only mental health-related indicators...
The eight dimensions (criteria) in which mental health services are evaluated are as follows:
(1) appropriateness of services provided,
(2) accessibility of patients to services provided,
(3) acceptability of the services from the patients,
(4) competence of mental health care providers,
(5) effectiveness of mental health professionals
(6) therapeutic continuity in the mental health system,
(7) the efficiency of health professionals,
(8) the safety of patients and health care providers.
Indicators of each dimension can be characterized as indicators of structure, indicators of process, and indicators of the outcome, as suggested by other researchers in the evaluation of the quality of mental health services. Each of the dimensions has aspects called indicators, which are described in detail in the text. Specifically, for each indicator is described:
(a) the background and the general meaning of the index,
(b) the definition that includes how the index is calculated, and
(c) the performance target for mental health services, quantitatively or qualitatively: The performance target is the benchmark.
3. Results
3.1. Appropriateness Criterion, or Appropriateness Dimension. Indicators of Appropriateness of Mental Health Services
S 3.1.1. The Number of Chronic Patients Hospitalized in Psychiatric Hospitals Rather Than Rehabilitation in an Outpatient Setting
S 3.1.2. Number of Cases That Could Avoid Admission to Hospital with Appropriate External Intervention
S 3.1.3. Number of Cases Treated without Indication
3.2. Accessibility Criterion, or Otherwise Accessibility Dimensions. Accessibility and Accessibility Indicators
P 3.2.1. Waiting Time at the Accident and Emergency Department
P 3.2.2. Waiting Days for Evaluation in the Outpatient Clinic
S 3.2.3. Waiting Days for Admission to the Clinic (Waiting Lists)
S 3.2.4. Percentage of the Population Having Access to the Health System
3.3. Acceptability Criterion or Acceptability Dimension. Indicators of Acceptability
O 3.3.1. Average Patient Satisfaction Rating
P+O 3.3.2. Recording Patient Experiences
P 3.3.3. Patients’ Rights to Information and Protection of Their Personal Data
P 3.3.4. Patient Rights to Health Services
P 3.3.5. Number of Patients Leaving the Clinic with a Discharge Note
P 3.3.6. Number of Patients Using the Suggestion/Complaint Box
3.4. Competence Criterion or Competence Dimension. Indicators of Competence
S 3.4.1. Lifelong Learning Program for Mental Health Professionals
P 3.4.2. Lifelong Learning Program with Quantification of Training for Mental Health Professionals
3.5. E ectiveness Criterion or E ectiveness Dimension. Indicators of E ectiveness
O 3.5.1. Percentage of Patients Who Have Improved as a Result of Treatment
O 3.5.2. Extra Mortality in Patients with Schizophrenia Overall and by Sex
O 3.5.3. Extra Mortality in Patients with Bipolar Disorder Overall and by Sex
S 3.5.4. Number of Psychiatric Beds per 100,000 Inhabitants
O 3.5.5. Inpatient Suicides
O 3.5.6. Suicides of Patients Hospitalized in a Psychiatric Facility in the Last Month and Previous Year
O 3.5.7. Suicides in the Country Last Year
P 3.5.8. Percentage of Patients Who Completed the Addiction Treatment Program
O 3.5.9. Percentage of Substance Abusers Who Have Reduced Consumption as a Consequence of Treatment
O 3.5.10. Percentage of Patients Readmitted in One Month
O 3.5.11. Percentage of Patients Who Continued Relapse Prevention Therapy after Detoxification
O 3.5.12. Number of Abstinence Days after Discharge from the Clinic (Days until Relapse)
O 3.5.13. Number of Days with Consumption More Than Two Units of Alcohol (Iu, International Units)
O 3.5.14. The Average Consumption of Alcohol or of Other Recreational Substance of Abuse after Discharge from the Clinic
3.6. The Criterion of Therapeutic Continuity or Therapeutic Continuity Dimension. Therapeutic Continuity Indicators
O 3.6.1. Percentage of Patients Continuing an Outpatient Follow-Up Program after Completion of the Inpatient Treatment Program
O 3.6.2. Percentage of Patients Attending the First Follow-Up Appointment as an Outpatient after Being Discharged from the Psychiatric Clinic
O 3.6.3. Percentage of Patients Attending the First Follow-Up Appointment after Discharge from an Inpatient Clinic for Treatment of Substance Use Disorder
O 3.6.4. Percentage of Patients Who Attended the Next Two Appointments after Being Discharged from Hospital
O 3.6.5. Number of Patients Attending Two Consecutive Appointments
P 3.6.6. Number of Referrals
3.7. Efficiency Criterion or Efficiency Dimension. Efficiency Indicators
S 3.7.1. Number of Mental Health Professionals per 100,000 Population
S 3.7.2. Percentage of the Workforce in the Country That Is Working in the Health System
S 3.7.3. Number of Patients per Physician per Day, in the Outpatient Clinic
O 3.7.4. The Average Length of Hospitalization
O 3.7.5. The Average Cost of Hospitalization per Patient per Doctor, Clinic, Field, Hospital
O 3.7.6. The Average Cost per Day of Hospitalization per Clinic, Sector, and Hospital
O 3.7.7. The Average Cost of Medication Consumption per Patient and per Day of Hospitalization, per Physician, Clinic, Field, Hospital
P 3.7.8. The Average Cost of Diagnostic Examinations per Physician, Clinic, Field, Hospital
P 3.7.9. Cost per Diagnosis Related Group (DRG)
P 3.7.10. Cost per Current Procedural Terminology
S 3.7.11. Doctors to Nurses Ratio
S 3.7.12. Doctors per Nurse per Bed in the Hospital
S 3.7.13. Economic Sustainability and Sustainable Development
P 3.7.14. Average Beds Occupancy
O 3.7.15. Average Inflow Rate (Average Number of Patients per Bed per Year)
P 3.7.16. Average Bed Rotation Interva
3.7.17. Cost of Mental Health Services Compared to Health System Costs
P 3.7.18. Existence of Strategic Plan and Action Plan
O 3.7.19. Mental Health Research Index
3.8. Safety Criterion or Safety Dimension. Indicators of Safety
O 3.8.1. Number of Incidents of Verbal Violence
O 3.8.2. Number of Incidents of Physical Violence
O 3.8.3. Number of Cases of Illegal Drug Use in the Clinic
O 3.8.4. Number of Cases of Alcohol Use in the Clinic
P 3.8.5. Personal Data Security
P 3.8.6. Existence of Institutionalized Internal and External Evaluation of Patients’ Human Rights
4. Discussion
Quality assessment in the provision of mental health services is a multidimensional process and di cult to implement. The di culty is compounded by the lack of reliable biological markers in psychiatric evaluation, which makes it di cult to quantify any improvement after hospitalization, or in general after hospital or out-of-hospital pharmacotherapy and psychotherapy interventions. The availability of biomarkers is going to increase in the near future as a great amount of research is already oriented in this direction.
The appropriateness of clinical structure and treatment is an important dimension of quality. Despite the progress in de-institutionalization in the mental health systems of most EU Member States, however, avoiding unnecessary admissions in the psychiatric clinic sometimes still remains a challenge. Additionally, a challenge is the continuity of rehabilitation in the community immediately after discharge from the hospital. For this to happen, appropriate outpatient structures are needed, which is not always possible, as many countries have been in a hurry to over-de-institutionalize, which has led to a deterioration in the prognosis and quality of life for a subgroup of chronic patients whose quality of life have decreased whilst morbidity has increased due to lack of appropriate community mental health services. In this case, there is an unmet need for coordination and close co-operation between the general practitioners and community mental health services in order to improve appropriateness of referals. The three indicators for qualitative assessment of appropriateness included in the review adequately quantify this dimension of services.
Accessibility to services is crucial for early treatment, and therefore for prognosis. Accessibility in mental health services is a core issue that a ects all underprivileged people with mental health issues and is more evident in vulnerable subpopulations as the immigrants and refugees...
In assessing the quality of mental health services, the degree of acceptability and overall opinion of service users is valuable and should be taken in to account...
The competence of mental health professionals is included in the evaluation and evaluated through the development of lifelong learning programs....
The efficacy of therapeutic interventions is an important element of the quality of mental health services and is evaluated through indicators assessing the outcome of therapies and, more generally, the prognosis of patients with specific diagnoses and the structural characteristics of services.
Ensuring therapeutic continuity is an important element of quality and is evaluated both by the seamless referral, mobility, and accessibility of patients to the most appropriate health care services as well as by the smooth transition from inpatient care to outpatient services. Despite the debate between continuity of care versus specialization of teams, continuity of care has been related to better social functioning, especially when primary care and mental health care, addiction and social welfare services are oriented towards recovery...
Evaluating the effectiveness of mental health services is a multifaceted quality control process. It includes indicators of mainly economic interests that are important for the sustainability and sustainable development of structures, services, and the mental health system. Recruitment, funding, and resource utilization are important aspects that should be clearly included in the strategic planning and action plan of the organization.
Safety is an important element of quality and includes the safety of patients as well as health professionals. Violence in mainly verbal and rarely physical, and in danger are mainly male nurses who areworkingintheemergencypsychiatryward. Training in communication skills and de-escalating skills are important pillars of violence prevention in mental health services settings...
There view in cludes the author’s most important quality indicators that cover all aspects of mental health service quality assessment. The current trend in measuring the quality of mental health has been taken into account, where research interest has now shifted from measuring structures and services to prognosis, outcome, and outcome measurement...
However,itisalimitationofthestudythatthatwedidnotsearchand,therefore,wedidnotinclude in this study, the body of published literature that did not have an English abstract. We considered only studies with an English abstract and we excluded those not referring to the developed countries, to the extent possible...
Another limitation of the study is the fact that it is not a systematic review but rather a narrative review, with a focus on clinically relevant indicators, that is, those that will ensure clinical quality...
In order to be used in practice, the above quality assessment indicators, for improvement of the quality of mental health services, they must be converted into electronic form, so that they can be automatically and systematically measured by appropriate e-health software. This will enable the indicators to be calculated automatically and their scores made available to the management team at any time. The existence of an integrated IT system for the collection of mental health data and indicators has been considered essential, and the establishment of a specialized independent European Mental Health Observatory within the EU has been proposed as an urgent need...
5. Conclusions
The long-term goal of this study is to provide an opportunity for Mental Health professionals to useresearchevidence, asshouldbeexpected, tounderpinthepublicandmentalhealthpolicy. Alimited number of studies have so far partially tackled the problem of connecting the quality assessment issues with the performance of mental health systems. This study provides a holistic approach to connect the quality aspects of a Mental Health System with its e ciency. Furthermore, the increasing availability of healthcare data will enhance the possibility of driving an important decision on how to build up a complex mental health system efficiently using Big data. It is important to note that a set of indicators can be used simultaneously, and these can be used to frame the issues and to define the problems under consideration. Di erent criteria mean di erent problems. The indicators do not suggest a solution to the problem under consideration. Indicators collectively can help to clarify and quantify policy objectives and strategies for an optimized Mental Healthcare system. Mental health is an important social parameter related to well-being, quality of life, human rights, but also to economics, creativity, productivity, sustainability, and sustainable development. Mental health is, therefore, socially good and the welfare state has a responsibility to maintain and improve it, through a system of mental health services of high quality, but also through interprofessional health education and preventive psychiatry programs. Improving the quality of mental health services requires assessing the existing quality and measuring and quantifying it so that comparisons can be made feasible over time at local, state, and transnational levels. Through the evaluation and measurement of quality with the proposed indicators, the areas of the mental health system that need to be emphasized and improved are revealed. Additionally, the optimization of available human resources and funding is optimized, and the mental health policies and planning of mental health services, based on scientific evidence, are encouraged.
Lampros Samartzis and Michael A. Talias
International Journal of Environmental Research and Public Health 2020, 17, 249
1. Introduction
Evaluation/measurement of existing quality is a prerequisite for its improvement: What cannot be evaluated and measured cannot be improved. The evaluation of the quality of mental health services at the national and international levels is qualitative and quantitative. However, this is a complicated process as there are no common scientific language, objectives, and priorities and there are no common examples in this area, and for most countries—even for those that are developed—there are clearly unmet needs in this area. There are significant differences in the quality of mental health services both between and within countries, which clinically take the form of different distances, within each health system, between the clinical guidelines of international scientific societies and daily clinical practice. Clinical decisions about the same symptom and illness differ from country to country because the systems in place for psychiatry are different, and therefore the resources and opportunities for quality mental health care are different.
In this study, we propose and describe the methodology and procedure for a thorough evaluation of the quality of mental health services at the health system level. Evaluation is based on evaluation criteria, and each criterion has its own specific evaluation indicators. Different criteria mean different problems. The indicators do not suggest a solution to the problem under consideration. Indicators collectively can help to clarify and quantify policy objectives and strategies for an optimized Mental Health System. The purpose of the project is twofold: first, to propose an integrated model of mental health services evaluation, and second to target specific interventions to improve the quality of mental health services at the level of the health system.
2. Materials and Methods
In order to search for criteria, indicators and methodology for evaluating and improving the quality of mental health services and related qualitative and quantitative indicators, a bibliography was searched in large databases PubMed, Google Scholar, CINAHL, using the keywords “mental”, “health”, “quality”, “indicators”, alone or in combinations thereof. Peer review journals were searched with English keywords for articles published in peer-reviewed journals possessing an English abstract without setting restrictions for the languages of the main text. Mental health databases maintained by Eurostat, WHO, and OECD were also searched.
To evaluate and measure the quality of mental health services, we propose and describe an eight-dimensional model in this study. Each dimension is an independent, quality assessment criterion. The model comes from the Canadian Health System General Rating System but is modified and enriched by the author specifically for mental health services and includes only mental health-related indicators...
The eight dimensions (criteria) in which mental health services are evaluated are as follows:
(1) appropriateness of services provided,
(2) accessibility of patients to services provided,
(3) acceptability of the services from the patients,
(4) competence of mental health care providers,
(5) effectiveness of mental health professionals
(6) therapeutic continuity in the mental health system,
(7) the efficiency of health professionals,
(8) the safety of patients and health care providers.
Indicators of each dimension can be characterized as indicators of structure, indicators of process, and indicators of the outcome, as suggested by other researchers in the evaluation of the quality of mental health services. Each of the dimensions has aspects called indicators, which are described in detail in the text. Specifically, for each indicator is described:
(a) the background and the general meaning of the index,
(b) the definition that includes how the index is calculated, and
(c) the performance target for mental health services, quantitatively or qualitatively: The performance target is the benchmark.
3. Results
3.1. Appropriateness Criterion, or Appropriateness Dimension. Indicators of Appropriateness of Mental Health Services
S 3.1.1. The Number of Chronic Patients Hospitalized in Psychiatric Hospitals Rather Than Rehabilitation in an Outpatient Setting
S 3.1.2. Number of Cases That Could Avoid Admission to Hospital with Appropriate External Intervention
S 3.1.3. Number of Cases Treated without Indication
3.2. Accessibility Criterion, or Otherwise Accessibility Dimensions. Accessibility and Accessibility Indicators
P 3.2.1. Waiting Time at the Accident and Emergency Department
P 3.2.2. Waiting Days for Evaluation in the Outpatient Clinic
S 3.2.3. Waiting Days for Admission to the Clinic (Waiting Lists)
S 3.2.4. Percentage of the Population Having Access to the Health System
3.3. Acceptability Criterion or Acceptability Dimension. Indicators of Acceptability
O 3.3.1. Average Patient Satisfaction Rating
P+O 3.3.2. Recording Patient Experiences
P 3.3.3. Patients’ Rights to Information and Protection of Their Personal Data
P 3.3.4. Patient Rights to Health Services
P 3.3.5. Number of Patients Leaving the Clinic with a Discharge Note
P 3.3.6. Number of Patients Using the Suggestion/Complaint Box
3.4. Competence Criterion or Competence Dimension. Indicators of Competence
S 3.4.1. Lifelong Learning Program for Mental Health Professionals
P 3.4.2. Lifelong Learning Program with Quantification of Training for Mental Health Professionals
3.5. E ectiveness Criterion or E ectiveness Dimension. Indicators of E ectiveness
O 3.5.1. Percentage of Patients Who Have Improved as a Result of Treatment
O 3.5.2. Extra Mortality in Patients with Schizophrenia Overall and by Sex
O 3.5.3. Extra Mortality in Patients with Bipolar Disorder Overall and by Sex
S 3.5.4. Number of Psychiatric Beds per 100,000 Inhabitants
O 3.5.5. Inpatient Suicides
O 3.5.6. Suicides of Patients Hospitalized in a Psychiatric Facility in the Last Month and Previous Year
O 3.5.7. Suicides in the Country Last Year
P 3.5.8. Percentage of Patients Who Completed the Addiction Treatment Program
O 3.5.9. Percentage of Substance Abusers Who Have Reduced Consumption as a Consequence of Treatment
O 3.5.10. Percentage of Patients Readmitted in One Month
O 3.5.11. Percentage of Patients Who Continued Relapse Prevention Therapy after Detoxification
O 3.5.12. Number of Abstinence Days after Discharge from the Clinic (Days until Relapse)
O 3.5.13. Number of Days with Consumption More Than Two Units of Alcohol (Iu, International Units)
O 3.5.14. The Average Consumption of Alcohol or of Other Recreational Substance of Abuse after Discharge from the Clinic
3.6. The Criterion of Therapeutic Continuity or Therapeutic Continuity Dimension. Therapeutic Continuity Indicators
O 3.6.1. Percentage of Patients Continuing an Outpatient Follow-Up Program after Completion of the Inpatient Treatment Program
O 3.6.2. Percentage of Patients Attending the First Follow-Up Appointment as an Outpatient after Being Discharged from the Psychiatric Clinic
O 3.6.3. Percentage of Patients Attending the First Follow-Up Appointment after Discharge from an Inpatient Clinic for Treatment of Substance Use Disorder
O 3.6.4. Percentage of Patients Who Attended the Next Two Appointments after Being Discharged from Hospital
O 3.6.5. Number of Patients Attending Two Consecutive Appointments
P 3.6.6. Number of Referrals
3.7. Efficiency Criterion or Efficiency Dimension. Efficiency Indicators
S 3.7.1. Number of Mental Health Professionals per 100,000 Population
S 3.7.2. Percentage of the Workforce in the Country That Is Working in the Health System
S 3.7.3. Number of Patients per Physician per Day, in the Outpatient Clinic
O 3.7.4. The Average Length of Hospitalization
O 3.7.5. The Average Cost of Hospitalization per Patient per Doctor, Clinic, Field, Hospital
O 3.7.6. The Average Cost per Day of Hospitalization per Clinic, Sector, and Hospital
O 3.7.7. The Average Cost of Medication Consumption per Patient and per Day of Hospitalization, per Physician, Clinic, Field, Hospital
P 3.7.8. The Average Cost of Diagnostic Examinations per Physician, Clinic, Field, Hospital
P 3.7.9. Cost per Diagnosis Related Group (DRG)
P 3.7.10. Cost per Current Procedural Terminology
S 3.7.11. Doctors to Nurses Ratio
S 3.7.12. Doctors per Nurse per Bed in the Hospital
S 3.7.13. Economic Sustainability and Sustainable Development
P 3.7.14. Average Beds Occupancy
O 3.7.15. Average Inflow Rate (Average Number of Patients per Bed per Year)
P 3.7.16. Average Bed Rotation Interva
3.7.17. Cost of Mental Health Services Compared to Health System Costs
P 3.7.18. Existence of Strategic Plan and Action Plan
O 3.7.19. Mental Health Research Index
3.8. Safety Criterion or Safety Dimension. Indicators of Safety
O 3.8.1. Number of Incidents of Verbal Violence
O 3.8.2. Number of Incidents of Physical Violence
O 3.8.3. Number of Cases of Illegal Drug Use in the Clinic
O 3.8.4. Number of Cases of Alcohol Use in the Clinic
P 3.8.5. Personal Data Security
P 3.8.6. Existence of Institutionalized Internal and External Evaluation of Patients’ Human Rights
4. Discussion
Quality assessment in the provision of mental health services is a multidimensional process and di cult to implement. The di culty is compounded by the lack of reliable biological markers in psychiatric evaluation, which makes it di cult to quantify any improvement after hospitalization, or in general after hospital or out-of-hospital pharmacotherapy and psychotherapy interventions. The availability of biomarkers is going to increase in the near future as a great amount of research is already oriented in this direction.
The appropriateness of clinical structure and treatment is an important dimension of quality. Despite the progress in de-institutionalization in the mental health systems of most EU Member States, however, avoiding unnecessary admissions in the psychiatric clinic sometimes still remains a challenge. Additionally, a challenge is the continuity of rehabilitation in the community immediately after discharge from the hospital. For this to happen, appropriate outpatient structures are needed, which is not always possible, as many countries have been in a hurry to over-de-institutionalize, which has led to a deterioration in the prognosis and quality of life for a subgroup of chronic patients whose quality of life have decreased whilst morbidity has increased due to lack of appropriate community mental health services. In this case, there is an unmet need for coordination and close co-operation between the general practitioners and community mental health services in order to improve appropriateness of referals. The three indicators for qualitative assessment of appropriateness included in the review adequately quantify this dimension of services.
Accessibility to services is crucial for early treatment, and therefore for prognosis. Accessibility in mental health services is a core issue that a ects all underprivileged people with mental health issues and is more evident in vulnerable subpopulations as the immigrants and refugees...
In assessing the quality of mental health services, the degree of acceptability and overall opinion of service users is valuable and should be taken in to account...
The competence of mental health professionals is included in the evaluation and evaluated through the development of lifelong learning programs....
The efficacy of therapeutic interventions is an important element of the quality of mental health services and is evaluated through indicators assessing the outcome of therapies and, more generally, the prognosis of patients with specific diagnoses and the structural characteristics of services.
Ensuring therapeutic continuity is an important element of quality and is evaluated both by the seamless referral, mobility, and accessibility of patients to the most appropriate health care services as well as by the smooth transition from inpatient care to outpatient services. Despite the debate between continuity of care versus specialization of teams, continuity of care has been related to better social functioning, especially when primary care and mental health care, addiction and social welfare services are oriented towards recovery...
Evaluating the effectiveness of mental health services is a multifaceted quality control process. It includes indicators of mainly economic interests that are important for the sustainability and sustainable development of structures, services, and the mental health system. Recruitment, funding, and resource utilization are important aspects that should be clearly included in the strategic planning and action plan of the organization.
Safety is an important element of quality and includes the safety of patients as well as health professionals. Violence in mainly verbal and rarely physical, and in danger are mainly male nurses who areworkingintheemergencypsychiatryward. Training in communication skills and de-escalating skills are important pillars of violence prevention in mental health services settings...
There view in cludes the author’s most important quality indicators that cover all aspects of mental health service quality assessment. The current trend in measuring the quality of mental health has been taken into account, where research interest has now shifted from measuring structures and services to prognosis, outcome, and outcome measurement...
However,itisalimitationofthestudythatthatwedidnotsearchand,therefore,wedidnotinclude in this study, the body of published literature that did not have an English abstract. We considered only studies with an English abstract and we excluded those not referring to the developed countries, to the extent possible...
Another limitation of the study is the fact that it is not a systematic review but rather a narrative review, with a focus on clinically relevant indicators, that is, those that will ensure clinical quality...
In order to be used in practice, the above quality assessment indicators, for improvement of the quality of mental health services, they must be converted into electronic form, so that they can be automatically and systematically measured by appropriate e-health software. This will enable the indicators to be calculated automatically and their scores made available to the management team at any time. The existence of an integrated IT system for the collection of mental health data and indicators has been considered essential, and the establishment of a specialized independent European Mental Health Observatory within the EU has been proposed as an urgent need...
5. Conclusions
The long-term goal of this study is to provide an opportunity for Mental Health professionals to useresearchevidence, asshouldbeexpected, tounderpinthepublicandmentalhealthpolicy. Alimited number of studies have so far partially tackled the problem of connecting the quality assessment issues with the performance of mental health systems. This study provides a holistic approach to connect the quality aspects of a Mental Health System with its e ciency. Furthermore, the increasing availability of healthcare data will enhance the possibility of driving an important decision on how to build up a complex mental health system efficiently using Big data. It is important to note that a set of indicators can be used simultaneously, and these can be used to frame the issues and to define the problems under consideration. Di erent criteria mean di erent problems. The indicators do not suggest a solution to the problem under consideration. Indicators collectively can help to clarify and quantify policy objectives and strategies for an optimized Mental Healthcare system. Mental health is an important social parameter related to well-being, quality of life, human rights, but also to economics, creativity, productivity, sustainability, and sustainable development. Mental health is, therefore, socially good and the welfare state has a responsibility to maintain and improve it, through a system of mental health services of high quality, but also through interprofessional health education and preventive psychiatry programs. Improving the quality of mental health services requires assessing the existing quality and measuring and quantifying it so that comparisons can be made feasible over time at local, state, and transnational levels. Through the evaluation and measurement of quality with the proposed indicators, the areas of the mental health system that need to be emphasized and improved are revealed. Additionally, the optimization of available human resources and funding is optimized, and the mental health policies and planning of mental health services, based on scientific evidence, are encouraged.
Population-Based Approaches to Mental Health: History, Strategies, and Evidence
Jonathan Purtle, Katherine L. Nelson, Nathaniel Z. Counts, Michael Yudell
Annu Rev Public Health. 2020 April 02; 41: 201–221.
INTRODUCTION
Approaches to addressing mental health issues in society have overwhelmingly focused on the provision of clinical services to individuals, not on fostering conditions that promote positive mental health, mental health promotion, or the primary prevention of mental illness.
Although clinical mental health services dramatically improve the lives of many people and their families, there are several reasons why the provision of clinical services in isolation is a suboptimal approach to maximizing the mental health of a population.
Positive mental health: sense of well-being, capacity to enjoy life, and the ability to deal with challenges—not only the absence of a mental health illness or condition
Mental health promotion: actions to improve quality of life and well-being, as opposed to ameliorating mental illness symptoms and mental health deficits
Primary prevention of mental illness: actions that address factors that might cause mental illnesses to avert their development
Most people who need mental health services do not receive them, in part because of workforce shortages. Estimates indicate that an additional 15,400 psychiatrists and 57,490 psychologists are needed by 2025 to meet the mental health service demand of the US population. Among people who do receive mental health services, there is a moderate likelihood that the services provided will not be evidence-based, implemented with fidelity, or effective. For these reasons, population-level increases in mental health service utilization are not associated with improvements in population mental health status. Finally, evidence suggests that much of the population burden of mental health problems can be prevented by reducing exposure to traumatic and chronic stressors, especially during key periods of child development. Taken together, these facts underscore the importance of complementing clinical approaches to mental health with population-based approaches that simultaneously affect entire groups of people.
The review is also focused on population-based approaches across three broad domains—public policy, public health practice, and health care system design—and does not focus on strategies for specific settings and populations (e.g., children in schools, people in prisons, older adults in elder care facilities).
Behavioral health: an umbrella term that refers to both mental health and substance use issues
Defining Interventions and Activities
Population-based interventions must be nonclinical and thus exclude direct mental health services (e.g., psychotherapies and pharmacological therapies) to individual patients.
Health care system-level interventions that address mental health, however, can be considered population-based because the intervention is at the system, as opposed to the clinical, level. Social, economic, and environmental policies are also considered population based interventions because they affect groups of people simultaneously, and psychiatric epidemiology studies indicate that a wide range of public policies affect mental health (detailed below). The definition includes mention of activities to encompass practices that monitor mental health outcomes and determinants without intervening on them
Psychiatric epidemiology: study of the incidence, prevalence, distribution, causes, and consequences of mental health conditions across people, space, and time
The interventions must also be implemented with the intent of addressing mental health outcomes or their determinants. This requirement stems from dictionary definitions of “approach”—“a way of doing or thinking about something such as a problem or a task”
This review draws from research about population-based interventions that affect mental health outcomes or determinants without the explicit intent of addressing them. These interventions are relevant because they could be implemented with the explicit intent of improving population mental health. The review also draws from research about population-based interventions that negatively affect mental health. Identifying these deleterious interventions is important because reforming them can produce benefits for population mental health.
Defining Outcomes and Determinants
Mental health outcomes can be conceptualized in many different ways—ranging from meeting full diagnostic criteria for a disorder in the DSM, to symptom severity of a disorder regardless of whether full DSM criteria are met, to general emotional distress, and across a continuum spanning from languishing to flourishing.... These include proximal determinants (e.g., poor sleep quality, exposure to traumatic stressors) as well as distal determinants (e.g., built environments with excessive ambient light and noise at night, high rates of community violence), which are the causes of the causes.
Defining Populations
In this review, the focus is on groups that share a geographic region (e.g., state or country), sociodemographic characteristics (e.g., ethnic or sexual minorities), or shared source of clinical service utilization (e.g., hospital, health care system). These types of groups encompass how populations are typically conceptualized in both public health and health care.
POPULATION-BASED APPROACHES TO MENTAL HEALTH AND THEIR EVIDENCE
Table 1 shows three broad domains in which population-based approaches to mental health can be implemented, identifies actors that are key to implementing these approaches, and summarizes core activities to these approaches. The text that follows provides detail about these approaches and evidence of their effectiveness.
Social, Economic, and Environmental Policy Approaches
In general, much more is known about the negative impacts of policies on mental health than about how policy can improve population mental health. This section provides a high-level summary of goals that can be advanced by public policy to improve the determinants of population mental health. The policy areas and approaches discussed in this section are not exhaustive, and each could be the focus of its own review.
Gene × environment interaction: when a person’s genetic predispositions for an outcome (e.g., mental illness) vary according to the environmental conditions to which they are exposed.
Reduce the incidence of traumatic events.
Exposures to traumatic events are well-established risk factors for post-traumatic stress disorder, depression, and a range of other mental health problems. Thus, policies that reduce the incidence of, and exposure to, traumatic events could substantially improve population mental health. Although not adopted with the explicit intent of improving mental health, evidence-based policies that prevent violent crime and accidental injuries—common traumatic events that carry high risk for mental health problems—might have the greatest impacts.
Stress: an individual’s mental, emotional, and physical response to demands or changes that require an adjustment.
Potentially traumatic events: experiencing, witnessing, or hearing about death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence.
Reduce the incidence of adverse childhood experiences.
Cumulative exposure to adverse childhood experiences (ACEs) increases risk for adult mental health problems.
Adverse childhood experiences: direct and indirect exposure to violence, abuse, neglect, and other forms of extreme stress before the age of 18—originally operationalized as ten indicators of “household dysfunction”
Modify the built environment.
Moderate evidence has shown that public policies can be used to improve population mental health by modifying three features of the built environment: green space, ambient light at night, and ambient noise. Exposure to green space, especially in urban areas, is associated with positive mental health, and policies that increase exposure could produce benefits by reducing stress, increasing physical activity, and preventing violent crime exposure.
Reduce financial and housing insecurity.
Associations between socioeconomic position and mental health are extremely complex, but evidence has shown that policies that promote financial and housing security among low-income populations could produce mental health benefits by reducing exposure to chronic stressors.
Public policy can also reduce stress among low-income groups and improve population mental health by reducing housing insecurity, such as through increasing public housing subsidies.
Reduce structural stigma toward people with mental illness and members of other social groups.
Structural stigma, which is often codified in policies, negatively affects population mental health though discrimination that inhibits access to resources and by fostering feelings of social exclusion and stress among socially marginalized groups. Identifying and reforming policies that create structural stigma is a strategy to improve population mental health. In terms of structural stigma toward people with mental illness, examples of policies to reform include those that prohibit people with mental illness from holding public office or practicing medicine.
In terms of other socially marginalized groups, numerous studies have demonstrated associations between policies that affect structural stigma toward sexual minorities and the mental health of these groups.
Structural stigma: societal conditions, cultural norms, and policies that constrain the opportunities, resources, and well-being of socially marginalized groups.
Structural racism: laws and system-level policies that limit racial minorities’ access to social and economic opportunities.
Public Health Practice Approaches
The United States has 59 state and territorial public health departments and more than 2,800 local public health departments (LHDs), all of which have a mandate to protect and promote population health. Although the structure and function of public health departments vary across the United States, most operate separately from their jurisdiction’s mental health agency.
Although mental health agencies in some jurisdictions have embraced a population-based approach—New York City and Philadelphia, for example—mental health agencies are usually narrowly focused on providing clinical services to individuals with diagnosable mental illnesses.
Over the past decade within the field of public health, there has been substantial interest in integrating mental health into public health practice.
Despite the enthusiasm about integrating mental health into mainstream public health practice, surprisingly little empirical research has examined how or why mental health is integrated into public health practice or assessed the impact of public health department activities on population mental health outcomes or determinants.
Scope of public health department activities to address population mental health.
Limited data exist about public health department engagement in mental health... Qualitative data and case studies offer more detailed information about the specific activities that LHDs perform to promote population mental health. These activities include conducting trainings about trauma-informed practice and monitoring population mental health status.
Behavioral health parity laws: statutory requirements for health insurance companies to provide equal benefits coverage for behavioral health and medical/surgical services.
Barriers and facilitators to public health department engagement in population mental health.
Few studies have examined barriers and facilitators to public health department engagement in mental health... Facilitators to LHD engagement in mental health might be emerging, however, as macrolevel trends in public health practice—including health department accreditation—could push mental health into mainstream public health practice.
Effects of public health department activities on population mental health.
While a growing body of evidence has demonstrated links between the activities of LHDs and physical health outcomes...
Strategies for health departments to monitor and assess population mental health.
Population mental health surveillance and monitoring are essential to effectively designing and deploying population-based interventions to improve mental health, especially during periods of acute stress, such as disasters and economic downturns. While many publicly available data sources can be used to generate population-level estimates of mental health status at state and local levels.
The use of big data has also emerged as a potential strategy for health departments to monitor population mental health.
Health Care System Approaches
Health care delivery systems are increasingly supplementing their clinical mental health service activities with population-based strategies to improve the mental health of those they serve. This shift reflects changes in health care financing that incentivize population health investments... Many of these systems-level strategies are novel, and evidence of their effects is still emerging.
Enhance the effectiveness of clinical mental health services.
Health care systems often implement systems-level strategies to improve the effectiveness of clinical mental health services. These interventions may be quality improvement initiatives such as training and coaching to promote the implementation of evidence-based practices, supports for measurement-based care to help providers evaluate patient progress and update treatment plans accordingly, and audit-feedback systems based on administrative data, such as feedback to reduce unnecessary antipsychotic prescribing. Health care systems can also support providers and improve patient outcomes by implementing care coordination programs. These can include the use of care managers who help ensure that patients can access needed mental health care and analytic efforts that use electronic health record data to help health care systems identify patients who might need mental health services. Other strategies focus on integrating mental health services into primary care. The collaborative care model is an effective and well-studied example of this approach.
Other effective models include the primary care behaviorist model, which integrates a psychologist into primary care, and the healthy steps for young children model, which integrates a developmental specialist into pediatric primary care. Some health care systems also work to engage individuals in community-based settings to provide early intervention services, promote sustained engagement with care, and initiate intensive services for complex needs.
Mental health can also be integrated into the practices of learning health care systems, which dynamically improve through rapid cycles of innovation, evaluation, and dissemination.
Provide consultation and training to community partners.
Health care systems can also deploy mental health providers to provide consultation and training to community-based partners and extend the impact of clinical interventions....Health care system–affiliated mental health providers can also help schools implement classroom-wide evidence-based interventions... Similarly, health care system–affiliated providers can assist with the development and implementation of evidence-based workplace mental health interventions in the communities they serve...
Employ paraprofessionals to address social needs and promote recovery.
Health care systems can provide nonclinical services that are effective at addressing prevention and recovery in mental health. Peer support specialists—people who have successfully lived with mental illness and help others recover in a formal and compensated capacity—can serve various functions within health care delivery systems, such as assisting with care navigation. Health care systems can also support prevention and recovery in mental health by employing other types of paraprofessionals, such as community health workers who can deliver nonclinical mental health interventions [e.g., psychoeducation or stress management training. Paraprofessionals can also help people with mental illness overcome barriers to recovery, such as through evidence-based, supported employment interventions that use a combination of clinical and nonclinical staff to help individuals access and maintain employment.
Recovery in mental health: a process through which people with mental illness gain hope, engage in an active life, and achieve personal autonomy and social identity.
Participate in accountable communities for health initiatives.
In the accountable communities for health model, a third-party nonprofit coordinates efforts among stakeholders in a community to advance a common goal, which can be population mental health. Health care systems can play a prominent role in these endeavors. With the accountable communities for health model, health care systems can invest to build capacity for collaboration around mental health and even invest in the other organizations to support complementary interventions. Some nonprofit health care systems make these investments to demonstrate community benefit, and some health care systems have created investment funds to enhance the capacity of community-based organizations to address population mental health.
Partner with public health departments.
Health care systems can also partner with public health departments and share data to inform planning activities. For example, to satisfy their community-benefit requirement, nonprofit hospitals can partner with health departments to fund population-based mental health interventions in the communities they serve... Health care systems can also share deidentified data to help public health departments and policy makers monitor and respond to emerging mental health issues... Like public health departments, health care systems can also advocate for evidence-supported public policy changes that have the potential to improve population mental health...
FUTURE DIRECTIONS
Near-term future directions include addressing emergent risks to population mental health and capitalizing on new opportunities to improve it. In terms of risks, there is an urgent need to prevent and mitigate the mental health effects of climate change. There is also a need to better understand, and intervene on, the mental health consequences of harmful social media exposures and stressful online interactions (e.g., cyberbullying), especially among youth and adolescents. However, there are also opportunities to use technology to improve population mental health. Smartphones can plausibly identify people experiencing serious mental distress, connect them to evidence-based mobile interventions, and help facilitate care management. Widespread implementation of population-based approaches to mental health is likely to require a collective shift in thinking at the societal level—from a view that conceptualizes mental health as an individual issue that is exclusively within the purview of psychologists and psychiatrists to one that conceptualizes mental health as a public health issue that actors and organizations across all sectors have a responsibility to address. Structural changes related to financing, training, and accreditation are also likely needed to institutionalize population-based approaches to mental health across sectors. More research is needed to better understand the impacts of population-based approaches to mental health to ensure they are effective and reduce, not exacerbate, disparities in mental health problems between socially disadvantaged and advantaged groups. While more evidence is needed, the state of the science is sufficient to recommend specific courses of action to improve population mental health.
Jonathan Purtle, Katherine L. Nelson, Nathaniel Z. Counts, Michael Yudell
Annu Rev Public Health. 2020 April 02; 41: 201–221.
INTRODUCTION
Approaches to addressing mental health issues in society have overwhelmingly focused on the provision of clinical services to individuals, not on fostering conditions that promote positive mental health, mental health promotion, or the primary prevention of mental illness.
Although clinical mental health services dramatically improve the lives of many people and their families, there are several reasons why the provision of clinical services in isolation is a suboptimal approach to maximizing the mental health of a population.
Positive mental health: sense of well-being, capacity to enjoy life, and the ability to deal with challenges—not only the absence of a mental health illness or condition
Mental health promotion: actions to improve quality of life and well-being, as opposed to ameliorating mental illness symptoms and mental health deficits
Primary prevention of mental illness: actions that address factors that might cause mental illnesses to avert their development
Most people who need mental health services do not receive them, in part because of workforce shortages. Estimates indicate that an additional 15,400 psychiatrists and 57,490 psychologists are needed by 2025 to meet the mental health service demand of the US population. Among people who do receive mental health services, there is a moderate likelihood that the services provided will not be evidence-based, implemented with fidelity, or effective. For these reasons, population-level increases in mental health service utilization are not associated with improvements in population mental health status. Finally, evidence suggests that much of the population burden of mental health problems can be prevented by reducing exposure to traumatic and chronic stressors, especially during key periods of child development. Taken together, these facts underscore the importance of complementing clinical approaches to mental health with population-based approaches that simultaneously affect entire groups of people.
The review is also focused on population-based approaches across three broad domains—public policy, public health practice, and health care system design—and does not focus on strategies for specific settings and populations (e.g., children in schools, people in prisons, older adults in elder care facilities).
Behavioral health: an umbrella term that refers to both mental health and substance use issues
Defining Interventions and Activities
Population-based interventions must be nonclinical and thus exclude direct mental health services (e.g., psychotherapies and pharmacological therapies) to individual patients.
Health care system-level interventions that address mental health, however, can be considered population-based because the intervention is at the system, as opposed to the clinical, level. Social, economic, and environmental policies are also considered population based interventions because they affect groups of people simultaneously, and psychiatric epidemiology studies indicate that a wide range of public policies affect mental health (detailed below). The definition includes mention of activities to encompass practices that monitor mental health outcomes and determinants without intervening on them
Psychiatric epidemiology: study of the incidence, prevalence, distribution, causes, and consequences of mental health conditions across people, space, and time
The interventions must also be implemented with the intent of addressing mental health outcomes or their determinants. This requirement stems from dictionary definitions of “approach”—“a way of doing or thinking about something such as a problem or a task”
This review draws from research about population-based interventions that affect mental health outcomes or determinants without the explicit intent of addressing them. These interventions are relevant because they could be implemented with the explicit intent of improving population mental health. The review also draws from research about population-based interventions that negatively affect mental health. Identifying these deleterious interventions is important because reforming them can produce benefits for population mental health.
Defining Outcomes and Determinants
Mental health outcomes can be conceptualized in many different ways—ranging from meeting full diagnostic criteria for a disorder in the DSM, to symptom severity of a disorder regardless of whether full DSM criteria are met, to general emotional distress, and across a continuum spanning from languishing to flourishing.... These include proximal determinants (e.g., poor sleep quality, exposure to traumatic stressors) as well as distal determinants (e.g., built environments with excessive ambient light and noise at night, high rates of community violence), which are the causes of the causes.
Defining Populations
In this review, the focus is on groups that share a geographic region (e.g., state or country), sociodemographic characteristics (e.g., ethnic or sexual minorities), or shared source of clinical service utilization (e.g., hospital, health care system). These types of groups encompass how populations are typically conceptualized in both public health and health care.
POPULATION-BASED APPROACHES TO MENTAL HEALTH AND THEIR EVIDENCE
Table 1 shows three broad domains in which population-based approaches to mental health can be implemented, identifies actors that are key to implementing these approaches, and summarizes core activities to these approaches. The text that follows provides detail about these approaches and evidence of their effectiveness.
Social, Economic, and Environmental Policy Approaches
In general, much more is known about the negative impacts of policies on mental health than about how policy can improve population mental health. This section provides a high-level summary of goals that can be advanced by public policy to improve the determinants of population mental health. The policy areas and approaches discussed in this section are not exhaustive, and each could be the focus of its own review.
Gene × environment interaction: when a person’s genetic predispositions for an outcome (e.g., mental illness) vary according to the environmental conditions to which they are exposed.
Reduce the incidence of traumatic events.
Exposures to traumatic events are well-established risk factors for post-traumatic stress disorder, depression, and a range of other mental health problems. Thus, policies that reduce the incidence of, and exposure to, traumatic events could substantially improve population mental health. Although not adopted with the explicit intent of improving mental health, evidence-based policies that prevent violent crime and accidental injuries—common traumatic events that carry high risk for mental health problems—might have the greatest impacts.
Stress: an individual’s mental, emotional, and physical response to demands or changes that require an adjustment.
Potentially traumatic events: experiencing, witnessing, or hearing about death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence.
Reduce the incidence of adverse childhood experiences.
Cumulative exposure to adverse childhood experiences (ACEs) increases risk for adult mental health problems.
Adverse childhood experiences: direct and indirect exposure to violence, abuse, neglect, and other forms of extreme stress before the age of 18—originally operationalized as ten indicators of “household dysfunction”
Modify the built environment.
Moderate evidence has shown that public policies can be used to improve population mental health by modifying three features of the built environment: green space, ambient light at night, and ambient noise. Exposure to green space, especially in urban areas, is associated with positive mental health, and policies that increase exposure could produce benefits by reducing stress, increasing physical activity, and preventing violent crime exposure.
Reduce financial and housing insecurity.
Associations between socioeconomic position and mental health are extremely complex, but evidence has shown that policies that promote financial and housing security among low-income populations could produce mental health benefits by reducing exposure to chronic stressors.
Public policy can also reduce stress among low-income groups and improve population mental health by reducing housing insecurity, such as through increasing public housing subsidies.
Reduce structural stigma toward people with mental illness and members of other social groups.
Structural stigma, which is often codified in policies, negatively affects population mental health though discrimination that inhibits access to resources and by fostering feelings of social exclusion and stress among socially marginalized groups. Identifying and reforming policies that create structural stigma is a strategy to improve population mental health. In terms of structural stigma toward people with mental illness, examples of policies to reform include those that prohibit people with mental illness from holding public office or practicing medicine.
In terms of other socially marginalized groups, numerous studies have demonstrated associations between policies that affect structural stigma toward sexual minorities and the mental health of these groups.
Structural stigma: societal conditions, cultural norms, and policies that constrain the opportunities, resources, and well-being of socially marginalized groups.
Structural racism: laws and system-level policies that limit racial minorities’ access to social and economic opportunities.
Public Health Practice Approaches
The United States has 59 state and territorial public health departments and more than 2,800 local public health departments (LHDs), all of which have a mandate to protect and promote population health. Although the structure and function of public health departments vary across the United States, most operate separately from their jurisdiction’s mental health agency.
Although mental health agencies in some jurisdictions have embraced a population-based approach—New York City and Philadelphia, for example—mental health agencies are usually narrowly focused on providing clinical services to individuals with diagnosable mental illnesses.
Over the past decade within the field of public health, there has been substantial interest in integrating mental health into public health practice.
Despite the enthusiasm about integrating mental health into mainstream public health practice, surprisingly little empirical research has examined how or why mental health is integrated into public health practice or assessed the impact of public health department activities on population mental health outcomes or determinants.
Scope of public health department activities to address population mental health.
Limited data exist about public health department engagement in mental health... Qualitative data and case studies offer more detailed information about the specific activities that LHDs perform to promote population mental health. These activities include conducting trainings about trauma-informed practice and monitoring population mental health status.
Behavioral health parity laws: statutory requirements for health insurance companies to provide equal benefits coverage for behavioral health and medical/surgical services.
Barriers and facilitators to public health department engagement in population mental health.
Few studies have examined barriers and facilitators to public health department engagement in mental health... Facilitators to LHD engagement in mental health might be emerging, however, as macrolevel trends in public health practice—including health department accreditation—could push mental health into mainstream public health practice.
Effects of public health department activities on population mental health.
While a growing body of evidence has demonstrated links between the activities of LHDs and physical health outcomes...
Strategies for health departments to monitor and assess population mental health.
Population mental health surveillance and monitoring are essential to effectively designing and deploying population-based interventions to improve mental health, especially during periods of acute stress, such as disasters and economic downturns. While many publicly available data sources can be used to generate population-level estimates of mental health status at state and local levels.
The use of big data has also emerged as a potential strategy for health departments to monitor population mental health.
Health Care System Approaches
Health care delivery systems are increasingly supplementing their clinical mental health service activities with population-based strategies to improve the mental health of those they serve. This shift reflects changes in health care financing that incentivize population health investments... Many of these systems-level strategies are novel, and evidence of their effects is still emerging.
Enhance the effectiveness of clinical mental health services.
Health care systems often implement systems-level strategies to improve the effectiveness of clinical mental health services. These interventions may be quality improvement initiatives such as training and coaching to promote the implementation of evidence-based practices, supports for measurement-based care to help providers evaluate patient progress and update treatment plans accordingly, and audit-feedback systems based on administrative data, such as feedback to reduce unnecessary antipsychotic prescribing. Health care systems can also support providers and improve patient outcomes by implementing care coordination programs. These can include the use of care managers who help ensure that patients can access needed mental health care and analytic efforts that use electronic health record data to help health care systems identify patients who might need mental health services. Other strategies focus on integrating mental health services into primary care. The collaborative care model is an effective and well-studied example of this approach.
Other effective models include the primary care behaviorist model, which integrates a psychologist into primary care, and the healthy steps for young children model, which integrates a developmental specialist into pediatric primary care. Some health care systems also work to engage individuals in community-based settings to provide early intervention services, promote sustained engagement with care, and initiate intensive services for complex needs.
Mental health can also be integrated into the practices of learning health care systems, which dynamically improve through rapid cycles of innovation, evaluation, and dissemination.
Provide consultation and training to community partners.
Health care systems can also deploy mental health providers to provide consultation and training to community-based partners and extend the impact of clinical interventions....Health care system–affiliated mental health providers can also help schools implement classroom-wide evidence-based interventions... Similarly, health care system–affiliated providers can assist with the development and implementation of evidence-based workplace mental health interventions in the communities they serve...
Employ paraprofessionals to address social needs and promote recovery.
Health care systems can provide nonclinical services that are effective at addressing prevention and recovery in mental health. Peer support specialists—people who have successfully lived with mental illness and help others recover in a formal and compensated capacity—can serve various functions within health care delivery systems, such as assisting with care navigation. Health care systems can also support prevention and recovery in mental health by employing other types of paraprofessionals, such as community health workers who can deliver nonclinical mental health interventions [e.g., psychoeducation or stress management training. Paraprofessionals can also help people with mental illness overcome barriers to recovery, such as through evidence-based, supported employment interventions that use a combination of clinical and nonclinical staff to help individuals access and maintain employment.
Recovery in mental health: a process through which people with mental illness gain hope, engage in an active life, and achieve personal autonomy and social identity.
Participate in accountable communities for health initiatives.
In the accountable communities for health model, a third-party nonprofit coordinates efforts among stakeholders in a community to advance a common goal, which can be population mental health. Health care systems can play a prominent role in these endeavors. With the accountable communities for health model, health care systems can invest to build capacity for collaboration around mental health and even invest in the other organizations to support complementary interventions. Some nonprofit health care systems make these investments to demonstrate community benefit, and some health care systems have created investment funds to enhance the capacity of community-based organizations to address population mental health.
Partner with public health departments.
Health care systems can also partner with public health departments and share data to inform planning activities. For example, to satisfy their community-benefit requirement, nonprofit hospitals can partner with health departments to fund population-based mental health interventions in the communities they serve... Health care systems can also share deidentified data to help public health departments and policy makers monitor and respond to emerging mental health issues... Like public health departments, health care systems can also advocate for evidence-supported public policy changes that have the potential to improve population mental health...
FUTURE DIRECTIONS
Near-term future directions include addressing emergent risks to population mental health and capitalizing on new opportunities to improve it. In terms of risks, there is an urgent need to prevent and mitigate the mental health effects of climate change. There is also a need to better understand, and intervene on, the mental health consequences of harmful social media exposures and stressful online interactions (e.g., cyberbullying), especially among youth and adolescents. However, there are also opportunities to use technology to improve population mental health. Smartphones can plausibly identify people experiencing serious mental distress, connect them to evidence-based mobile interventions, and help facilitate care management. Widespread implementation of population-based approaches to mental health is likely to require a collective shift in thinking at the societal level—from a view that conceptualizes mental health as an individual issue that is exclusively within the purview of psychologists and psychiatrists to one that conceptualizes mental health as a public health issue that actors and organizations across all sectors have a responsibility to address. Structural changes related to financing, training, and accreditation are also likely needed to institutionalize population-based approaches to mental health across sectors. More research is needed to better understand the impacts of population-based approaches to mental health to ensure they are effective and reduce, not exacerbate, disparities in mental health problems between socially disadvantaged and advantaged groups. While more evidence is needed, the state of the science is sufficient to recommend specific courses of action to improve population mental health.
Medicaid NCCI Policy Manual
General Background
The NCCI PTP edits and MUEs are used by state Medicaid agencies or fiscal agents to adjudicate provider claims for practitioner services, ambulatory surgical center services, outpatient hospital services, DME, prosthetics, orthotics, and supplies. NCCI edits are not applied to facility claims for inpatient services. The Medicare and Medicaid NCCI programs undergo continuous refinement with revised edit tables published quarterly. There is a process to address annual changes (additions, deletions, and modifications) of HCPCS/CPT codes and CPT Professional coding guidelines. Other sources of refinement are initiatives by CMS and comments CMS, AMA, national medical, surgical, and other health care societies/organizations, Medicare contractor medical directors, providers, consultants, other third-party payers, and other interested parties. Before implementing new edits, the NCCI program generally provides a 60-day review and comment period to representative national health care organizations that may be impacted by the edits and a 45-day review and comment period to the state Medicaid programs. However, there are situations when the NCCI program thinks that it is prudent to implement edits before completion of the review and comment period. The NCCI program evaluates the input from all sources and decides which edits are modified, deleted, or added each quarter.
General Background
The NCCI PTP edits and MUEs are used by state Medicaid agencies or fiscal agents to adjudicate provider claims for practitioner services, ambulatory surgical center services, outpatient hospital services, DME, prosthetics, orthotics, and supplies. NCCI edits are not applied to facility claims for inpatient services. The Medicare and Medicaid NCCI programs undergo continuous refinement with revised edit tables published quarterly. There is a process to address annual changes (additions, deletions, and modifications) of HCPCS/CPT codes and CPT Professional coding guidelines. Other sources of refinement are initiatives by CMS and comments CMS, AMA, national medical, surgical, and other health care societies/organizations, Medicare contractor medical directors, providers, consultants, other third-party payers, and other interested parties. Before implementing new edits, the NCCI program generally provides a 60-day review and comment period to representative national health care organizations that may be impacted by the edits and a 45-day review and comment period to the state Medicaid programs. However, there are situations when the NCCI program thinks that it is prudent to implement edits before completion of the review and comment period. The NCCI program evaluates the input from all sources and decides which edits are modified, deleted, or added each quarter.
How to Use the Medicaid National Correct Coding Initiative (NCCI) Tools
MLN9018659 December 2023
What’s the Medicaid NCCI?
MLN Booklet The Medicaid National Correct Coding Initiative (NCCI) promotes correct coding methodologies and reduces improper coding, with the overall goal of reducing improper payments of Medicaid claims.
The Medicaid NCCI includes 2 edit types:
1. Procedure-to-Procedure (PTP) Edits define pairs of HCPCS and CPT codes that providers shouldn’t report together for various reasons. PTP edits prevent improper payments when you report incorrect code combinations. Each edit has a Column 1 and a Column 2 HCPCS/CPT code. If you report the 2 codes of an edit pair for the same patient on the same date of service, the Column 1 code is eligible for payment, but the Column 2 code is denied, unless you use a proper modifier. We’ll learn more about modifiers later.
2. Medically Unlikely Edits (MUEs) define the maximum Units of Service (UOS) reported for a HCPCS/CPT code on the vast majority of appropriately reported claims by the same provider/supplier for the same beneficiary on the same date of service. MUEs prevent payment for an inappropriate number or quantity of the same service on a single day. Not all HCPCS/CPT codes have an MUE.
Note: The Medicaid National Correct Coding Initiative program has significant differences from the Medicare NCCI program. This booklet focuses on how to access and use the publicly available Medicaid NCCI files. If you’re looking for information on the Medicare NCCI program, visit the Medicare NCCI Edits webpage.
Differences between the 2 programs include:
● Some Medicare NCCI edits aren’t in the Medicaid NCCI program, while others are present but differ in some way from the Medicare NCCI edits
● Medicaid’s durable medical equipment (DME) NCCI PTP edits are specific to the Medicaid Program, in other words, the Medicare NCCI program doesn’t have DME NCCI PTP edits
● The Medicaid NCCI program has unique edits, for example, edits for codes not covered or not separately payable by the Medicare Program
● Unlike Medicare, for which most MUE edits are applied based on the date of service, Medicaid applies MUEs separately to each line of a claim
Note: Medicaid coding NCCI edit decisions are based on:
• Conventions defined in the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Professional
• National and local policies and edits
• Coding guidelines developed by national health care organizations
• Analysis of standard medical and surgical practices
• Review of current coding practices
MLN9018659 December 2023
What’s the Medicaid NCCI?
MLN Booklet The Medicaid National Correct Coding Initiative (NCCI) promotes correct coding methodologies and reduces improper coding, with the overall goal of reducing improper payments of Medicaid claims.
The Medicaid NCCI includes 2 edit types:
1. Procedure-to-Procedure (PTP) Edits define pairs of HCPCS and CPT codes that providers shouldn’t report together for various reasons. PTP edits prevent improper payments when you report incorrect code combinations. Each edit has a Column 1 and a Column 2 HCPCS/CPT code. If you report the 2 codes of an edit pair for the same patient on the same date of service, the Column 1 code is eligible for payment, but the Column 2 code is denied, unless you use a proper modifier. We’ll learn more about modifiers later.
2. Medically Unlikely Edits (MUEs) define the maximum Units of Service (UOS) reported for a HCPCS/CPT code on the vast majority of appropriately reported claims by the same provider/supplier for the same beneficiary on the same date of service. MUEs prevent payment for an inappropriate number or quantity of the same service on a single day. Not all HCPCS/CPT codes have an MUE.
Note: The Medicaid National Correct Coding Initiative program has significant differences from the Medicare NCCI program. This booklet focuses on how to access and use the publicly available Medicaid NCCI files. If you’re looking for information on the Medicare NCCI program, visit the Medicare NCCI Edits webpage.
Differences between the 2 programs include:
● Some Medicare NCCI edits aren’t in the Medicaid NCCI program, while others are present but differ in some way from the Medicare NCCI edits
● Medicaid’s durable medical equipment (DME) NCCI PTP edits are specific to the Medicaid Program, in other words, the Medicare NCCI program doesn’t have DME NCCI PTP edits
● The Medicaid NCCI program has unique edits, for example, edits for codes not covered or not separately payable by the Medicare Program
● Unlike Medicare, for which most MUE edits are applied based on the date of service, Medicaid applies MUEs separately to each line of a claim
Note: Medicaid coding NCCI edit decisions are based on:
• Conventions defined in the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Professional
• National and local policies and edits
• Coding guidelines developed by national health care organizations
• Analysis of standard medical and surgical practices
• Review of current coding practices
CHAPTER XI MEDICINE EVALUATION AND MANAGEMENT SERVICES CPT CODES 90000 – 99999 MEDICAID NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL
Revision Date (Medicaid): 1/1/2024
C. Psychiatric Services
CPT codes for psychiatric services include diagnostic (CPT codes 90791, 90792) and therapeutic (individual, group, other) procedures. Since psychotherapy includes continuing psychiatric evaluation, CPT codes 90791 and 90792 are not separately reportable with individual, group, family, crisis, or other psychotherapy codes for the same date of service.
CPT codes 90832-90838 include all psychotherapy of a patient with family members as informants, if present, for a single date of service. Family psychotherapy, (e.g., CPT codes 90846, 90847) focused on the patient addressing interactions between the patient and family members may be reported separately with psychotherapy CPT codes 90832-90838 on the same date of service if performed as a separate and distinct service during a separate time interval.
Interactive services (diagnostic or therapeutic) are distinct services for patients who have "lost, or have not yet developed either the expressive language communication skills to explain his/her symptoms and response to treatment..." Interactive complexity to psychiatric services is reported with add-on CPT code 90785.
Diagnostic psychiatric evaluation is reported with 1 of 2 CPT codes. CPT code 90791 is psychiatric evaluation without medical E&M, and CPT code 90792 is psychiatric evaluation with medical E&M. E&M codes (e.g., 99202-99215) shall not be reported with either of these diagnostic psychiatric codes.
Individual psychotherapy codes are time-based codes. There are separate codes for psychotherapy without E&M service (CPT codes 90832, 90834, 90837) and Add-on Codes (AOCs) (CPT codes 90833, 90836, 90838) for psychotherapy to be reported in conjunction with the appropriate E&M code.
For practitioner services, E&M codes are separately reportable on the same date of service as psychoanalysis (CPT code 90845), narcosynthesis (CPT code 90865), or hypnotherapy (CPT code 90880) only if the E&M service is separate and distinct from the psychiatric service.
Revision Date (Medicaid): 1/1/2024
C. Psychiatric Services
CPT codes for psychiatric services include diagnostic (CPT codes 90791, 90792) and therapeutic (individual, group, other) procedures. Since psychotherapy includes continuing psychiatric evaluation, CPT codes 90791 and 90792 are not separately reportable with individual, group, family, crisis, or other psychotherapy codes for the same date of service.
CPT codes 90832-90838 include all psychotherapy of a patient with family members as informants, if present, for a single date of service. Family psychotherapy, (e.g., CPT codes 90846, 90847) focused on the patient addressing interactions between the patient and family members may be reported separately with psychotherapy CPT codes 90832-90838 on the same date of service if performed as a separate and distinct service during a separate time interval.
Interactive services (diagnostic or therapeutic) are distinct services for patients who have "lost, or have not yet developed either the expressive language communication skills to explain his/her symptoms and response to treatment..." Interactive complexity to psychiatric services is reported with add-on CPT code 90785.
Diagnostic psychiatric evaluation is reported with 1 of 2 CPT codes. CPT code 90791 is psychiatric evaluation without medical E&M, and CPT code 90792 is psychiatric evaluation with medical E&M. E&M codes (e.g., 99202-99215) shall not be reported with either of these diagnostic psychiatric codes.
Individual psychotherapy codes are time-based codes. There are separate codes for psychotherapy without E&M service (CPT codes 90832, 90834, 90837) and Add-on Codes (AOCs) (CPT codes 90833, 90836, 90838) for psychotherapy to be reported in conjunction with the appropriate E&M code.
For practitioner services, E&M codes are separately reportable on the same date of service as psychoanalysis (CPT code 90845), narcosynthesis (CPT code 90865), or hypnotherapy (CPT code 90880) only if the E&M service is separate and distinct from the psychiatric service.
CHAPTER XII SUPPLEMENTAL SERVICES HCPCS LEVEL II CODES A0000 – V9999 FOR MEDICAID NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL
Revision Date (Medicaid): 1/1/2024
B. Evaluation & Management (E&M) Services
Physician services can be categorized as either major surgical procedures, minor surgical procedures, non-surgical procedures, or Evaluation & Management (E&M) services. This section summarizes some of the rules for reporting E&M services in relation to major surgical, minor surgical, and non-surgical procedures. Even in the absence of NCCI PTP edits, providers shall bill for their services following these rules.
An E&M service is separately reportable on the same date of service as a major or minor surgical procedure under limited circumstances. If an E&M service is performed on the same date of service as a major surgical procedure to decide whether to perform this surgical procedure, the E&M service is separately reportable with modifier 57. Other preoperative E&M services on the same date of service as a major surgical procedure are included in the global package for the procedure and are not separately reportable. There are currently no NCCI PTP edits based on this rule. In general, E&M services performed on the same date of service as a minor surgical procedure are included in the payment for the procedure. The decision to perform a minor surgical procedure is included in the payment for the minor surgical procedure and shall not be reported separately as an E&M service. However, a significant and separately identifiable E&M service unrelated to the decision to perform a minor surgical procedure is separately reportable with modifier 25. The E&M service and minor surgical procedure do not require different diagnoses. If a minor surgical procedure is performed on a new patient, the same rules for reporting E&M services apply. The fact that the patient is “new” to the provider is not sufficient alone to justify reporting an E&M service on the same date of service as a minor surgical procedure. The NCCI program contains many but not all, possible edits based on these principles. For major and minor surgical procedures, postoperative E&M services related to recovery from the surgical procedure during the postoperative period are included in the global package as are E&M services related to complications of the surgery. Postoperative visits unrelated to the diagnosis for which the surgical procedure was performed unless related to a complication of surgery may be reported separately on the same day as a surgical procedure with modifier 24 (“Unrelated Evaluation and Management Service by the same Physician or Other Qualified Health Care Professional During a Postoperative Period”).
Many non-surgical procedures are performed by physicians and have inherent pre-procedure, intra-procedure, and post-procedure work usually performed each time the procedure is completed. This work shall not be reported as a separate E&M code.
Other non-surgical procedures are not usually performed by a physician and have no physician work associated with them. A physician shall not report a separate E&M code with these procedures for the supervision of others performing the procedure or for the interpretation of the procedure. With most non-surgical procedures, the physician may, however, perform a significant and separately identifiable E&M service that is above and beyond the usual pre- and post-operative work of the procedure on the same date of service which may be reported by appending modifier 25 to the E&M code. This E&M service may be related to the same diagnosis necessitating performance of the non-surgical procedure but cannot include any work inherent in the non-surgical procedure, supervision of others performing the non-surgical procedure, or time for interpreting the result of the non-surgical procedure.
BING
Evaluation and Management (E&M) services play a vital role in healthcare. These services involve cognitive (non-procedural) tasks performed by physicians and other qualified healthcare professionals to diagnose and treat illnesses or injuries. Here are some key points about E&M services:
Medical decision making (MDM) is a critical aspect of healthcare practice. Let’s explore it further:
Revision Date (Medicaid): 1/1/2024
B. Evaluation & Management (E&M) Services
Physician services can be categorized as either major surgical procedures, minor surgical procedures, non-surgical procedures, or Evaluation & Management (E&M) services. This section summarizes some of the rules for reporting E&M services in relation to major surgical, minor surgical, and non-surgical procedures. Even in the absence of NCCI PTP edits, providers shall bill for their services following these rules.
An E&M service is separately reportable on the same date of service as a major or minor surgical procedure under limited circumstances. If an E&M service is performed on the same date of service as a major surgical procedure to decide whether to perform this surgical procedure, the E&M service is separately reportable with modifier 57. Other preoperative E&M services on the same date of service as a major surgical procedure are included in the global package for the procedure and are not separately reportable. There are currently no NCCI PTP edits based on this rule. In general, E&M services performed on the same date of service as a minor surgical procedure are included in the payment for the procedure. The decision to perform a minor surgical procedure is included in the payment for the minor surgical procedure and shall not be reported separately as an E&M service. However, a significant and separately identifiable E&M service unrelated to the decision to perform a minor surgical procedure is separately reportable with modifier 25. The E&M service and minor surgical procedure do not require different diagnoses. If a minor surgical procedure is performed on a new patient, the same rules for reporting E&M services apply. The fact that the patient is “new” to the provider is not sufficient alone to justify reporting an E&M service on the same date of service as a minor surgical procedure. The NCCI program contains many but not all, possible edits based on these principles. For major and minor surgical procedures, postoperative E&M services related to recovery from the surgical procedure during the postoperative period are included in the global package as are E&M services related to complications of the surgery. Postoperative visits unrelated to the diagnosis for which the surgical procedure was performed unless related to a complication of surgery may be reported separately on the same day as a surgical procedure with modifier 24 (“Unrelated Evaluation and Management Service by the same Physician or Other Qualified Health Care Professional During a Postoperative Period”).
Many non-surgical procedures are performed by physicians and have inherent pre-procedure, intra-procedure, and post-procedure work usually performed each time the procedure is completed. This work shall not be reported as a separate E&M code.
Other non-surgical procedures are not usually performed by a physician and have no physician work associated with them. A physician shall not report a separate E&M code with these procedures for the supervision of others performing the procedure or for the interpretation of the procedure. With most non-surgical procedures, the physician may, however, perform a significant and separately identifiable E&M service that is above and beyond the usual pre- and post-operative work of the procedure on the same date of service which may be reported by appending modifier 25 to the E&M code. This E&M service may be related to the same diagnosis necessitating performance of the non-surgical procedure but cannot include any work inherent in the non-surgical procedure, supervision of others performing the non-surgical procedure, or time for interpreting the result of the non-surgical procedure.
BING
Evaluation and Management (E&M) services play a vital role in healthcare. These services involve cognitive (non-procedural) tasks performed by physicians and other qualified healthcare professionals to diagnose and treat illnesses or injuries. Here are some key points about E&M services:
- Nature of E&M Services:
- E&M services focus on diagnosis, treatment, and patient management.
- Nearly all physicians provide E&M services, and they are an integral part of medical practice.
- Infectious diseases physicians, for instance, often engage in E&M services.
- Coding and Billing:
- E/M coding translates physician-patient encounters into CPT codes for billing purposes.
- These codes reflect the complexity and nature of the patient’s visit.
- For example, the 99214 code may be used for an office visit with an established patient1.
- Recent Changes:
- The Centers for Medicare & Medicaid Services (CMS) have made significant revisions to E&M services.
- Physicians can now select the E/M visit level based on either:
- Total time spent during the patient encounter.
- Medical decision making used in providing care2.
Medical decision making (MDM) is a critical aspect of healthcare practice. Let’s explore it further:
- Defining Goals:
- Before conducting complex, costly, or potentially risky tests, physicians engage in detailed conversations with patients about the goals of diagnostic and treatment plans.
- These goals typically involve identifying and curing diseases.
- Standard of Care and Second Opinions:
- Physicians adhere to a standard of care, which represents the accepted practices within the medical community.
- Seeking second opinions is common, especially for significant medical decisions.
- Information Sources:
- For Doctors:
- Physicians rely on various sources, including medical literature, clinical guidelines, and expert consultations.
- Evidence-based medicine plays a crucial role in informed decision making.
- For Patients:
- Patients can access reliable information from sources such as trusted websites, patient education materials, and discussions with healthcare providers.
- For Doctors:
1995 DOCUMENTATION GUIDELINES FOR EVALUATION AND MANAGEMENT SERVICES
WHAT DO PAYERS WANT AND WHY?
Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate:
the site of service;
the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or
that services provided have been accurately reported.
II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION
The principles of documentation listed below are applicable to all types of medical and surgical services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. The general principles listed below may be modified to account for these variable circumstances in providing E/M services.
1. The medical record should be complete and legible.
2. The documentation of each patient encounter should include: reason for the encounter and relevant history, physical examination findings, and prior diagnostic test results; assessment, clinical impression, or diagnosis; plan for care; and date and legible identity of the observer.
3. If not documented, the rationale for ordering diagnostic and other ancillary services should be easily inferred.
4. Past and present diagnoses should be accessible to the treating and/or consulting physician.
5. Appropriate health risk factors should be identified.
6. The patient's progress, response to and changes in treatment, and revision of diagnosis should be documented.
7. The CPT and ICD-9-CM codes reported on the health insurance claim form or billing statement should be supported by the documentation in the medical record.
WHAT DO PAYERS WANT AND WHY?
Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate:
the site of service;
the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or
that services provided have been accurately reported.
II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION
The principles of documentation listed below are applicable to all types of medical and surgical services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. The general principles listed below may be modified to account for these variable circumstances in providing E/M services.
1. The medical record should be complete and legible.
2. The documentation of each patient encounter should include: reason for the encounter and relevant history, physical examination findings, and prior diagnostic test results; assessment, clinical impression, or diagnosis; plan for care; and date and legible identity of the observer.
3. If not documented, the rationale for ordering diagnostic and other ancillary services should be easily inferred.
4. Past and present diagnoses should be accessible to the treating and/or consulting physician.
5. Appropriate health risk factors should be identified.
6. The patient's progress, response to and changes in treatment, and revision of diagnosis should be documented.
7. The CPT and ICD-9-CM codes reported on the health insurance claim form or billing statement should be supported by the documentation in the medical record.
MEDICAID.GOV
Behavioral Health Services
Medicaid is the single largest payer for mental health services in the United States and is increasingly playing a larger role in the reimbursement of substance use disorder services. Individuals with a behavioral health disorder also utilize significant health care services—nearly 12 million visits made to U.S. hospital emergency departments in 2007 involved individuals with a mental disorder, substance abuse problem, or both.
This new and revised section of the Medicaid.gov website that provides information to States, managed care organizations, providers, beneficiaries and others regarding mental health and substance use disorder—referred to as behavioral health services. This site provides information regarding services and supports to meet the health, behavioral health and long term services and support needs of Medicaid individuals with mental health or substance use disorders. This website has been organized around several key areas that the Centers for Medicaid and CHIP Services (CMCS) has identified as a priority for the next several years:
- Effective benefit design for mental health services for children, youth and their families
- Effective benefit design for substance use disorder services
- Mental Health Parity and Addiction Equity Act (MHPAEA) application to Medicaid programs
Pathways for Covering Mental Health and Substance Use Disorder Services
The following federal authorities offer states the flexibility to transform their systems and improve coverage for individuals with mental health or substance use disorder (MH/SUD) conditions:
1. Coordinating physical and behavioral health
A primary goal of MH/SUD system reform is to encourage care models that thoughtfully integrate primary care. As part of an interdisciplinary approach to improving the delivery of behavioral, mental and physical health services to individuals with MH/SUD, states are encouraged develop a clear approach for integrating primary care. Entry into treatment for mental health conditions and/or substance use disorder should serve as a touch point for access to primary care or specialist services and vice versa. An uptick in ambulatory care utilization is generally seen as a favorable outcome for individuals engaging in treatment. CMS encourages states to submit proposals that integrate MH/SUD services and medical care, in concert with acute treatment and continuously throughout long-term treatment and recovery.
a. Health Home for Enrollees with Chronic Conditions
This provision offers important coordinated care opportunities for supporting physical and behavioral health, as well as linkages to long-term supports, which are fundamental elements of a successful health home.
b. Integrated Care Models (ICM)
ICMs are characterized by organized and accountable care delivery and payment methodologies aligned across payers and providers to ensure effective, seamless, and coordinated care. By orienting the system around the needs and preferences of beneficiaries, successful ICMs can demonstrate improved health care outcomes and result in improved beneficiary experience, while reducing overall health care expenditures. ICMs include integration of various types of health care services such as primary, acute, specialty, dental, behavioral, and long-term support services. To implement ICMs within Medicaid programs, states may seek to explore new initiatives or enhance existing efforts under a Medicaid state plan, or use demonstration or waiver authority.
c. Managed Care Organization
States can contract with Managed Care Organizations (MCOs) who offer care coordination to individuals, including individuals that have primary care, behavioral health and long term services and supports. States can use a managed care delivery system by getting a state plan amendment under 1932 of the Social Security Act (SSA) or 1915(b) approved by CMS. The state plan includes information such as the types of entities that will be used and what groups of people will be enrolled. Many states are interested in testing shared savings methodologies in the Medicaid program as a means to promote better coordination efforts. CMS has issues guidance that focuses specifically on reimbursement methodologies that can be adopted in the context of integrated care models to incentivize improved quality and outcomes and reduce costs by sharing program savings with high performing providers. Information regarding the Medicaid Shared Savings Program can be found at http://www.medicaid.gov/Federal-Policy-Guidance/Downloads/SMD-13-005.pdf
2. Expanding the availability of recovery services
a. Section 1915(i) State Plan Home and Community-Based Services (HCBS)
b. Section 1915(b) Managed Care Options
c. Section 1115(a) Demonstration Projects
3. Traditional Health and Behavioral Health Benefits
a. Section 1905(a) State Plan Authority
b. Alternative Benefit Plan
Home & Community Based Services 1915(i)
States can offer a variety of services under a State Plan Home and Community Based Services (HCBS) benefit. People must meet state-defined criteria based on need and typically get a combination of acute-care medical services (like dental services, skilled nursing services) and long-term services (like respite, case management, supported employment and environmental modifications) in home and community-based settings.
Section 223 Demonstration Program to Improve Community Mental Health Services
Updated Certified Community Behavioral Health Clinic (CCBHC) Prospective Payment System (PPS) Technical Guidance
CCBHC PPS Guidance Proposed UpdatesThe Centers for Medicare & Medicaid Services is seeking public comment on proposed updates to the Certified Community Behavioral Health Clinic (CCBHC) Prospective Payment System (PPS) Technical Guidance published as part of the Substance Abuse and Mental Health Services (SAMSHA) CCBHC 2015 Notice of Funding Opportunity.
A summary of the proposed updates include:
- Simplifying the PPS-2 methodology to make special population rates optional,
- Addition of two new PPS rate options (PPS-3, daily; PPS-4, monthly) which includes a Special Crisis Service rate component,
- Updating the quality bonus payment measure-set and providing clarification and examples regarding flexibilities for quality bonus payments,
- Updating specific sections of the existing CCBHC PPS Guidance to bring it up-to-date, and provide additional flexibilities as allowable under the Demonstration, and
- Establishing a standard 3-year cadence for states to rebase clinic-specific PPS rates.
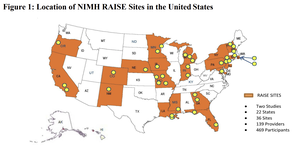
Coverage of Early Intervention Services for First Episode Psychosis
This Informational Bulletin is intended to assist states in designing a benefit package to guide early treatment intervention options that will meet the needs of youth and young adults experiencing first episode psychosis. The National Institute of Mental Health (NIMH), Centers for Medicare & Medicaid Services’ Center for Medicaid and CHIP Services (CMCS) and Substance Abuse and Mental Health Services Administration (SAMHSA) are engaged in an ongoing partnership to further efforts to support early intervention services for youth and young adults that experience first episode psychosis.
Schizophrenia is associated with high rates of morbidity and mortality. In the U.S., people diagnosed with psychotic disorders such as schizophrenia die an average of 11 years earlier than the general population, typically due to co-occurring medical conditions. Up to 10 percent of individuals with schizophrenia die by suicide, often in the early years of illness.
Eighty to 90% of people with schizophrenia are unemployed, 20% are homeless, and 17% live in prison or jail. Approximately 100,000 adolescents and young adults in the U.S. experience first episode psychosis each year. Psychotic symptoms usually emerge during late adolescence or early adulthood, and derail important developmental milestones such as completing school or entering the workforce. The early stages of psychotic illness are tumultuous, and may place tremendous strain on a family’s emotional and financial resources.
Untreated psychosis increases a person’s risk for suicide, involuntary emergency care, and poor clinical outcomes. Often individuals experience long periods of untreated psychosis and treatment delays are between one and three years following the onset of psychotic symptoms. In the U.S., a recent study of the duration of untreated psychosis reported a median rate of 74 weeks across 34 geographically diverse community mental health centers, a level more than six times the World Health Organization standard for effective early psychosis intervention.
Early intervention can alter this illness trajectory and enable individuals experiencing first episode psychosis to live in community settings and participate fully in family and community life.
Evidence-based services such as the integrated, team-based mental health services described in this document support clinical and functional recovery by reducing the severity of first episode psychotic symptoms, keeping individuals in school or at work, and putting them on a path to better health.
Compared to traditional treatment approaches, specialty care programs that provide coordinated, targeted treatment in the early stages of illness and integrate medical, psychological, and rehabilitation interventions, are an effective means for treating first episode psychosis.Without such interventions during a first episode, the typical course of psychotic disorder involves multiple episodes of acute mental illness, with accumulating disability between periods of active psychosis and increased long-term health care costs.
NIMH launched the Recovery After an Initial Schizophrenia Episode (RAISE) research initiative in 2008 with the aim of developing, testing, and implementing Coordinated Specialty Care (CSC) programs for first episode psychosis in “real world” community clinics. Under RAISE, NIMH funded two research investigations: the RAISE Early Treatment Program (RAISE-ETP) and the RAISE Implementation and Evaluation Study (RAISE-IES). Figure 1 illustrates the 22 states in the RAISE initiative, which included 36 geographically diverse community clinics.
The RAISE-ETP randomized control trial involved 404 young people with first episode psychosis in 34 community clinics. Community-based clinicians were trained to deliver a teambased approach to CSC that included four core interventions: resilience-focused individual therapy, family psychoeducation and support, supported education and employment, and personalized medication management. Compared to patients who received usual care, participants in CSC experienced significantly greater improvements in total symptoms, social functioning, work or school involvement, and overall quality of life.
Individuals with a shorter duration of untreated psychosis benefited most from CSC treatment, demonstrating that receipt of appropriate care early in the course of a first episode of psychotic disorder is essential to improved outcomes.
This Informational Bulletin is intended to assist states in designing a benefit package to guide early treatment intervention options that will meet the needs of youth and young adults experiencing first episode psychosis. The National Institute of Mental Health (NIMH), Centers for Medicare & Medicaid Services’ Center for Medicaid and CHIP Services (CMCS) and Substance Abuse and Mental Health Services Administration (SAMHSA) are engaged in an ongoing partnership to further efforts to support early intervention services for youth and young adults that experience first episode psychosis.
Schizophrenia is associated with high rates of morbidity and mortality. In the U.S., people diagnosed with psychotic disorders such as schizophrenia die an average of 11 years earlier than the general population, typically due to co-occurring medical conditions. Up to 10 percent of individuals with schizophrenia die by suicide, often in the early years of illness.
Eighty to 90% of people with schizophrenia are unemployed, 20% are homeless, and 17% live in prison or jail. Approximately 100,000 adolescents and young adults in the U.S. experience first episode psychosis each year. Psychotic symptoms usually emerge during late adolescence or early adulthood, and derail important developmental milestones such as completing school or entering the workforce. The early stages of psychotic illness are tumultuous, and may place tremendous strain on a family’s emotional and financial resources.
Untreated psychosis increases a person’s risk for suicide, involuntary emergency care, and poor clinical outcomes. Often individuals experience long periods of untreated psychosis and treatment delays are between one and three years following the onset of psychotic symptoms. In the U.S., a recent study of the duration of untreated psychosis reported a median rate of 74 weeks across 34 geographically diverse community mental health centers, a level more than six times the World Health Organization standard for effective early psychosis intervention.
Early intervention can alter this illness trajectory and enable individuals experiencing first episode psychosis to live in community settings and participate fully in family and community life.
Evidence-based services such as the integrated, team-based mental health services described in this document support clinical and functional recovery by reducing the severity of first episode psychotic symptoms, keeping individuals in school or at work, and putting them on a path to better health.
Compared to traditional treatment approaches, specialty care programs that provide coordinated, targeted treatment in the early stages of illness and integrate medical, psychological, and rehabilitation interventions, are an effective means for treating first episode psychosis.Without such interventions during a first episode, the typical course of psychotic disorder involves multiple episodes of acute mental illness, with accumulating disability between periods of active psychosis and increased long-term health care costs.
NIMH launched the Recovery After an Initial Schizophrenia Episode (RAISE) research initiative in 2008 with the aim of developing, testing, and implementing Coordinated Specialty Care (CSC) programs for first episode psychosis in “real world” community clinics. Under RAISE, NIMH funded two research investigations: the RAISE Early Treatment Program (RAISE-ETP) and the RAISE Implementation and Evaluation Study (RAISE-IES). Figure 1 illustrates the 22 states in the RAISE initiative, which included 36 geographically diverse community clinics.
The RAISE-ETP randomized control trial involved 404 young people with first episode psychosis in 34 community clinics. Community-based clinicians were trained to deliver a teambased approach to CSC that included four core interventions: resilience-focused individual therapy, family psychoeducation and support, supported education and employment, and personalized medication management. Compared to patients who received usual care, participants in CSC experienced significantly greater improvements in total symptoms, social functioning, work or school involvement, and overall quality of life.
Individuals with a shorter duration of untreated psychosis benefited most from CSC treatment, demonstrating that receipt of appropriate care early in the course of a first episode of psychotic disorder is essential to improved outcomes.
Maternal Depression Screening and Treatment: A Critical Role for Medicaid in the Care of Mothers and Children
Introduction
This Informational Bulletin discusses the importance of early screening for maternal depression and clarifies the pivotal role Medicaid can play in identifying children with mothers who experience depression and its consequences, and connecting mothers and children to the help they need. State Medicaid agencies may cover maternal depression screening as part of a wellchild visit. In addition, states must cover any medically necessary treatment for the child as part of the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit.
Prevalence and Impact of Maternal Depression
Maternal depression is a serious and widespread condition that not only affects the mother, but may have a lasting, detrimental impact on the child’s health. Maternal depression presents a significant early risk to proper child development, the mother-infant bond, and the family. Maternal depression screening and treatment is an important tool to protect the child from the potential adverse physical and developmental effects of maternal depression. According to the American Academy of Pediatrics (AAP), screening mothers for maternal depression is a best practice for primary care pediatricians caring for infants and their families1 and can be integrated into the well-child care schedule, as well as included in the prenatal visit.
Maternal depression is characterized by a spectrum of severity: the common “maternity blues” or “baby blues” are usually gone after a few days or one to two weeks and are helped with reassurance and support for the mother.
In light of recent evidence that children living with mothers with depression may be at risk for long-term physical and behavioral health consequences, the importance of screening and treating maternal depression is clear.
Medicaid’s Role in Maternal Depression Screening and Treatment
Diagnostic and Treatment Services
If a problem is identified as a result of an EPSDT screen, states have an obligation to arrange for medically necessary diagnostic and treatment services to address the child’s needs.15 Diagnostic and treatment services directed solely at the mother would be coverable under the Medicaid program only if the mother is Medicaid eligible. Mothers who are not Medicaid eligible may receive some benefit from diagnostic and treatment services directed at treating the health and well-being of the child (such as family therapy services) to reduce or treat the effects of the mother’s condition on the child. Consistent with current policy regarding services provided for the “direct benefit of the child,” such diagnostic and treatment services must actively involve the child, be directly related to the needs of the child and such treatment must be delivered to the child and mother together, but can be claimed as a direct service for the child. Such services also must be coverable under one or more section 1905(a) benefit categories such as rehabilitative services or other licensed practitioner services.
State Medicaid agencies should encourage the child’s provider to refer mothers for other appropriate care, including diagnosis, therapy and/or medication. Mothers who are Medicaid eligible should be referred to their primary care providers or other appropriate providers. Mothers who are ineligible for Medicaid, or lose their eligibility 60 days postpartum, can be referred to community resources that offer appropriate mental health services, such as community mental health programs, federally qualified health centers or other programs that may exist in the community.
Promoting Maternal Depression Screening Under Medicaid
Conclusion
Maternal depression can take a substantial toll on the health and well-being of both mothers and children, and can increase related health costs, impede the development of the child, and create negative social consequences. Maternal depression screening during the well-child visit is considered a pediatric best practice and is a simple way to identify mothers who may be suffering from depression and may lead to treatment for the child or referral for mothers to other appropriate treatment. In addition to covering this screening for Medicaid eligible mothers, states may cover maternal depression screening for non-Medicaid eligible mothers during the well-child visit. States may also cover treatment for the mother when both the child and the mother are present, treatment focuses on the effects of the mother’s condition on the child, and services are for the direct benefit of the child.
Introduction
This Informational Bulletin discusses the importance of early screening for maternal depression and clarifies the pivotal role Medicaid can play in identifying children with mothers who experience depression and its consequences, and connecting mothers and children to the help they need. State Medicaid agencies may cover maternal depression screening as part of a wellchild visit. In addition, states must cover any medically necessary treatment for the child as part of the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit.
Prevalence and Impact of Maternal Depression
Maternal depression is a serious and widespread condition that not only affects the mother, but may have a lasting, detrimental impact on the child’s health. Maternal depression presents a significant early risk to proper child development, the mother-infant bond, and the family. Maternal depression screening and treatment is an important tool to protect the child from the potential adverse physical and developmental effects of maternal depression. According to the American Academy of Pediatrics (AAP), screening mothers for maternal depression is a best practice for primary care pediatricians caring for infants and their families1 and can be integrated into the well-child care schedule, as well as included in the prenatal visit.
Maternal depression is characterized by a spectrum of severity: the common “maternity blues” or “baby blues” are usually gone after a few days or one to two weeks and are helped with reassurance and support for the mother.
In light of recent evidence that children living with mothers with depression may be at risk for long-term physical and behavioral health consequences, the importance of screening and treating maternal depression is clear.
Medicaid’s Role in Maternal Depression Screening and Treatment
Diagnostic and Treatment Services
If a problem is identified as a result of an EPSDT screen, states have an obligation to arrange for medically necessary diagnostic and treatment services to address the child’s needs.15 Diagnostic and treatment services directed solely at the mother would be coverable under the Medicaid program only if the mother is Medicaid eligible. Mothers who are not Medicaid eligible may receive some benefit from diagnostic and treatment services directed at treating the health and well-being of the child (such as family therapy services) to reduce or treat the effects of the mother’s condition on the child. Consistent with current policy regarding services provided for the “direct benefit of the child,” such diagnostic and treatment services must actively involve the child, be directly related to the needs of the child and such treatment must be delivered to the child and mother together, but can be claimed as a direct service for the child. Such services also must be coverable under one or more section 1905(a) benefit categories such as rehabilitative services or other licensed practitioner services.
State Medicaid agencies should encourage the child’s provider to refer mothers for other appropriate care, including diagnosis, therapy and/or medication. Mothers who are Medicaid eligible should be referred to their primary care providers or other appropriate providers. Mothers who are ineligible for Medicaid, or lose their eligibility 60 days postpartum, can be referred to community resources that offer appropriate mental health services, such as community mental health programs, federally qualified health centers or other programs that may exist in the community.
Promoting Maternal Depression Screening Under Medicaid
Conclusion
Maternal depression can take a substantial toll on the health and well-being of both mothers and children, and can increase related health costs, impede the development of the child, and create negative social consequences. Maternal depression screening during the well-child visit is considered a pediatric best practice and is a simple way to identify mothers who may be suffering from depression and may lead to treatment for the child or referral for mothers to other appropriate treatment. In addition to covering this screening for Medicaid eligible mothers, states may cover maternal depression screening for non-Medicaid eligible mothers during the well-child visit. States may also cover treatment for the mother when both the child and the mother are present, treatment focuses on the effects of the mother’s condition on the child, and services are for the direct benefit of the child.
BILLING AND CODING GUIDANCE IN MEDICAID HEALTHCARE
BINGLet’s explore billing and coding guidance in the context of Medicaid healthcare:
BINGLet’s explore billing and coding guidance in the context of Medicaid healthcare:
- Billing and Coding Guidance:
- Medicaid provides resources and guidelines to assist states, providers, and local governments in understanding billing and coding practices.
- These resources cover various aspects, including COVID-19-related services, monoclonal antibody infusion programs, and payment for alternate care sites.
- For specific details, you can refer to the Medicaid Billing and Coding Guidance provided by Medicaid1.
- National Correct Coding Initiative (NCCI) Tools:
- The NCCI tools are essential for correct coding and billing.
- They help prevent improper payment when certain codes should not be reported together.
- You can learn more about using these tools in the Medicaid NCCI Booklet2.
- Importance of Medical Coding and Billing:
- Medical coding translates healthcare services into standardized codes for accurate billing and reimbursement.
- Billing ensures that healthcare providers receive appropriate payment for their services.
- Understanding these processes is crucial for efficient healthcare administration and financial stability.
Partial capitation versus fee-for-service in mental health care
D L Shern, S A Donahue, C Felton, G R Joseph and N Brier
Health Affairs, 14, no.3 (1995):208-219
D L Shern, S A Donahue, C Felton, G R Joseph and N Brier
Health Affairs, 14, no.3 (1995):208-219
What are bundled payments and how can they be used by healthcare organizations?
By Carol Bazell, Maggie Alston, Pamela M. Pelizzari, and Brian A. Sweatman
27 March 2023
https://www.milliman.com/en/insight/what-are-bundled-payments-and-how-can-they-be-used-by-healthcare-organizations
Intro
In healthcare, provider payments are moving away from fee-for-service (FFS) payment and toward value-based models, where an increasing amount of healthcare dollars flow through different types of alternative payment models (APMs) that tie payments to quality and efficiency rather than solely to the volume of services provided. One form of value-based payment is a bundled payment.
This paper is a primer on bundled payments and explores a variety of healthcare industry perspectives on their use.
What is a bundled payment?
A bundled payment is a fixed-price agreement for a predefined episode of care, commonly consisting of a procedure and all related services or all care for a medical condition. In a bundled payment, the responsible entity (commonly a provider) assumes some financial risk for the episode costs that exceed the fixed price. Because payment for an episode of care is not linked to the number and types of services rendered within the episode, a bundled payment incentivizes providers to coordinate care in order to improve efficiency and quality of all included services. Key care management strategies within bundled payments include eliminating services that do not contribute to positive outcomes and increasing the efficiency of services, which includes choosing cost-effective care settings.
Which organizations use bundled payments? And why?
Value-based payment approaches are tailored to a responsible entity’s capabilities and degree of influence over healthcare expenditures. For example, a primary care organization or an integrated delivery system has a high degree of influence over a large proportion of total healthcare expenditures for a set of individuals and, therefore, may be willing to enter into value-based payment agreements for the financial responsibility for the total cost of care of an attributed population (e.g., shared savings models, global capitation, etc.). In contrast, specialty provider organizations have lower degrees of influence over total healthcare expenditures for attributed populations. By focusing on specific procedures or medical conditions and defining an episode of care, bundled payments provide a way for specialty provider organizations to engage in valuebased payment in a manner that is aligned with their influence over healthcare expenditures.
The types of organizations designing and implementing bundled payments are diverse, but they generally share the goals of reducing medically unnecessary variation in care and enhancing the quality of services during a clinically appropriate time period that are related to common highcost procedures and conditions. Below are descriptions of organizations that typically participate in bundled payments.
Bundled payment participation: Organizations transferring financial risk
Centers for Medicare and Medicaid Services (CMS)
CMS is currently testing a variety of bundled payment models for providers caring for Medicare fee-for-service (FFS) beneficiaries. The types of episodes included in CMS’s bundled payment models span surgical procedures and medical care, including oncology. As of early 2023, provider participation in the large majority of CMS models is voluntary rather than mandatory.
Medicare Advantage organizations (MAOs)
MAOs use bundled payments for in-network providers caring for members enrolled in their Medicare Advantage products. A provider’s participation in an MAO’s bundled payment arrangement is typically voluntary. Because of the similarities in the demographics of individuals covered under Medicare FFS and Medicare Advantage, MAOs may use CMS’s episode specifications as a starting point for how their bundled payment arrangements defi ne an episode of care.
Commercial health plans
Commercial health plans use bundled payments for in-network providers caring for members enrolled in their commercial products (e.g., individual and group, fully insured and self-insured). Provider participation in a commercial health plan’s bundled payment arrangement is typically voluntary. The demographics of members enrolled in commercial products differ from those covered by Medicare FFS and Medicare Advantage and, as a result, commercial health plans typically invest the time and resources needed for designing episodes of care relevant to their members (e.g., maternity). Additionally, the degree of variation exhibited in commercial payment rates presents additional challenges and opportunities for both commercial health plans and providers. One such opportunity is modifying member cost sharing to create incentives for members to seek care from providers participating in bundled payment arrangements.
Medicaid organizations
Some state Medicaid agencies have implemented bundled payments for providers caring for Medicaid beneficiaries and/or members enrolled in a plan offered by a Medicaid managed care organization (MCO). For example, Arkansas, Ohio, and Tennessee have each developed programs requiring providers to participate in bundled payments spanning multiple specialty categories, and Colorado has developed a voluntary program focused on maternity episodes. Like commercial health plans, Medicaid organizations may design episodes specific to their covered populations’ characteristics.
Bundled payment participation: Organizations taking financial risk
Provider organizations
Provider organizations can participate in bundled payments designed by payers (CMS, MAOs, commercial health plans, etc.), but some have designed their own bundled payment arrangements for episodes that have been constructed to align with their unique capabilities and clinical pathways. Provider organizations negotiate participation in these bundled payment arrangements with payers (as well as self-insured employer groups via direct contracting).
Conveners
Conveners are third-party organizations (not providers or payers) that generally take on financial liability from payers for the performance of provider participants in bundled payment programs. These organizations typically facilitate coordination among participants, oversee care redesign eff orts to help achieve savings, apportion downside financial risk to participants, and bear some (if not all) of that risk. In exchange, they have the opportunity to receive episode savings payments. They may off er bundled payment network management and provide software tools and reports that enable providers to organize and finance delivery efficiencies. Conveners, common in CMS bundled payment models, can encourage participation in bundled payment models by allowing providers to share financial risk with another entity.
Bundled payment participation: Other organizations shaping uptake
Self-insured employer groups and “point solutions” vendors
Aside from healthcare providers who may develop bundled payment arrangements in which their own self-insured employee health plans are participating and large employers that directly purchase bundled care for their employees through selected providers (e.g., designated centers for lower extremity joint replacement or cardiac surgery episodes), most self-insured employers typically do not design and implement their own bundled payments. They are, however, a driving force in creating demand for value in healthcare purchasing, and their participation in these arrangements can be passive or active. An example of passive participation is when an employer plan’s third-party administrator (TPA) has implemented bundled payments with in-network providers in the TPA’s network in a manner that may not be apparent to the self-insured employer or its members. An example of active participation is an employer engaging with a “point solution” vendor. These arrangements may involve incentives for members (such as reduced cost sharing) to use preferred providers participating in a bundled payment arrangement (although the consumer may not be aware of the underlying financial arrangement).
“Point solution” vendors in this context are organizations that have designed bundled payment programs and have contracted with multiple provider organizations to participate in their networks. They often focus on a particular subpopulation or chronic conditions (e.g., diabetes or obesity). Access to this network is marketed to self-insured employer groups separately from their TPAs’ provider networks.
Workers’ compensation insurers and vendors
The medical portion of workers’ compensation (WC) benefits represents about 50% to 60% of total WC benefits and, consistent with the cost of medical services, continues to trend at rates higher than inflation. While WC insurers can develop networks of provider organizations, they often lack the scale and data to manage these networks as efficiently as health insurers. Additionally, the medical cost of an episode in WC is often significantly higher than the same episode in healthcare. To address this issue, WC insurers and vendors have begun collaborating with healthcare providers to establish benchmark bundled payments for common types of WC episodes (e.g., musculoskeletal injuries). These providers agree to lower prices in exchange for increased volume and the opportunity to be paid for delivering efficient, high-quality care. It’s important to note that, in some states, employers cannot direct care.
What are the considerations for designing and implementing bundled payments?
Bundled payments are complex and require input and ongoing feedback from stakeholders with clinical, actuarial, policy, financial, operational, and technological backgrounds. Key considerations for designing and implementing bundled payments are further described below.
Perspective: Provider-led vs. payer-led?
There are plenty of examples of bundled payment development being led by providers and payers. The type of organization leading the bundled payment eff ort, however, influences the program’s design and operational parameters. Providers leading the eff ort are likely to prioritize creating episode definitions that align with their clinical strengths and capabilities that lead to high-quality, efficient care and optimized health outcomes, whereas payers are likely to prioritize episode definitions with high-volume and financial methodologies intended to both lower the cost of care and improve quality.
Breadth of definition
Defining the scope of episode services is essential for the successful implementation of bundled payments. Identifying the procedures or medical conditions of interest that are the episode focus is typically straightforward and can be based on analysis of claims data to identify the potential episode volume and material variations in the cost of care attributable to the procedure or condition (e.g., the cost of total knee replacement in inpatient versus outpatient settings).
Identifying the services that are considered related to the episode procedures or medical condition (commonly based on claims data alone), as well as the appropriate duration of an episode of care, is typically referred to as creating the episode definition. This is a more subjective exercise requiring a substantial degree of clinical expertise and analytic capability and may be subject to the limitations of relying on claims data (e.g., no clinical information from the medical record, imprecision in provider reporting of diagnosis codes on claims, etc.). Episodes that are narrowly defi ned provide stability and predictability for providers but limit the financial opportunities for both payers and providers related to improving the efficiency of services. Episodes that are more broadly defi ned may provide greater opportunities to improve efficiency and quality but are more likely to result in taking on financial risk for services that are not tightly linked to the episode focus. Organizations should be aware of this trade-off between breadth of definitions and financial incentives.
Another consideration for the breadth of an episode definition is whether prescription drugs are included. Drugs can play an important role in managing episodes of care (particularly for episodes focused on medical conditions), but drug pricing dynamics are complex and thus providers may have difficulty understanding and taking financial responsibility for prescription drugs.
Procedures vs. medical condition focus
Bundled payments for episodes centered on procedures can create incentives for providers to eliminate wasteful services and choose cost-effective care settings for the procedure. These types of episodes are initially appealing to providers, payers, and other interested organizations because the procedure and related services included in the episode definition are generally overseen primarily by the operating specialist, as the scope of episode care is typically closely linked to the procedure itself. However, payers may be concerned that procedural episodes may not provide incentives for providers to most appropriately select patients for procedures or to intensify medical management that may potentially avoid procedures altogether. To address concerns about potential overutilization of elective procedures that may result from the provider opportunities presented by bundled payments, bundled payments for episodes centered on medical conditions for which a procedure is one treatment option among others can help to address this risk. Condition-based episodes typically identify and include services that are
considered beneficial to reducing the need for surgery and directly incentivize lower rates of procedures, which are typically high-cost services that contribute substantially to the episode cost for medical conditions.
Prospective vs. retrospective methodologies
There are two fundamental designs for bundled payments, which have significant implications for price-setting and the role of quality:
1. Prospective, which involves known up-front prices for an episode and concurrent identification of patients eligible for bundled payments.
2. Retrospective, which involves reconciling episode costs against bundled payment price targets for patients who may not be identified as being in an eligible episode until the end of a bundled payment performance period.
Prospective designs have the potential to be more transformative by aligning patient incentives to use participating providers (e.g., by waiving cost sharing), but they are more administratively complex than retrospective designs.
Administrative capabilities
As organizations explore prospective versus retrospective approaches, they should consider whether they have the necessary administrative capabilities, such as:
Accounting for healthcare system changes over time
The healthcare industry is constantly evolving and responding to external forces (e.g., a global pandemic, revised evidence-based clinical guidelines). As a result, value-based payment programs will evolve and change if goals and incentives are to remain appropriately aligned. At the same time, bundled payments, especially those with broad episode definitions, will need to maintain flexibility to address any unintended impacts.
What are the keys to success?
Our experience in supporting organizations in designing and implementing their bundled payments has yielded several elements which we believe are keys to success, including:
Defining and measuring success
The success of bundled payments will likely mean different things to different organizations. Some organizations may prioritize financial results above all else, whereas other organizations may emphasize patient outcomes. Most organizations will want to achieve both objectives. Having a clear framework for defining and measuring success is essential. It helps with:
Using benchmarking
Benchmark data can come from a variety of sources, including government-maintained databases, a payer’s book of business, and proprietary databases constructed by vendors and consultants. By aggregating medical and prescription drug claims and capturing the total cost of care for patients of interest, benchmark data can be used to explore various questions relevant to bundled payments, such as:
Using analytics
Provider organizations continue to invest in their technology and analytics capabilities but often have difficulty with visibility into services their patients receive from unaffiliated providers. They may also struggle with the timeliness of claims data and the lack of usability of claims data to inform individual patient care decisions. Organizations engaged in bundled payments may have a higher chance of success if they can supply participants with analytics that give timely visibility into the following types of information:
Conclusion
As the demand for value in healthcare purchasing continues, the increased interest and use of bundled payments will likely continue. Because they are often viewed as a “middle ground” between the “low risk” of traditional FFS payments and the “high risk” of full capitation, some organizations see bundled payments as a steppingstone toward taking on risk in value-based payment. Bundled payments may provide a feasible approach to specialist engagement in value-based payments, as well as provide an opportunity for other organizations to showcase their unique capabilities and clinical pathways. Carefully considering the design and implementation elements in combination with the keys to success described above is important for all organizations participating in bundled payments.
By Carol Bazell, Maggie Alston, Pamela M. Pelizzari, and Brian A. Sweatman
27 March 2023
https://www.milliman.com/en/insight/what-are-bundled-payments-and-how-can-they-be-used-by-healthcare-organizations
Intro
In healthcare, provider payments are moving away from fee-for-service (FFS) payment and toward value-based models, where an increasing amount of healthcare dollars flow through different types of alternative payment models (APMs) that tie payments to quality and efficiency rather than solely to the volume of services provided. One form of value-based payment is a bundled payment.
This paper is a primer on bundled payments and explores a variety of healthcare industry perspectives on their use.
What is a bundled payment?
A bundled payment is a fixed-price agreement for a predefined episode of care, commonly consisting of a procedure and all related services or all care for a medical condition. In a bundled payment, the responsible entity (commonly a provider) assumes some financial risk for the episode costs that exceed the fixed price. Because payment for an episode of care is not linked to the number and types of services rendered within the episode, a bundled payment incentivizes providers to coordinate care in order to improve efficiency and quality of all included services. Key care management strategies within bundled payments include eliminating services that do not contribute to positive outcomes and increasing the efficiency of services, which includes choosing cost-effective care settings.
Which organizations use bundled payments? And why?
Value-based payment approaches are tailored to a responsible entity’s capabilities and degree of influence over healthcare expenditures. For example, a primary care organization or an integrated delivery system has a high degree of influence over a large proportion of total healthcare expenditures for a set of individuals and, therefore, may be willing to enter into value-based payment agreements for the financial responsibility for the total cost of care of an attributed population (e.g., shared savings models, global capitation, etc.). In contrast, specialty provider organizations have lower degrees of influence over total healthcare expenditures for attributed populations. By focusing on specific procedures or medical conditions and defining an episode of care, bundled payments provide a way for specialty provider organizations to engage in valuebased payment in a manner that is aligned with their influence over healthcare expenditures.
The types of organizations designing and implementing bundled payments are diverse, but they generally share the goals of reducing medically unnecessary variation in care and enhancing the quality of services during a clinically appropriate time period that are related to common highcost procedures and conditions. Below are descriptions of organizations that typically participate in bundled payments.
Bundled payment participation: Organizations transferring financial risk
Centers for Medicare and Medicaid Services (CMS)
CMS is currently testing a variety of bundled payment models for providers caring for Medicare fee-for-service (FFS) beneficiaries. The types of episodes included in CMS’s bundled payment models span surgical procedures and medical care, including oncology. As of early 2023, provider participation in the large majority of CMS models is voluntary rather than mandatory.
Medicare Advantage organizations (MAOs)
MAOs use bundled payments for in-network providers caring for members enrolled in their Medicare Advantage products. A provider’s participation in an MAO’s bundled payment arrangement is typically voluntary. Because of the similarities in the demographics of individuals covered under Medicare FFS and Medicare Advantage, MAOs may use CMS’s episode specifications as a starting point for how their bundled payment arrangements defi ne an episode of care.
Commercial health plans
Commercial health plans use bundled payments for in-network providers caring for members enrolled in their commercial products (e.g., individual and group, fully insured and self-insured). Provider participation in a commercial health plan’s bundled payment arrangement is typically voluntary. The demographics of members enrolled in commercial products differ from those covered by Medicare FFS and Medicare Advantage and, as a result, commercial health plans typically invest the time and resources needed for designing episodes of care relevant to their members (e.g., maternity). Additionally, the degree of variation exhibited in commercial payment rates presents additional challenges and opportunities for both commercial health plans and providers. One such opportunity is modifying member cost sharing to create incentives for members to seek care from providers participating in bundled payment arrangements.
Medicaid organizations
Some state Medicaid agencies have implemented bundled payments for providers caring for Medicaid beneficiaries and/or members enrolled in a plan offered by a Medicaid managed care organization (MCO). For example, Arkansas, Ohio, and Tennessee have each developed programs requiring providers to participate in bundled payments spanning multiple specialty categories, and Colorado has developed a voluntary program focused on maternity episodes. Like commercial health plans, Medicaid organizations may design episodes specific to their covered populations’ characteristics.
Bundled payment participation: Organizations taking financial risk
Provider organizations
Provider organizations can participate in bundled payments designed by payers (CMS, MAOs, commercial health plans, etc.), but some have designed their own bundled payment arrangements for episodes that have been constructed to align with their unique capabilities and clinical pathways. Provider organizations negotiate participation in these bundled payment arrangements with payers (as well as self-insured employer groups via direct contracting).
Conveners
Conveners are third-party organizations (not providers or payers) that generally take on financial liability from payers for the performance of provider participants in bundled payment programs. These organizations typically facilitate coordination among participants, oversee care redesign eff orts to help achieve savings, apportion downside financial risk to participants, and bear some (if not all) of that risk. In exchange, they have the opportunity to receive episode savings payments. They may off er bundled payment network management and provide software tools and reports that enable providers to organize and finance delivery efficiencies. Conveners, common in CMS bundled payment models, can encourage participation in bundled payment models by allowing providers to share financial risk with another entity.
Bundled payment participation: Other organizations shaping uptake
Self-insured employer groups and “point solutions” vendors
Aside from healthcare providers who may develop bundled payment arrangements in which their own self-insured employee health plans are participating and large employers that directly purchase bundled care for their employees through selected providers (e.g., designated centers for lower extremity joint replacement or cardiac surgery episodes), most self-insured employers typically do not design and implement their own bundled payments. They are, however, a driving force in creating demand for value in healthcare purchasing, and their participation in these arrangements can be passive or active. An example of passive participation is when an employer plan’s third-party administrator (TPA) has implemented bundled payments with in-network providers in the TPA’s network in a manner that may not be apparent to the self-insured employer or its members. An example of active participation is an employer engaging with a “point solution” vendor. These arrangements may involve incentives for members (such as reduced cost sharing) to use preferred providers participating in a bundled payment arrangement (although the consumer may not be aware of the underlying financial arrangement).
“Point solution” vendors in this context are organizations that have designed bundled payment programs and have contracted with multiple provider organizations to participate in their networks. They often focus on a particular subpopulation or chronic conditions (e.g., diabetes or obesity). Access to this network is marketed to self-insured employer groups separately from their TPAs’ provider networks.
Workers’ compensation insurers and vendors
The medical portion of workers’ compensation (WC) benefits represents about 50% to 60% of total WC benefits and, consistent with the cost of medical services, continues to trend at rates higher than inflation. While WC insurers can develop networks of provider organizations, they often lack the scale and data to manage these networks as efficiently as health insurers. Additionally, the medical cost of an episode in WC is often significantly higher than the same episode in healthcare. To address this issue, WC insurers and vendors have begun collaborating with healthcare providers to establish benchmark bundled payments for common types of WC episodes (e.g., musculoskeletal injuries). These providers agree to lower prices in exchange for increased volume and the opportunity to be paid for delivering efficient, high-quality care. It’s important to note that, in some states, employers cannot direct care.
What are the considerations for designing and implementing bundled payments?
Bundled payments are complex and require input and ongoing feedback from stakeholders with clinical, actuarial, policy, financial, operational, and technological backgrounds. Key considerations for designing and implementing bundled payments are further described below.
Perspective: Provider-led vs. payer-led?
There are plenty of examples of bundled payment development being led by providers and payers. The type of organization leading the bundled payment eff ort, however, influences the program’s design and operational parameters. Providers leading the eff ort are likely to prioritize creating episode definitions that align with their clinical strengths and capabilities that lead to high-quality, efficient care and optimized health outcomes, whereas payers are likely to prioritize episode definitions with high-volume and financial methodologies intended to both lower the cost of care and improve quality.
Breadth of definition
Defining the scope of episode services is essential for the successful implementation of bundled payments. Identifying the procedures or medical conditions of interest that are the episode focus is typically straightforward and can be based on analysis of claims data to identify the potential episode volume and material variations in the cost of care attributable to the procedure or condition (e.g., the cost of total knee replacement in inpatient versus outpatient settings).
Identifying the services that are considered related to the episode procedures or medical condition (commonly based on claims data alone), as well as the appropriate duration of an episode of care, is typically referred to as creating the episode definition. This is a more subjective exercise requiring a substantial degree of clinical expertise and analytic capability and may be subject to the limitations of relying on claims data (e.g., no clinical information from the medical record, imprecision in provider reporting of diagnosis codes on claims, etc.). Episodes that are narrowly defi ned provide stability and predictability for providers but limit the financial opportunities for both payers and providers related to improving the efficiency of services. Episodes that are more broadly defi ned may provide greater opportunities to improve efficiency and quality but are more likely to result in taking on financial risk for services that are not tightly linked to the episode focus. Organizations should be aware of this trade-off between breadth of definitions and financial incentives.
Another consideration for the breadth of an episode definition is whether prescription drugs are included. Drugs can play an important role in managing episodes of care (particularly for episodes focused on medical conditions), but drug pricing dynamics are complex and thus providers may have difficulty understanding and taking financial responsibility for prescription drugs.
Procedures vs. medical condition focus
Bundled payments for episodes centered on procedures can create incentives for providers to eliminate wasteful services and choose cost-effective care settings for the procedure. These types of episodes are initially appealing to providers, payers, and other interested organizations because the procedure and related services included in the episode definition are generally overseen primarily by the operating specialist, as the scope of episode care is typically closely linked to the procedure itself. However, payers may be concerned that procedural episodes may not provide incentives for providers to most appropriately select patients for procedures or to intensify medical management that may potentially avoid procedures altogether. To address concerns about potential overutilization of elective procedures that may result from the provider opportunities presented by bundled payments, bundled payments for episodes centered on medical conditions for which a procedure is one treatment option among others can help to address this risk. Condition-based episodes typically identify and include services that are
considered beneficial to reducing the need for surgery and directly incentivize lower rates of procedures, which are typically high-cost services that contribute substantially to the episode cost for medical conditions.
Prospective vs. retrospective methodologies
There are two fundamental designs for bundled payments, which have significant implications for price-setting and the role of quality:
1. Prospective, which involves known up-front prices for an episode and concurrent identification of patients eligible for bundled payments.
2. Retrospective, which involves reconciling episode costs against bundled payment price targets for patients who may not be identified as being in an eligible episode until the end of a bundled payment performance period.
Prospective designs have the potential to be more transformative by aligning patient incentives to use participating providers (e.g., by waiving cost sharing), but they are more administratively complex than retrospective designs.
Administrative capabilities
As organizations explore prospective versus retrospective approaches, they should consider whether they have the necessary administrative capabilities, such as:
- Claims processing: Retrospective approaches may continue to rely on traditional FFS payments with periodic transfers of savings and losses, whereas prospective approaches may require substantial overhauls to claims adjudication processes, which could have significant downstream implications on other processes that rely on adjudicated claims (e.g., pricing and contracting).
- Reconciliation: Both retrospective and prospective approaches may require periodic evaluation to determine providers’ financial and quality performance and to settle savings and losses between the payer and the provider.
- Maintenance of episode definitions: The claims-based codes (diagnosis, procedure, revenue, etc.) underlying an episode definition will change over time for a multitude of reasons, including the creation and deletion of codes by the code maintainers that occurs multiple times during a year and stakeholder feedback about episode definitions.
Accounting for healthcare system changes over time
The healthcare industry is constantly evolving and responding to external forces (e.g., a global pandemic, revised evidence-based clinical guidelines). As a result, value-based payment programs will evolve and change if goals and incentives are to remain appropriately aligned. At the same time, bundled payments, especially those with broad episode definitions, will need to maintain flexibility to address any unintended impacts.
What are the keys to success?
Our experience in supporting organizations in designing and implementing their bundled payments has yielded several elements which we believe are keys to success, including:
- Defining and measuring success
- Using benchmarking to support bundle selection and design
- Using analytics for monitoring and management
Defining and measuring success
The success of bundled payments will likely mean different things to different organizations. Some organizations may prioritize financial results above all else, whereas other organizations may emphasize patient outcomes. Most organizations will want to achieve both objectives. Having a clear framework for defining and measuring success is essential. It helps with:
- Articulating an organization’s value proposition
- Creating discipline to guide ongoing decision-making
- Garnering ongoing organizational support
Using benchmarking
Benchmark data can come from a variety of sources, including government-maintained databases, a payer’s book of business, and proprietary databases constructed by vendors and consultants. By aggregating medical and prescription drug claims and capturing the total cost of care for patients of interest, benchmark data can be used to explore various questions relevant to bundled payments, such as:
- How common are certain procedures or medical conditions?
- What sites of service have been used to perform procedures and/or treat medical conditions?
- What services are most commonly happening in proximity to a procedure or diagnosis of a medical condition? Do these services appear to be related to the procedure or medical condition?
- If an episode of care is constructed around a procedure or medical condition, how much variation in cost exists? Are there clear opportunities to increase the efficiency of services, e.g., eliminate wasteful services, substitute less costly services, or change sites of service?
- How does a prospectively determined bundled payment price compare to a status quo FFS amount?
Using analytics
Provider organizations continue to invest in their technology and analytics capabilities but often have difficulty with visibility into services their patients receive from unaffiliated providers. They may also struggle with the timeliness of claims data and the lack of usability of claims data to inform individual patient care decisions. Organizations engaged in bundled payments may have a higher chance of success if they can supply participants with analytics that give timely visibility into the following types of information:
- Episode characteristics: Volume and costs (for historical and performance periods), site of service, codes triggering the episode, quality metrics (e.g., complications).
- Patient characteristics: Age, diagnosis codes, indicators of socioeconomic status (e.g., eligibility for Medicaid).
- Financial information: Bundled payment price targets, risk adjustment factors, outlier exclusions, reconciliation detail.
Conclusion
As the demand for value in healthcare purchasing continues, the increased interest and use of bundled payments will likely continue. Because they are often viewed as a “middle ground” between the “low risk” of traditional FFS payments and the “high risk” of full capitation, some organizations see bundled payments as a steppingstone toward taking on risk in value-based payment. Bundled payments may provide a feasible approach to specialist engagement in value-based payments, as well as provide an opportunity for other organizations to showcase their unique capabilities and clinical pathways. Carefully considering the design and implementation elements in combination with the keys to success described above is important for all organizations participating in bundled payments.
Reform model not yet helping people with mental illness
Coordinated care gains not reaching patients with mental health diagnoses
By JAKE MILLER December 7, 2015
https://medicalxpress.com/news/2015-12-reform-people-mental-illness.html
People diagnosed with mental health conditions did not see improvements in coordination and quality of their care, as some had hoped, but they also did not experience large cuts in access, as some had feared. Those were some of the findings of a team of researchers from Harvard Medical School and Johns Hopkins Bloomberg School of Public Health who studied an early alternative payment model designed to encourage coordinated health care.
The research team looked at claims data from 2006-2011 to examine whether the implementation of the Blue Cross Blue Shield of Massachusetts Alternative Quality Contract affected mental health service use, mental health care spending, total spending and quality of care.
They also interviewed providers and managers about the process of implementing the AQC and the potential for developing systems to improve coordination of care for people with mental health diagnoses.
The researchers said the interviews suggest that these organizations were not focused on mental health integration when the contract was first implemented but are now thinking creatively and innovatively about developing new programs. Some involve integrating social workers into treatment teams focused on non-mental health conditions, like diabetes, to better identify and support patients with mental health conditions who would benefit from more integration of mental health and medical care. They said it is too early to have seen results from these new programs.
“The initial effort didn't solve the problem of fragmented care for people with mental health conditions,” Huskamp said. “We still need to do more to integrate the care that they get.”The study was led by Haiden Huskamp, professor of health care policy in the Department of Health Care Policy at Harvard Medical School, and Colleen Barry, professor and associate chair for research and practice in the Department of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health. The findings are published in the December issue of Health Affairs.
“The initial effort didn't solve the problem of fragmented care for people with mental health conditions,” Huskamp said. “We still need to do more to integrate the care that they get.”
Payment reform experiments
While the traditional fee-for-service model provides a financial incentive for providers to perform more procedures, new payment models that provide a lump sum to cover all the costs of a person’s care can motivate physicians and hospital administrators to focus on providing the highest value care and improving care coordination, although the new models could also result in reduced access to care.
Various organizational approaches to this goal—accountable care organizations, bundled payments, global budgets—are part of many public and private health care reform efforts. One early example is the Blue Cross Blue Shield of Massachusetts Alternative Quality Contract, which began in 2009.
An earlier study of the AQC found that for the general population, the growth of overall health care spending slowed and some measures of quality of care improved.
Huskamp, Barry and colleagues at HMS, Johns Hopkins and McLean Hospital wanted to know whether the model had the same effects on people who receive mental health care.
This is a crucial population for health care reform. Mental health disorders affect tens of millions of people in the United States each year, and the total direct and indirect costs of the most serious mental health illness are more than $300 billion per year, according to the National Institute of Mental Health.
Integrating fragmented care
Since care for mental health is even more fragmented than care in the rest of the health care system—with distinct insurance benefits for mental and behavioral health, and a separate mental health care system that is often not directly linked to primary or secondary medical care services—the researchers noted that it is an area that could benefit greatly from efforts to improve the quality and coordination of care.
Instead, they found that some AQC patients with a mental health diagnosis were slightly less likely to receive mental health services than a comparable group covered by the same insurer. They also found that for people who did use mental health services, spending did not change.
In addition, people with mental health diagnoses were less likely to benefit from improvements in quality of care.
For example, to help prevent and treat chronic illnesses, the AQC offers incentives for clinicians to increase the use of diabetes management approaches. Providers working under the AQC were more likely to adopt certain diabetes management approaches for patients in the AQC than for a comparison group of Blue Cross Blue Shield enrollees not in the AQC, but these improvements were not found among the subgroup of AQC enrollees with both diabetes and a co-occurring mental health diagnosis.
According to the researchers, as accountable care evolves, policymakers, insurance companies and providers will need to understand how these reforms affect care for often high-cost individuals with mental health treatment needs.
“In order to take advantage of the transformative power of coordinated care,” Barry said, “we need to make sure that the incentives and quality measures we use address the needs of this crucial population.”
Evolution Ongoing
In addition to their quantitative analysis, the researchers also conducted interviews with providers and managers in a variety of organizations to understand the context for the complex transformations taking place.
Interview participants said that many organizations spent the first years of the contract building the basic infrastructure for collecting the data necessary to coordinate care and measure progress, and that their organizations have only recently begun to address some of the more challenging changes needed to manage mental health care delivery.
“They now have to think about the whole person, and that's changing how they do business,” Huskamp said.
The study was funded by Commonwealth Fund grant number 20130499.
Co-author Robert Mechanic is a trustee at Atrius Health, one of the provider organizations that signed the Alternative Quality Contract with Blue Cross Blue Shield of Massachusetts (BCBSMA).
Coordinated care gains not reaching patients with mental health diagnoses
By JAKE MILLER December 7, 2015
https://medicalxpress.com/news/2015-12-reform-people-mental-illness.html
People diagnosed with mental health conditions did not see improvements in coordination and quality of their care, as some had hoped, but they also did not experience large cuts in access, as some had feared. Those were some of the findings of a team of researchers from Harvard Medical School and Johns Hopkins Bloomberg School of Public Health who studied an early alternative payment model designed to encourage coordinated health care.
The research team looked at claims data from 2006-2011 to examine whether the implementation of the Blue Cross Blue Shield of Massachusetts Alternative Quality Contract affected mental health service use, mental health care spending, total spending and quality of care.
They also interviewed providers and managers about the process of implementing the AQC and the potential for developing systems to improve coordination of care for people with mental health diagnoses.
The researchers said the interviews suggest that these organizations were not focused on mental health integration when the contract was first implemented but are now thinking creatively and innovatively about developing new programs. Some involve integrating social workers into treatment teams focused on non-mental health conditions, like diabetes, to better identify and support patients with mental health conditions who would benefit from more integration of mental health and medical care. They said it is too early to have seen results from these new programs.
“The initial effort didn't solve the problem of fragmented care for people with mental health conditions,” Huskamp said. “We still need to do more to integrate the care that they get.”The study was led by Haiden Huskamp, professor of health care policy in the Department of Health Care Policy at Harvard Medical School, and Colleen Barry, professor and associate chair for research and practice in the Department of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health. The findings are published in the December issue of Health Affairs.
“The initial effort didn't solve the problem of fragmented care for people with mental health conditions,” Huskamp said. “We still need to do more to integrate the care that they get.”
Payment reform experiments
While the traditional fee-for-service model provides a financial incentive for providers to perform more procedures, new payment models that provide a lump sum to cover all the costs of a person’s care can motivate physicians and hospital administrators to focus on providing the highest value care and improving care coordination, although the new models could also result in reduced access to care.
Various organizational approaches to this goal—accountable care organizations, bundled payments, global budgets—are part of many public and private health care reform efforts. One early example is the Blue Cross Blue Shield of Massachusetts Alternative Quality Contract, which began in 2009.
An earlier study of the AQC found that for the general population, the growth of overall health care spending slowed and some measures of quality of care improved.
Huskamp, Barry and colleagues at HMS, Johns Hopkins and McLean Hospital wanted to know whether the model had the same effects on people who receive mental health care.
This is a crucial population for health care reform. Mental health disorders affect tens of millions of people in the United States each year, and the total direct and indirect costs of the most serious mental health illness are more than $300 billion per year, according to the National Institute of Mental Health.
Integrating fragmented care
Since care for mental health is even more fragmented than care in the rest of the health care system—with distinct insurance benefits for mental and behavioral health, and a separate mental health care system that is often not directly linked to primary or secondary medical care services—the researchers noted that it is an area that could benefit greatly from efforts to improve the quality and coordination of care.
Instead, they found that some AQC patients with a mental health diagnosis were slightly less likely to receive mental health services than a comparable group covered by the same insurer. They also found that for people who did use mental health services, spending did not change.
In addition, people with mental health diagnoses were less likely to benefit from improvements in quality of care.
For example, to help prevent and treat chronic illnesses, the AQC offers incentives for clinicians to increase the use of diabetes management approaches. Providers working under the AQC were more likely to adopt certain diabetes management approaches for patients in the AQC than for a comparison group of Blue Cross Blue Shield enrollees not in the AQC, but these improvements were not found among the subgroup of AQC enrollees with both diabetes and a co-occurring mental health diagnosis.
According to the researchers, as accountable care evolves, policymakers, insurance companies and providers will need to understand how these reforms affect care for often high-cost individuals with mental health treatment needs.
“In order to take advantage of the transformative power of coordinated care,” Barry said, “we need to make sure that the incentives and quality measures we use address the needs of this crucial population.”
Evolution Ongoing
In addition to their quantitative analysis, the researchers also conducted interviews with providers and managers in a variety of organizations to understand the context for the complex transformations taking place.
Interview participants said that many organizations spent the first years of the contract building the basic infrastructure for collecting the data necessary to coordinate care and measure progress, and that their organizations have only recently begun to address some of the more challenging changes needed to manage mental health care delivery.
“They now have to think about the whole person, and that's changing how they do business,” Huskamp said.
The study was funded by Commonwealth Fund grant number 20130499.
Co-author Robert Mechanic is a trustee at Atrius Health, one of the provider organizations that signed the Alternative Quality Contract with Blue Cross Blue Shield of Massachusetts (BCBSMA).
The Case for Capitation
It’s the only way to cut waste while improving quality. by Brent C. James, MD and Gregory P. Poulsen
From the Magazine (July–August 2016)
Harvard Business Review
Summary. Recent studies suggest that at least 35%—and maybe over 50%—of all health care spending in the U.S. is wasted on inadequate, unnecessary, and inefficient care and suboptimal business processes. But efforts to get rid of that waste face a huge challenge.
To rein in health care costs in the United States, we should look to the ideas of W. Edwards Deming, the legendary management guru who showed companies how to cut waste from work processes and lower operating costs by improving quality. Recent studies using Deming’s approach reveal that inadequate, unnecessary, uncoordinated, and inefficient care and suboptimal business processes eat up at least 35%—and maybe over 50%—of the more than $3 trillion that the country spends annually on health care. That suggests more than $1 trillion is being squandered.
Ongoing reform efforts by the federal government and private insurers have had some success in prodding health care providers to improve quality and reduce waste. But it’s far from certain that they’ll be enough. Even after taking existing and proposed reform initiatives into account, federal projections show health care expenditures consuming larger and larger proportions of the GDP. Moreover, under the prevailing payment models, which are based on volume of services, providers often don’t receive any of the savings from waste reduction, which undermines both their financial health and their ability to continue to invest in such efforts.
The solution to this quandary is to change the way businesses, government, and other purchasers pay for health care to population-based payment. Under this approach, providers receive a fixed per person (or “capitated”) payment that covers all health care services over a defined time period, adjusted for each patient’s expected needs, and are also held accountable for high-quality outcomes. It’s the only payment system that fully aligns providers’ financial incentives with the goal of eliminating all major categories of waste. It fundamentally shifts the role of managing the amount, form, and cost of care from insurers to medical practitioners. It also ensures that providers receive enough of the savings that they can afford to fund the changes needed to bring down costs.
A population-based payment model also has major implications for pure health insurers: Because it removes care oversight from their purview, it leaves them only traditional insurance functions such as claims processing, risk analysis, reinsurance, marketing, and customer service. Many nonprofit health insurers competently provide a full range of such services for less than 10% of total health insurance payments, well below the portion that many health insurers now extract through current systems.
In this article we’ll look at the different categories of waste in health care and then outline the various payment methods that have evolved in the United States and their effect on waste. We’ll then demonstrate how population-based payment, backed by good reporting, can improve clinical results, eliminate unnecessary spending, and lower costs.
Three Kinds of WasteIn health care there are three basic categories of waste: production-level waste, case-level waste, and population-level waste.
Half of all waste in care delivery is unnecessary or suboptimal care.
The first category involves inefficiencies in producing “units of care”—drugs, lab tests, x-rays, hours of nursing support, and any other item consumed in patient treatment. It accounts for about 5% of total health care waste. Eliminating it requires things like negotiating down prices for supplies, lowering handling and storage costs, streamlining processes for producing lab tests or x-rays, and reducing losses due to damage, misplacement, or expiration.
The second category, which comprises about half of all waste in care delivery, is unnecessary or suboptimal use of care during a hospital stay, an outpatient visit, or some other treatment episode, or “case.” Examples include redundant x-rays ordered when the original images couldn’t be found, duplicate lab tests ordered because a physician didn’t know that someone else had already done the tests, and medications prescribed to treat avoidable complications.
The third category, which accounts for about 45% of total waste, involves cases within a patient population that are unnecessary or preventable. It includes end-of-life intensive care given to people who’ve expressly asked not to receive it; elective surgical procedures that, with better information, patients would have forgone; and visits to specialists or hospitalizations that could have been avoided through timely, cheaper outpatient care. Waste here obviously feeds waste at the other two levels, since each unnecessary or avoidable case consumes care.
The Impact of Different Payment ModelsTo understand what’s driving up health care spending, it’s critical to examine whether—and to what extent—health care payment methods encourage or discourage waste reduction. An optimal payment method must address two important challenges. One is how to divvy up the savings generated by eliminating waste. If most or all of the money goes to health care payers, providers have no incentive to cut waste. If most or all of it goes to providers, how do you ensure that they pass on some of it to customers—especially if there is no efficient market, which, we’d argue, you often can’t create in health care because of its complexities? Another issue is how a payment method affects the power of patients and their physicians to make decisions that are in patients’ best interests. Let’s look at the methods that have evolved in the United States over the years and see how each stacks up.
Cost-plus.In 1965, as part of the War on Poverty, the U.S. Congress enacted the Medicare and Medicaid government-funded health insurance programs. Those programs paid physicians and hospitals on a cost-plus basis. Care providers estimated their cost for delivering each unit of care, and then the government paid that cost plus a markup. The result was that providers could basically consume whatever resources they wanted—and had no incentive to reduce spending. Today cost-plus payment persists only in small pockets of health care, such as some specialty hospitals and some small rural hospitals.
Fee for service.
Until the 1980s there was little standardization in the way hospitals and physicians billed payers for individual units of care such as lab tests, supplies, or medical services. Then, in a bid to control costs, Medicare began to organize some of the fee categories, and a degree of standardization emerged for the prices and nomenclature of most items, for commercial as well as government payers.
Under the fee-for-service payment method, a provider supplies an approved billing code for (and may be required to justify) each unit of care consumed during a hospitalization, same-day procedure, or outpatient visit. It cannot bill for anything that lacks a code. For each billed item the government pays the lesser of the group’s actual billed charges or a federal maximum allowed rate. (The method it uses to calculate that rate isn’t strongly linked to true underlying costs and is controversial.) As a result, care delivery groups try to ensure that their billed charges are above the federal rates. Given that the rates change constantly as the government updates its estimates, the easiest way for a group to guarantee maximum payment is to set high prices for everything.
Fee for service also encourages care deliverers to provide as much care as possible, regardless of whether it’s all necessary or optimal. Because of that, the types and volume of care used to treat a given disease vary widely, making it difficult to compare the true cost of care across providers. As a result, commercial insurers often base purchasing decisions on percentage discounts they’ve negotiated with care delivery groups. That in turn leads some groups to apply very high markups—so that they can offer large discounts to the insurers.
Fee for service neither effectively promotes the elimination of all kinds of waste nor allocates savings among providers, payers, and patients in a way that would fuel continual improvements. Despite its widely acknowledged deficiencies, it remains the most common payment method in the United States. It forms the basis for nearly all accounting systems used by care delivery groups and health care insurers.
Per case.
This payment method dates back to 1983, when the federal government introduced the “diagnosis-related group” (DRG) system for Medicare patients. Again, the primary purpose was cost control. Currently, DRGs classify hospital and same-day surgery patients into 753 unique categories, on the basis of each patient’s primary disease, specific treatment, secondary chronic conditions, and care intensity. For example, DRG 7 is a lung transplant, DRG 179 uncomplicated pneumonia, and DRG 343 a simple appendectomy. Medicare pays facilities, such as hospitals or surgery centers, a flat rate per case in each category. Meanwhile, it pays physicians involved in the same cases on a fee-for-service basis. Commercial insurers sometimes pay hospitals and surgery centers per case but pay the physicians providing treatment via fee for service.
In 2016 the government introduced “bundled” per case payments in its Medicare program, following an approach first tried by a handful of commercial health insurers. The initial federal experiment focuses on total hip- and total knee-joint-replacement surgery. It extends the single flat-rate DRG payment to include all physician fees and all costs of any related treatments, complications, or hospital readmissions within 90 days of the original operation. If the experiment successfully reduces costs, the government plans to extend it to other types of cases.
Per case payment gives providers incentives to improve efficiency within cases but, like fee for service, is a volume-based system that fuels waste. The more cases a care delivery group handles, the more it gets paid. Therefore, it’s in the group’s financial interest to maximize the number of cases it treats, even if some add no value or actively harm patients.
Capitation.
In contrast to fee-for-service and per case payment methods, per person payment methods can encourage waste reduction at all three levels and give patients and physicians the freedom to make the treatment decisions they think are best. But to function well, such systems must adjust payments for risk, which is easier to do at the level of a population than of an individual patient. (A typical population is a business’s employees and their dependents.) There have to be quality measures to ensure that providers don’t withhold necessary care. And finally, savings from waste reduction must go back to care delivery groups to keep them financially viable.
The last widespread use of capitation in the U.S. didn’t meet the last two criteria. In the late 1980s and into the 1990s, both government and private payers looked for ways to reduce health care inflation. The primary mechanism they turned to was health maintenance organizations (HMOs), which were usually owned and managed by insurance companies. While employers generally paid HMOs on a capitated basis, most HMOs continued to pay care delivery groups using fee-for-service and per case methods.
HMOs employed a series of tools to limit health care consumption. For example, many mandated that primary care physicians act as gatekeepers. Care providers had to get permission from nurses and doctors based at insurance companies to make referrals to specialists and order surgical procedures, imaging, and hospitalizations. In some instances the HMOs passed along a portion of the capitated insurance payment to the provider groups to cover all necessary services, which transferred the financial risk to them.
HMOs succeeded in curbing expenditures. Health care costs as a proportion of GDP remained flat from 1993 through 2000—even though one reason was that the GDP was growing rapidly, hiding the price increases that did occur. However, the insurance companies weren’t in the best position to make health care decisions, because they were removed from patient-clinician interactions. The HMOs’ bureaucratic controls imposed hassles and treatment delays. Some physician groups, unable to manage care costs after accepting capitated payments, failed financially. Patients and physicians rebelled, arguing that the financial incentives built into capitated payments led HMOs to ration care and accusing insurance companies of putting profits before patients’ health. The resulting political backlash ended insurance-company-based cost control as a national movement.
A Better Capitation Model
A population-based payment system would differ from the capitated method most insurance companies use in significant ways. With PBP, care provider organizations would receive a risk-adjusted monthly payment that covers all necessary health services for each person. Eliminating the gatekeeper and the third-party authorization for care that made HMOs so unpopular, PBP would put responsibility for considering the cost of treatment options in the hands of physicians as they consult with patients. Finally, unlike HMOs of the 1990s, PBP would include quality measures and standards. A care delivery group would pay independent physicians using existing fee-for-service mechanisms but would adjust payments quarterly according to the levels of clinical quality and patient satisfaction achieved as well as total cost to care for the covered population. The advantage of this approach is that it would build on a system physicians already understand while rewarding them for improvements in quality and cost, which would compensate them for income lost if total care volumes decline as a result of waste elimination.
Federal cost control efforts mandated by the Affordable Care Act of 2010 are pushing health care payments in this direction. Recognizing that volume-based payments fuel expenditures, increase waste, and potentially worsen quality, government officials are moving toward “pay for value” systems, which give providers financial incentives to hold costs down by improving clinical outcomes and patient satisfaction. To do this, they’re implementing the initiatives below—each of which represents a step along the spectrum toward full capitated payment:
We recommend that, where possible, care providers jump directly to population-based payment and that payers actively support them in that move. Of the pay-for-value methods just listed, it’s the only one that gives care delivery groups the financial incentives to attack all three levels of waste. More specifically, it’s the only one that ensures that care delivery groups capture enough of the savings from waste elimination that they stay financially viable and can continue to invest in such programs. Let us explain.
To raise quality and eliminate waste in health care, we need to do more than end production inefficiencies and unnecessary or inappropriate treatments. Care providers also have to develop, test, and repeatedly improve new care delivery processes—and that requires investment. A major problem with fee-for-service and per case payments is that they redirect the savings away from those who must make the investment and into the pockets of insurance companies. Consider these two examples:
Congestive heart failure and ischemic heart disease (compromised blood flow to the heart) are very common conditions, especially among Medicare patients. Certain medications (beta blockers and ACE and ARB inhibitors), taken every day, can stabilize patients’ conditions and prevent death. The key is recognizing which people need the medications and getting them started on them.
Nationwide, hospitals prescribe the right long-term medications for these two conditions to their patients only 44% of the time. Intermountain Healthcare’s LDS Hospital in Salt Lake City developed a system that boosted its accuracy rate from 57% to over 98%. As a result, mortality fell by more than 450 deaths a year, and hospitalizations by almost 900 cases a year. The majority of those cases were paid through Medicare, on the per case DRG system. The lower hospitalization rate meant that LDS Hospital lost $3.2 million a year in revenues, along with associated operating income. From a purely financial viewpoint, its investment in improving patient outcomes and lowering costs worked out very poorly indeed.
When Intermountain rolled out a better lung treatment for babies, it lost $5 million.
Intermountain’s American Fork Hospital had a large birthing service. About 110 of its newborns each year were borderline premature—with a 34- to 37-week gestation versus the normal 40 weeks. Often the lungs of premature babies are not fully developed, which means they can collapse. In the distant past, most of these “blue babies” died. Then clinicians learned to place a breathing tube through an infant’s mouth into its major airway and use a mechanical ventilator to keep the lungs inflated for a few weeks. This gave infants’ lungs time to mature, and mortality rates plummeted. Unfortunately, intubation and mechanical ventilation are highly invasive, and some babies suffered significant complications.
A group of obstetricians and neonatologists at American Fork Hospital argued that since borderline preemies have lungs that are almost mature, a milder intervention, “nasal continuous positive airway pressure,” which involves blowing pressurized air through the newborn’s nose, might work. In a clinical trial, intubation rates fell from 78% to 18%. The children stayed in the nursery, not the far more expensive newborn ICU. With the simpler, less invasive care, the hospital’s total operating costs for these children fell by $544,000 a year. But fee-for-service insurance payments dropped by $873,000, causing a $329,000 dip in the hospital’s operating income. The hospital also had to bear the costs of developing and implementing the change. Moreover, when Intermountain decided to deploy the new methods across all its hospitals—clearly the right thing to do for the children—that $329,000 turned into more than $5 million in annual losses.
These examples raise critical questions: Should care delivery groups invest in quality improvements that reduce costs if it could mean their own financial demise? Even if a group does so because it’s the right thing for patients, where will it find the resources to launch its next waste reduction project? Shouldn’t the windfall that health insurers receive from waste reduction help fund further improvements? If sharing in the savings strengthened the care delivery group financially, wouldn’t it become a more effective competitor, encouraging other groups to adopt the same cost-saving strategies?
We believe that population-based payment addresses these issues, because it encourages providers to attack all waste, by ensuring that they benefit from the savings. Because per case systems, including the new bundled payment approaches, don’t offer the right financial incentives, close to half of all waste reduction opportunities are likely to go unrealized under them. Under fee for service, the situation is even worse: More than 90% of such opportunities will probably fall by the wayside. Population-based payment has other advantages as well:
Higher returns.For care delivery groups, waste elimination under PBP has a far more positive financial impact than revenue enhancements do under pay-for-volume systems. Only 5% to 9% of all new revenues from a successful, well-managed new fee-for-service or per case service will find their way to a care delivery organization’s bottom line. From 50% to 100% of the savings generated through waste elimination in a PBP system will.
A bigger opportunity for more providers.The total size of the opportunity—a minimum of $1 trillion a year in the United States—dwarfs any financial gains from offering new services. Any competent care delivery group can immediately act on that opportunity; that’s not true with new services. Eliminating waste often requires much smaller investments than launching new services, especially if those services rely on cutting-edge technologies.
Cheaper, higher-quality care for patients.PBP would create a market in which care delivery organizations would compete for patients on the basis of the cost and quality of their clinical services. Competition would prod them to pass some of the savings on to patients and to give them better care.
Judging by what’s going on in the market beyond the Medicare initiatives, others seem to agree that the population-based payment model is best. An increasing number of care delivery groups have started their own insurance companies or partnered with existing insurers, and many large health insurers have purchased care delivery groups. Combining care delivery and insurance in one organization creates a de facto population-based payment system.
Finding the Tipping PointMost care delivery groups now navigate a complex mix of discounted fee-for-service (commercial insurance) and per case (Medicare, plus some commercial insurance) payment. Population-based payment—capitated payment made directly to care delivery groups—remains relatively rare. Yet if it were adopted more broadly, groups that aggressively cut waste, as Intermountain did, would benefit financially; the revenues they received for treating each patient would hold steady, while their costs would fall. The key is identifying and reaching the tipping point: the proportion of a group’s total payment that must come through capitation in order for gains from waste elimination under PBP to outweigh losses under other payment systems.
To explore that question, we built mathematical and empirical models. Under conditions simulating the operations of both community care groups and academic medical centers, the tipping point was consistently below 30%. If 23% to 29% of a group’s payments came through PBP, the group improved its finances by concentrating on waste elimination.
Answering the CriticsOpponents of population-based payments raise three main concerns about them—all of which we believe are unfounded.
Objection 1: PBP’s financial incentives will cause rationing, leading clinicians to withhold necessary care.Some critics cite the 1990s HMO experience to support that viewpoint. But they are wrong for a number of reasons.
First, the science of assessing clinical quality, while still imperfect, is dramatically better than it was in the 1990s. To a much greater degree than the HMOs of that era, all proposals for pay-for-value, including capitated payment, contain measures to ensure that each patient receives all necessary and beneficial care, at least to the degree achieved by the current fee-for-service and per case payment systems.
Second, the HMO movement placed oversight of care decisions in the hands of an insurance company. That created conflict between patients and their clinicians on one side and a distant, financially driven corporation on the other. Making capitated payments directly to care delivery groups and eliminating the insurers’ supervisory role remove the fundamental conflict that doomed the HMO movement.
Finally, there is solid historical evidence that when physicians are asked to take costs into account in treatment decisions, the vast majority consistently do what’s clinically best for the patient. During the 1930s and the 1940s, before broadly available third-party payment for health care, physicians routinely considered a family’s resources when providing care. During HMOs’ heyday, concerns about rationing were fears, not reality: Empirical measurement of quality showed, on average, a slight but significant increase in the quality of care.
The healing professions select for ethical behaviors, train their members deeply in them, and monitor for violations. While failures do occur, they’re rare. When they happen, they’re corrected. The medical professions’ ethical codes of conduct actually work.
Objection 2: Care delivery groups are not best equipped to address problems of fragmented care and to promote population health.
Most people agree on the need to better coordinate care delivery in the United States. The current system is deplorably fragmented, forcing patients to navigate a confusing maze of independent primary, specialty, and hospital care. There’s also consensus that the country should expand population-wide efforts to promote healthful lifestyles and immunization to prevent diseases, and early detection to nip them in the bud. Some argue that health insurance companies are best positioned to achieve these goals.
We disagree for several reasons. While it’s true that coordinated care is essential to reducing waste and increasing quality, it works most effectively and efficiently when embedded within an integrated care delivery organization—a network of providers that have agreed to offer a continuum of care to a defined population and to be accountable for clinical and financial outcomes. Such groups already account for between a third and half of all care delivery in the country, and their share is growing rapidly. Even if an integrated care delivery group doesn’t contain every essential service, it’s as well positioned as an insurance company to partner with other providers for additional services. Moreover, we estimate that at least one-third of all opportunities to improve population-level health reside exclusively within specialty and hospital-based care delivery—well outside the reach of insurance companies. The new way to treat newborns with immature lungs cited earlier is one of many such examples.
PBP gives providers strong incentives to do interventions that reduce care needs.
Last, even when insurance companies do have some ability to address population-level waste, care delivery groups are still more effective at it. For example, Intermountain has found that embedding “appropriate use criteria” in clinical practice, where physicians consult with patients to make treatment choices, prevents unnecessary or harmful care better than insurance-based preauthorization does. Intermountain’s cardiologists, for instance, routinely employ such formal evidence-based criteria when counseling patients who might need heart catheterization, stents in the arteries that supply blood to the heart, or permanent heart pacemakers and defibrillators. The result is that the use of such treatments has fallen by almost 25% below Intermountain’s already low rates, eliminating about $30 million in waste annually. Meanwhile, quality measures showed slight improvements in clinical outcomes.
Objection 3: It would be better to expand bundled payments.
The use of bundled payments has focused mostly on clinical conditions with well-defined boundaries, such as cataract eye surgery, total joint replacements, uncomplicated deliveries, and simple outpatient upper respiratory infections. Some propose applying it to more-complex cases, such as the management of chronic diseases like diabetes, heart failure, and asthma. That approach, they argue, would give patients greater choice and make health care markets more competitive. (See “How to Pay for Health Care” by Michael E. Porter and Robert S. Kaplan.)
This approach to bundled payments is sometimes called “disease capitation.” It’s a very small step away from full capitation. It attempts to push actuarial risk analysis down to the individual patient level, rather than analyzing risk for a group of patients. Such analysis is technically difficult. In addition, this approach could create strong incentives for care delivery groups to select patients, conditions, and treatments based on financial returns rather than patient need.
Most people who have chronic diseases such as heart failure, hypertension, asthma, and depression suffer from several at once. This is especially true with elderly patients, whose needs often include palliative care, help with bowel issues, and general pain control. Any care delivery group has to treat the whole person, not just the disease; it must supply comprehensive care for all of a patient’s conditions, either by providing it directly or coordinating with other groups. Bundled payment systems, however, spur patients to seek out highly specialized groups that treat only one disease and its related conditions.
Finally, bundled payments don’t directly encourage prevention. In contrast, PBP gives care provider groups strong incentives to perform interventions so that their services aren’t needed in the first place—something capitated care delivery groups are starting to do under the banner of “population health.”
Proof That Population-Based Payment Works
The experience of Intermountain Healthcare, which serves about 2 million people in Utah, Idaho, and surrounding states, shows that a population-based payment model is viable.
Intermountain has its own insurance subsidiary: SelectHealth, the largest commercial health insurer in the region, which has some 800,000 enrolled members. Through its commercial insurance business, capitated Medicare Advantage programs, and a new capitated Medicaid program introduced by the state of Utah, SelectHealth now pays for more than 30% of all care delivered within the Intermountain system. Add true charitable care, and capitated care accounts for over 35% of Intermountain’s business.
As a nonprofit with a social mission, Intermountain regards the patients and communities it serves as its “shareholders.” Its leaders and trustees believe that access to care is paramount. In 2011, recognizing that access depends on affordability, Intermountain’s CFO set a goal of dropping the group’s year-over-year rate increases within 1% of the consumer-price-index inflation rate by the end of 2016.
Intermountain is making good progress toward that goal. Through 2015, waste elimination reduced its total cost of operations (“revenues,” under traditional fee-for-service-based health care accounting systems) by 13%. But since more than 35% of Intermountain’s care is now compensated through capitated payment—well past the tipping point—the group has been able to remain financially strong: With consistently healthy operating margins, it boasts the highest bond ratings in the industry. The cardiac-medication and newborn initiatives, which initially hurt Intermountain’s operating income, now make financial contributions. So do a whole host of other waste reduction innovations, such as a new supply-chain management system, the introduction of best-practice standards for high-volume diseases, and primary care clinics that coordinate all aspects of medical and social services.
If 35% to more than 50% of total health care spending is wasted, then the 13% drop in operating costs that Intermountain has achieved is merely a good start. Large financial opportunities remain.
In 2014, Intermountain, which employs more than 1,350 physicians, launched a new program that allows interested independent physicians to participate in population-health efforts and share in the savings they generate. Under the modified fee-for-service system described earlier, these physicians, along with the employed group, receive significant payment when total costs are reduced, patient satisfaction is increased, and quality measures—which guarantee that no physician is withholding beneficial care—improve. About 1,200 of the more than 4,000 independent physicians that work with Intermountain have signed up.
In the fall of 2015, Intermountain used the savings generated by waste elimination to offer business customers a new insurance product. It limits total rate increases to 4% a year for three years—a level likely to be one-half to one-third of general insurance rate increases in Intermountain’s markets. The organization sees this as a “dividend” to its “shareholders”—the patients and communities it serves. In return for low rates, businesses have to participate in disease prevention and activities that promote better health—for example, encouraging their employees to exercise regularly and eat wisely, to stop using tobacco products, to avoid excessive alcohol consumption, and so on.
Deming got it right. Raising quality by reducing process variations and rework can eliminate waste and bring down operating costs. Better products at lower costs generate higher value, which helps organizations achieve better market positions. Strategies based on that thinking have transformed other industries. We believe that they will do the same in health care. Population-based payment will play a critical role in helping care delivery groups make that leap.
A version of this article appeared in the July–August 2016 issue (pp.102–111) of Harvard Business Review.
Read more on Business and society or related topics Corporate social responsibility and Healthcare sector
It’s the only way to cut waste while improving quality. by Brent C. James, MD and Gregory P. Poulsen
From the Magazine (July–August 2016)
Harvard Business Review
Summary. Recent studies suggest that at least 35%—and maybe over 50%—of all health care spending in the U.S. is wasted on inadequate, unnecessary, and inefficient care and suboptimal business processes. But efforts to get rid of that waste face a huge challenge.
To rein in health care costs in the United States, we should look to the ideas of W. Edwards Deming, the legendary management guru who showed companies how to cut waste from work processes and lower operating costs by improving quality. Recent studies using Deming’s approach reveal that inadequate, unnecessary, uncoordinated, and inefficient care and suboptimal business processes eat up at least 35%—and maybe over 50%—of the more than $3 trillion that the country spends annually on health care. That suggests more than $1 trillion is being squandered.
Ongoing reform efforts by the federal government and private insurers have had some success in prodding health care providers to improve quality and reduce waste. But it’s far from certain that they’ll be enough. Even after taking existing and proposed reform initiatives into account, federal projections show health care expenditures consuming larger and larger proportions of the GDP. Moreover, under the prevailing payment models, which are based on volume of services, providers often don’t receive any of the savings from waste reduction, which undermines both their financial health and their ability to continue to invest in such efforts.
The solution to this quandary is to change the way businesses, government, and other purchasers pay for health care to population-based payment. Under this approach, providers receive a fixed per person (or “capitated”) payment that covers all health care services over a defined time period, adjusted for each patient’s expected needs, and are also held accountable for high-quality outcomes. It’s the only payment system that fully aligns providers’ financial incentives with the goal of eliminating all major categories of waste. It fundamentally shifts the role of managing the amount, form, and cost of care from insurers to medical practitioners. It also ensures that providers receive enough of the savings that they can afford to fund the changes needed to bring down costs.
A population-based payment model also has major implications for pure health insurers: Because it removes care oversight from their purview, it leaves them only traditional insurance functions such as claims processing, risk analysis, reinsurance, marketing, and customer service. Many nonprofit health insurers competently provide a full range of such services for less than 10% of total health insurance payments, well below the portion that many health insurers now extract through current systems.
In this article we’ll look at the different categories of waste in health care and then outline the various payment methods that have evolved in the United States and their effect on waste. We’ll then demonstrate how population-based payment, backed by good reporting, can improve clinical results, eliminate unnecessary spending, and lower costs.
Three Kinds of WasteIn health care there are three basic categories of waste: production-level waste, case-level waste, and population-level waste.
Half of all waste in care delivery is unnecessary or suboptimal care.
The first category involves inefficiencies in producing “units of care”—drugs, lab tests, x-rays, hours of nursing support, and any other item consumed in patient treatment. It accounts for about 5% of total health care waste. Eliminating it requires things like negotiating down prices for supplies, lowering handling and storage costs, streamlining processes for producing lab tests or x-rays, and reducing losses due to damage, misplacement, or expiration.
The second category, which comprises about half of all waste in care delivery, is unnecessary or suboptimal use of care during a hospital stay, an outpatient visit, or some other treatment episode, or “case.” Examples include redundant x-rays ordered when the original images couldn’t be found, duplicate lab tests ordered because a physician didn’t know that someone else had already done the tests, and medications prescribed to treat avoidable complications.
The third category, which accounts for about 45% of total waste, involves cases within a patient population that are unnecessary or preventable. It includes end-of-life intensive care given to people who’ve expressly asked not to receive it; elective surgical procedures that, with better information, patients would have forgone; and visits to specialists or hospitalizations that could have been avoided through timely, cheaper outpatient care. Waste here obviously feeds waste at the other two levels, since each unnecessary or avoidable case consumes care.
The Impact of Different Payment ModelsTo understand what’s driving up health care spending, it’s critical to examine whether—and to what extent—health care payment methods encourage or discourage waste reduction. An optimal payment method must address two important challenges. One is how to divvy up the savings generated by eliminating waste. If most or all of the money goes to health care payers, providers have no incentive to cut waste. If most or all of it goes to providers, how do you ensure that they pass on some of it to customers—especially if there is no efficient market, which, we’d argue, you often can’t create in health care because of its complexities? Another issue is how a payment method affects the power of patients and their physicians to make decisions that are in patients’ best interests. Let’s look at the methods that have evolved in the United States over the years and see how each stacks up.
Cost-plus.In 1965, as part of the War on Poverty, the U.S. Congress enacted the Medicare and Medicaid government-funded health insurance programs. Those programs paid physicians and hospitals on a cost-plus basis. Care providers estimated their cost for delivering each unit of care, and then the government paid that cost plus a markup. The result was that providers could basically consume whatever resources they wanted—and had no incentive to reduce spending. Today cost-plus payment persists only in small pockets of health care, such as some specialty hospitals and some small rural hospitals.
Fee for service.
Until the 1980s there was little standardization in the way hospitals and physicians billed payers for individual units of care such as lab tests, supplies, or medical services. Then, in a bid to control costs, Medicare began to organize some of the fee categories, and a degree of standardization emerged for the prices and nomenclature of most items, for commercial as well as government payers.
Under the fee-for-service payment method, a provider supplies an approved billing code for (and may be required to justify) each unit of care consumed during a hospitalization, same-day procedure, or outpatient visit. It cannot bill for anything that lacks a code. For each billed item the government pays the lesser of the group’s actual billed charges or a federal maximum allowed rate. (The method it uses to calculate that rate isn’t strongly linked to true underlying costs and is controversial.) As a result, care delivery groups try to ensure that their billed charges are above the federal rates. Given that the rates change constantly as the government updates its estimates, the easiest way for a group to guarantee maximum payment is to set high prices for everything.
Fee for service also encourages care deliverers to provide as much care as possible, regardless of whether it’s all necessary or optimal. Because of that, the types and volume of care used to treat a given disease vary widely, making it difficult to compare the true cost of care across providers. As a result, commercial insurers often base purchasing decisions on percentage discounts they’ve negotiated with care delivery groups. That in turn leads some groups to apply very high markups—so that they can offer large discounts to the insurers.
Fee for service neither effectively promotes the elimination of all kinds of waste nor allocates savings among providers, payers, and patients in a way that would fuel continual improvements. Despite its widely acknowledged deficiencies, it remains the most common payment method in the United States. It forms the basis for nearly all accounting systems used by care delivery groups and health care insurers.
Per case.
This payment method dates back to 1983, when the federal government introduced the “diagnosis-related group” (DRG) system for Medicare patients. Again, the primary purpose was cost control. Currently, DRGs classify hospital and same-day surgery patients into 753 unique categories, on the basis of each patient’s primary disease, specific treatment, secondary chronic conditions, and care intensity. For example, DRG 7 is a lung transplant, DRG 179 uncomplicated pneumonia, and DRG 343 a simple appendectomy. Medicare pays facilities, such as hospitals or surgery centers, a flat rate per case in each category. Meanwhile, it pays physicians involved in the same cases on a fee-for-service basis. Commercial insurers sometimes pay hospitals and surgery centers per case but pay the physicians providing treatment via fee for service.
In 2016 the government introduced “bundled” per case payments in its Medicare program, following an approach first tried by a handful of commercial health insurers. The initial federal experiment focuses on total hip- and total knee-joint-replacement surgery. It extends the single flat-rate DRG payment to include all physician fees and all costs of any related treatments, complications, or hospital readmissions within 90 days of the original operation. If the experiment successfully reduces costs, the government plans to extend it to other types of cases.
Per case payment gives providers incentives to improve efficiency within cases but, like fee for service, is a volume-based system that fuels waste. The more cases a care delivery group handles, the more it gets paid. Therefore, it’s in the group’s financial interest to maximize the number of cases it treats, even if some add no value or actively harm patients.
Capitation.
In contrast to fee-for-service and per case payment methods, per person payment methods can encourage waste reduction at all three levels and give patients and physicians the freedom to make the treatment decisions they think are best. But to function well, such systems must adjust payments for risk, which is easier to do at the level of a population than of an individual patient. (A typical population is a business’s employees and their dependents.) There have to be quality measures to ensure that providers don’t withhold necessary care. And finally, savings from waste reduction must go back to care delivery groups to keep them financially viable.
The last widespread use of capitation in the U.S. didn’t meet the last two criteria. In the late 1980s and into the 1990s, both government and private payers looked for ways to reduce health care inflation. The primary mechanism they turned to was health maintenance organizations (HMOs), which were usually owned and managed by insurance companies. While employers generally paid HMOs on a capitated basis, most HMOs continued to pay care delivery groups using fee-for-service and per case methods.
HMOs employed a series of tools to limit health care consumption. For example, many mandated that primary care physicians act as gatekeepers. Care providers had to get permission from nurses and doctors based at insurance companies to make referrals to specialists and order surgical procedures, imaging, and hospitalizations. In some instances the HMOs passed along a portion of the capitated insurance payment to the provider groups to cover all necessary services, which transferred the financial risk to them.
HMOs succeeded in curbing expenditures. Health care costs as a proportion of GDP remained flat from 1993 through 2000—even though one reason was that the GDP was growing rapidly, hiding the price increases that did occur. However, the insurance companies weren’t in the best position to make health care decisions, because they were removed from patient-clinician interactions. The HMOs’ bureaucratic controls imposed hassles and treatment delays. Some physician groups, unable to manage care costs after accepting capitated payments, failed financially. Patients and physicians rebelled, arguing that the financial incentives built into capitated payments led HMOs to ration care and accusing insurance companies of putting profits before patients’ health. The resulting political backlash ended insurance-company-based cost control as a national movement.
A Better Capitation Model
A population-based payment system would differ from the capitated method most insurance companies use in significant ways. With PBP, care provider organizations would receive a risk-adjusted monthly payment that covers all necessary health services for each person. Eliminating the gatekeeper and the third-party authorization for care that made HMOs so unpopular, PBP would put responsibility for considering the cost of treatment options in the hands of physicians as they consult with patients. Finally, unlike HMOs of the 1990s, PBP would include quality measures and standards. A care delivery group would pay independent physicians using existing fee-for-service mechanisms but would adjust payments quarterly according to the levels of clinical quality and patient satisfaction achieved as well as total cost to care for the covered population. The advantage of this approach is that it would build on a system physicians already understand while rewarding them for improvements in quality and cost, which would compensate them for income lost if total care volumes decline as a result of waste elimination.
Federal cost control efforts mandated by the Affordable Care Act of 2010 are pushing health care payments in this direction. Recognizing that volume-based payments fuel expenditures, increase waste, and potentially worsen quality, government officials are moving toward “pay for value” systems, which give providers financial incentives to hold costs down by improving clinical outcomes and patient satisfaction. To do this, they’re implementing the initiatives below—each of which represents a step along the spectrum toward full capitated payment:
- Mandatory reporting of quality and patient satisfaction for all care delivered under Medicare, with financial penalties for care delivery groups that don’t meet standards or that rank poorly compared with other groups.
- The Medicare bundled payment experiment launched this year.
- The Medicare Shared Savings Program, under which a care delivery group is paid via traditional fee for service and per case DRGs but receives a portion of any savings it achieves through care coordination and waste reduction.
- Alternative payment models, including patient-centered medical homes and accountable care organizations (ACOs) for Medicare patients. These programs also pay via fee for service and per case but give care delivery groups a potentially larger share of the savings, provided their charges come in under preset spending levels. However, if charges exceed the preset levels, care delivery groups may have to absorb them.
- Full capitated payment. The federal government is launching “next-generation ACOs,” in which a care delivery group receives a monthly capitated payment that covers all health services for Medicare patients enrolled with it, adjusted for their expected health needs. Different care delivery groups (including our organization, Intermountain Healthcare) are proposing—and the government is likely to approve—different forms. It may take a few years, after these experiments produce results, for the definitive form to emerge.
We recommend that, where possible, care providers jump directly to population-based payment and that payers actively support them in that move. Of the pay-for-value methods just listed, it’s the only one that gives care delivery groups the financial incentives to attack all three levels of waste. More specifically, it’s the only one that ensures that care delivery groups capture enough of the savings from waste elimination that they stay financially viable and can continue to invest in such programs. Let us explain.
To raise quality and eliminate waste in health care, we need to do more than end production inefficiencies and unnecessary or inappropriate treatments. Care providers also have to develop, test, and repeatedly improve new care delivery processes—and that requires investment. A major problem with fee-for-service and per case payments is that they redirect the savings away from those who must make the investment and into the pockets of insurance companies. Consider these two examples:
Congestive heart failure and ischemic heart disease (compromised blood flow to the heart) are very common conditions, especially among Medicare patients. Certain medications (beta blockers and ACE and ARB inhibitors), taken every day, can stabilize patients’ conditions and prevent death. The key is recognizing which people need the medications and getting them started on them.
Nationwide, hospitals prescribe the right long-term medications for these two conditions to their patients only 44% of the time. Intermountain Healthcare’s LDS Hospital in Salt Lake City developed a system that boosted its accuracy rate from 57% to over 98%. As a result, mortality fell by more than 450 deaths a year, and hospitalizations by almost 900 cases a year. The majority of those cases were paid through Medicare, on the per case DRG system. The lower hospitalization rate meant that LDS Hospital lost $3.2 million a year in revenues, along with associated operating income. From a purely financial viewpoint, its investment in improving patient outcomes and lowering costs worked out very poorly indeed.
When Intermountain rolled out a better lung treatment for babies, it lost $5 million.
Intermountain’s American Fork Hospital had a large birthing service. About 110 of its newborns each year were borderline premature—with a 34- to 37-week gestation versus the normal 40 weeks. Often the lungs of premature babies are not fully developed, which means they can collapse. In the distant past, most of these “blue babies” died. Then clinicians learned to place a breathing tube through an infant’s mouth into its major airway and use a mechanical ventilator to keep the lungs inflated for a few weeks. This gave infants’ lungs time to mature, and mortality rates plummeted. Unfortunately, intubation and mechanical ventilation are highly invasive, and some babies suffered significant complications.
A group of obstetricians and neonatologists at American Fork Hospital argued that since borderline preemies have lungs that are almost mature, a milder intervention, “nasal continuous positive airway pressure,” which involves blowing pressurized air through the newborn’s nose, might work. In a clinical trial, intubation rates fell from 78% to 18%. The children stayed in the nursery, not the far more expensive newborn ICU. With the simpler, less invasive care, the hospital’s total operating costs for these children fell by $544,000 a year. But fee-for-service insurance payments dropped by $873,000, causing a $329,000 dip in the hospital’s operating income. The hospital also had to bear the costs of developing and implementing the change. Moreover, when Intermountain decided to deploy the new methods across all its hospitals—clearly the right thing to do for the children—that $329,000 turned into more than $5 million in annual losses.
These examples raise critical questions: Should care delivery groups invest in quality improvements that reduce costs if it could mean their own financial demise? Even if a group does so because it’s the right thing for patients, where will it find the resources to launch its next waste reduction project? Shouldn’t the windfall that health insurers receive from waste reduction help fund further improvements? If sharing in the savings strengthened the care delivery group financially, wouldn’t it become a more effective competitor, encouraging other groups to adopt the same cost-saving strategies?
We believe that population-based payment addresses these issues, because it encourages providers to attack all waste, by ensuring that they benefit from the savings. Because per case systems, including the new bundled payment approaches, don’t offer the right financial incentives, close to half of all waste reduction opportunities are likely to go unrealized under them. Under fee for service, the situation is even worse: More than 90% of such opportunities will probably fall by the wayside. Population-based payment has other advantages as well:
Higher returns.For care delivery groups, waste elimination under PBP has a far more positive financial impact than revenue enhancements do under pay-for-volume systems. Only 5% to 9% of all new revenues from a successful, well-managed new fee-for-service or per case service will find their way to a care delivery organization’s bottom line. From 50% to 100% of the savings generated through waste elimination in a PBP system will.
A bigger opportunity for more providers.The total size of the opportunity—a minimum of $1 trillion a year in the United States—dwarfs any financial gains from offering new services. Any competent care delivery group can immediately act on that opportunity; that’s not true with new services. Eliminating waste often requires much smaller investments than launching new services, especially if those services rely on cutting-edge technologies.
Cheaper, higher-quality care for patients.PBP would create a market in which care delivery organizations would compete for patients on the basis of the cost and quality of their clinical services. Competition would prod them to pass some of the savings on to patients and to give them better care.
Judging by what’s going on in the market beyond the Medicare initiatives, others seem to agree that the population-based payment model is best. An increasing number of care delivery groups have started their own insurance companies or partnered with existing insurers, and many large health insurers have purchased care delivery groups. Combining care delivery and insurance in one organization creates a de facto population-based payment system.
Finding the Tipping PointMost care delivery groups now navigate a complex mix of discounted fee-for-service (commercial insurance) and per case (Medicare, plus some commercial insurance) payment. Population-based payment—capitated payment made directly to care delivery groups—remains relatively rare. Yet if it were adopted more broadly, groups that aggressively cut waste, as Intermountain did, would benefit financially; the revenues they received for treating each patient would hold steady, while their costs would fall. The key is identifying and reaching the tipping point: the proportion of a group’s total payment that must come through capitation in order for gains from waste elimination under PBP to outweigh losses under other payment systems.
To explore that question, we built mathematical and empirical models. Under conditions simulating the operations of both community care groups and academic medical centers, the tipping point was consistently below 30%. If 23% to 29% of a group’s payments came through PBP, the group improved its finances by concentrating on waste elimination.
Answering the CriticsOpponents of population-based payments raise three main concerns about them—all of which we believe are unfounded.
Objection 1: PBP’s financial incentives will cause rationing, leading clinicians to withhold necessary care.Some critics cite the 1990s HMO experience to support that viewpoint. But they are wrong for a number of reasons.
First, the science of assessing clinical quality, while still imperfect, is dramatically better than it was in the 1990s. To a much greater degree than the HMOs of that era, all proposals for pay-for-value, including capitated payment, contain measures to ensure that each patient receives all necessary and beneficial care, at least to the degree achieved by the current fee-for-service and per case payment systems.
Second, the HMO movement placed oversight of care decisions in the hands of an insurance company. That created conflict between patients and their clinicians on one side and a distant, financially driven corporation on the other. Making capitated payments directly to care delivery groups and eliminating the insurers’ supervisory role remove the fundamental conflict that doomed the HMO movement.
Finally, there is solid historical evidence that when physicians are asked to take costs into account in treatment decisions, the vast majority consistently do what’s clinically best for the patient. During the 1930s and the 1940s, before broadly available third-party payment for health care, physicians routinely considered a family’s resources when providing care. During HMOs’ heyday, concerns about rationing were fears, not reality: Empirical measurement of quality showed, on average, a slight but significant increase in the quality of care.
The healing professions select for ethical behaviors, train their members deeply in them, and monitor for violations. While failures do occur, they’re rare. When they happen, they’re corrected. The medical professions’ ethical codes of conduct actually work.
Objection 2: Care delivery groups are not best equipped to address problems of fragmented care and to promote population health.
Most people agree on the need to better coordinate care delivery in the United States. The current system is deplorably fragmented, forcing patients to navigate a confusing maze of independent primary, specialty, and hospital care. There’s also consensus that the country should expand population-wide efforts to promote healthful lifestyles and immunization to prevent diseases, and early detection to nip them in the bud. Some argue that health insurance companies are best positioned to achieve these goals.
We disagree for several reasons. While it’s true that coordinated care is essential to reducing waste and increasing quality, it works most effectively and efficiently when embedded within an integrated care delivery organization—a network of providers that have agreed to offer a continuum of care to a defined population and to be accountable for clinical and financial outcomes. Such groups already account for between a third and half of all care delivery in the country, and their share is growing rapidly. Even if an integrated care delivery group doesn’t contain every essential service, it’s as well positioned as an insurance company to partner with other providers for additional services. Moreover, we estimate that at least one-third of all opportunities to improve population-level health reside exclusively within specialty and hospital-based care delivery—well outside the reach of insurance companies. The new way to treat newborns with immature lungs cited earlier is one of many such examples.
PBP gives providers strong incentives to do interventions that reduce care needs.
Last, even when insurance companies do have some ability to address population-level waste, care delivery groups are still more effective at it. For example, Intermountain has found that embedding “appropriate use criteria” in clinical practice, where physicians consult with patients to make treatment choices, prevents unnecessary or harmful care better than insurance-based preauthorization does. Intermountain’s cardiologists, for instance, routinely employ such formal evidence-based criteria when counseling patients who might need heart catheterization, stents in the arteries that supply blood to the heart, or permanent heart pacemakers and defibrillators. The result is that the use of such treatments has fallen by almost 25% below Intermountain’s already low rates, eliminating about $30 million in waste annually. Meanwhile, quality measures showed slight improvements in clinical outcomes.
Objection 3: It would be better to expand bundled payments.
The use of bundled payments has focused mostly on clinical conditions with well-defined boundaries, such as cataract eye surgery, total joint replacements, uncomplicated deliveries, and simple outpatient upper respiratory infections. Some propose applying it to more-complex cases, such as the management of chronic diseases like diabetes, heart failure, and asthma. That approach, they argue, would give patients greater choice and make health care markets more competitive. (See “How to Pay for Health Care” by Michael E. Porter and Robert S. Kaplan.)
This approach to bundled payments is sometimes called “disease capitation.” It’s a very small step away from full capitation. It attempts to push actuarial risk analysis down to the individual patient level, rather than analyzing risk for a group of patients. Such analysis is technically difficult. In addition, this approach could create strong incentives for care delivery groups to select patients, conditions, and treatments based on financial returns rather than patient need.
Most people who have chronic diseases such as heart failure, hypertension, asthma, and depression suffer from several at once. This is especially true with elderly patients, whose needs often include palliative care, help with bowel issues, and general pain control. Any care delivery group has to treat the whole person, not just the disease; it must supply comprehensive care for all of a patient’s conditions, either by providing it directly or coordinating with other groups. Bundled payment systems, however, spur patients to seek out highly specialized groups that treat only one disease and its related conditions.
Finally, bundled payments don’t directly encourage prevention. In contrast, PBP gives care provider groups strong incentives to perform interventions so that their services aren’t needed in the first place—something capitated care delivery groups are starting to do under the banner of “population health.”
Proof That Population-Based Payment Works
The experience of Intermountain Healthcare, which serves about 2 million people in Utah, Idaho, and surrounding states, shows that a population-based payment model is viable.
Intermountain has its own insurance subsidiary: SelectHealth, the largest commercial health insurer in the region, which has some 800,000 enrolled members. Through its commercial insurance business, capitated Medicare Advantage programs, and a new capitated Medicaid program introduced by the state of Utah, SelectHealth now pays for more than 30% of all care delivered within the Intermountain system. Add true charitable care, and capitated care accounts for over 35% of Intermountain’s business.
As a nonprofit with a social mission, Intermountain regards the patients and communities it serves as its “shareholders.” Its leaders and trustees believe that access to care is paramount. In 2011, recognizing that access depends on affordability, Intermountain’s CFO set a goal of dropping the group’s year-over-year rate increases within 1% of the consumer-price-index inflation rate by the end of 2016.
Intermountain is making good progress toward that goal. Through 2015, waste elimination reduced its total cost of operations (“revenues,” under traditional fee-for-service-based health care accounting systems) by 13%. But since more than 35% of Intermountain’s care is now compensated through capitated payment—well past the tipping point—the group has been able to remain financially strong: With consistently healthy operating margins, it boasts the highest bond ratings in the industry. The cardiac-medication and newborn initiatives, which initially hurt Intermountain’s operating income, now make financial contributions. So do a whole host of other waste reduction innovations, such as a new supply-chain management system, the introduction of best-practice standards for high-volume diseases, and primary care clinics that coordinate all aspects of medical and social services.
If 35% to more than 50% of total health care spending is wasted, then the 13% drop in operating costs that Intermountain has achieved is merely a good start. Large financial opportunities remain.
In 2014, Intermountain, which employs more than 1,350 physicians, launched a new program that allows interested independent physicians to participate in population-health efforts and share in the savings they generate. Under the modified fee-for-service system described earlier, these physicians, along with the employed group, receive significant payment when total costs are reduced, patient satisfaction is increased, and quality measures—which guarantee that no physician is withholding beneficial care—improve. About 1,200 of the more than 4,000 independent physicians that work with Intermountain have signed up.
In the fall of 2015, Intermountain used the savings generated by waste elimination to offer business customers a new insurance product. It limits total rate increases to 4% a year for three years—a level likely to be one-half to one-third of general insurance rate increases in Intermountain’s markets. The organization sees this as a “dividend” to its “shareholders”—the patients and communities it serves. In return for low rates, businesses have to participate in disease prevention and activities that promote better health—for example, encouraging their employees to exercise regularly and eat wisely, to stop using tobacco products, to avoid excessive alcohol consumption, and so on.
Deming got it right. Raising quality by reducing process variations and rework can eliminate waste and bring down operating costs. Better products at lower costs generate higher value, which helps organizations achieve better market positions. Strategies based on that thinking have transformed other industries. We believe that they will do the same in health care. Population-based payment will play a critical role in helping care delivery groups make that leap.
A version of this article appeared in the July–August 2016 issue (pp.102–111) of Harvard Business Review.
Read more on Business and society or related topics Corporate social responsibility and Healthcare sector
- Brent C. James, MD, is Intermountain Healthcare’s chief quality officer and leads the Intermountain Institute for Healthcare Delivery Research. He is a member of the National Academy of Medicine and a professor of clinical medicine (affiliated) at the Stanford University School of Medicine. He holds adjunct faculty appointments at the Harvard School of Public Health and the University of Utah School of Medicine.
- Gregory P. Poulsen is Intermountain Healthcare’s senior vice president and chief strategy officer. He is a trustee of the American Board of Internal Medicine Foundation and a national guest scholar at the Stanford University School of Medicine.
Capitation Payments: Definition, How They Work, and Calculation
By JULIA KAGAN
Reviewed by THOMAS J. CATALANO
Updated September 28, 2023
What Are Capitation Payments?Capitation payments are payments agreed upon in a capitated contract by a health insurance company and a medical provider. They are fixed, pre-arranged monthly payments received by a physician, clinic, or hospital per patient enrolled in a health plan, or per capita. The monthly payment is calculated one year in advance and remains fixed for that year, regardless of how often the patient needs services.
KEY TAKEAWAYS
Money in this risk pool is withheld from the physician until the end of the fiscal year. If the health plan does well financially, the medical provider receives this money; if the health plan does poorly, the money is kept to pay the deficit expenses.
The amount of the capitation will be determined, in part, by the number of services provided and will vary from health plan to health plan. Most capitation payment plans for primary care services include basic areas of healthcare:
There are two types of capitation relationships. The first is where the provider is paid directly by the insurer, also called a primary capitation. Then, a secondary capitation is where another provider (such as a lab or medical specialist) is paid out of the provider’s funds.
Another form of capitation may encourage preventative health services. With capitations that encourage preventative care, the provider is rewarded for providing preventive health care services. This incentivizes the doctor or provider to help avoid expensive medical services.
Capitation agreements will provide a list of specific included services in the contract.
Capitation is meant to help limit excessive costs and the performance of unnecessary services. But on the downside, it might also mean that patients get less facetime with the doctor. Providers may look to increase profitability under the capitation model by cutting down on the time that patients see the doctor.
Compared with the capitation alternative, fee-for-service (FFS), it’s supposed to be more cost-effective, hence the reason providers look to limit face time with doctors. FFS pays providers based on the number of services provided—unlike capitations that pay based on the number of participants in the group. Studies from many years suggest capitation is more cost-effective among groups that have a high amount of individuals with moderate health care needs.2
At the same time, it’s been shown that capitation systems encourage doctors to reduce services. A Center for Studying Health System Change study found that 7% of doctors in a capitation system reduce services because there’s financial incentive to do so.3
Advantages and Disadvantages of Capitation PaymentsCapitation payments have various advantages when it comes to the alternative—FFS. However, some providers may still opt for FFS given its advantages over capitation.
Advantages of CapitationThe alternative to capitation payments is FFS, where providers are paid based on the number of services provided. Perhaps the biggest benefit to capitation contracts is that they provide fixed payments to providers, dissuading the incentive to order more procedures than necessary, which can be an issue with FFS (i.e. capitation provides greater provider accountability).
As well, the fixed payments by capitation offer greater financial certainty for providers. They can focus on face-to-face services and explore cost-effective care that provides the best treatment. Along those lines, providers have a greater incentive to encourage preventative care.
Disadvantages of CapitationOn the downside, a capitation arrangement can lead providers to opt for less expensive drugs or procedures. That is, providers opt to not use name-brand products to save money. Capitation can also encourage providers to enroll large numbers of patients, which can lead to short visits for patients and long wait times.
Financial risk for patients with major medical issues is borne by the provider in the case of capitation agreements. In higher population areas, the capitation rates might be on the low side. In those circumstances, the provider may supplement the capitation model with FFS.
Pros
Cons
The payment varies depending on the capitation agreement, but generally, they are based on characteristics such as the age of the individual enrolled in the plan. Modifying the plan, according to specific characteristics for groups of patients, is one way to compensate providers for the medical care expected for similar ailments within a group.
Health insurance companies use capitation payments to control health care costs. Capitation payments control the use of healthcare resources by putting the physician at financial risk for patient services.
At the same time, in order to ensure that patients do not receive suboptimal care through the under-utilization of health care services, insurance companies measure rates of resource utilization in physician practices. These reports are publicly available and can be linked to financial rewards, such as bonuses.
One major drawback of capitation is that it incentivizes physicians to spend less time with patients—i.e. spending only a few minutes on appointments.
Example of a Capitation PaymentA capitation example would be an IPA—a type of HMO—that has 5,000 patients. The IPA needs to secure insurance coverage for its patients for the upcoming year. Thus, it would enter into a capitation contract with a physician.
The physician would be paid a fixed payment to treat all 5,000 patients. For example, say the capitation fee is $400 per year per patient. The physician would collect $2 million per year from the IPA. In return, the physician would be expected to cover all expenses related to treating those 5,000 patients.
The idea is that not all patients will use $400 in services over the course of the year. Some may use $2,000, but others may only use $100 or none at all. Overall, the doctor is assuming that (on average) the patients from this IPA will use less than $400 each in services.
The capitation payment amount is expected on how much each patient is expected to use the service. Patients, such as those with preexisting conditions, are likely to have higher expected medical needs and costs. It’s in the IPA or HMO's best interest to try and estimate as best as possible the potential utilization of services.
Caput (which means head) is the Latin word that capitation is derived from. Capitation is the headcount for a group (such as IPA or HMO) that the fees are based on.
Capitation FAQsWhat Is a Capitation Agreement?A capitation agreement is an actual contract between the HMO or IPA and the medical provider or doctor. This agreement lays out the details and expectations between the two, including the fixed amount of money (fee) to be paid to the health care provider.
What Are Capitation Fees?Capitation fee, or capitation rate, is the fixed amount paid from an insurer to a provider. This is the amount that is paid (generally monthly) to cover the cost of services performed for a patient. Capitation fees can be lower in higher population areas.
What Is the Difference Between Capitation and Fee-For-Service?Capitation is a model that pays a fixed amount to providers based on the number of patients they have or see. Meanwhile, fee-for-service (FFS) pays based on the procedures or services that providers perform. Both these systems are used in the U.S. healthcare system.2
Bottom LineCapitation payments are payments made to health care providers for providing services to patients. These payments are fixed and generally paid monthly (based on yearly contracts—i.e. capitation contracts).
This system helps doctors reduce bookkeeping, accounting, and other operating costs. Capitation also benefits the HMO or IPA by ensuring that providers don’t undertake more services than necessary. The idea is that it reduces the potential for excessive billing.
SPONSORED
Trade smarter with TradingView and Economic Calendar
Become a smarter trader with eToro’s advanced trading tools: be ready for every market movement, from earnings reports to dividend payments, and get the best out of our technical analysis skills with the power of TradingView charts — all easily accessible on the eToro trading platform. Join eToro today.
By JULIA KAGAN
Reviewed by THOMAS J. CATALANO
Updated September 28, 2023
What Are Capitation Payments?Capitation payments are payments agreed upon in a capitated contract by a health insurance company and a medical provider. They are fixed, pre-arranged monthly payments received by a physician, clinic, or hospital per patient enrolled in a health plan, or per capita. The monthly payment is calculated one year in advance and remains fixed for that year, regardless of how often the patient needs services.
KEY TAKEAWAYS
- Capitation payments are fixed payment amounts between insurers and medical providers as part of the capitation health care payment system.
- It is used by physician associations or insurers to pay hospitals or doctors per enrolled patient for a specific amount of time.
- Rates for capitation payments are developed using local costs and average utilization of services
- HMOs and IPAs tend to benefit from operating in a healthcare capitation payment system.
- Capitation payments are designed to lower the high costs of healthcare.
Money in this risk pool is withheld from the physician until the end of the fiscal year. If the health plan does well financially, the medical provider receives this money; if the health plan does poorly, the money is kept to pay the deficit expenses.
The amount of the capitation will be determined, in part, by the number of services provided and will vary from health plan to health plan. Most capitation payment plans for primary care services include basic areas of healthcare:
- Preventive, diagnostic, and treatment services
- Injections, immunizations, and medications administered in the office
- Outpatient laboratory tests that are done in the office or at a designated laboratory
- Health education and counseling services performed in the office
- Routine vision and hearing screening
There are two types of capitation relationships. The first is where the provider is paid directly by the insurer, also called a primary capitation. Then, a secondary capitation is where another provider (such as a lab or medical specialist) is paid out of the provider’s funds.
Another form of capitation may encourage preventative health services. With capitations that encourage preventative care, the provider is rewarded for providing preventive health care services. This incentivizes the doctor or provider to help avoid expensive medical services.
Capitation agreements will provide a list of specific included services in the contract.
Capitation is meant to help limit excessive costs and the performance of unnecessary services. But on the downside, it might also mean that patients get less facetime with the doctor. Providers may look to increase profitability under the capitation model by cutting down on the time that patients see the doctor.
Compared with the capitation alternative, fee-for-service (FFS), it’s supposed to be more cost-effective, hence the reason providers look to limit face time with doctors. FFS pays providers based on the number of services provided—unlike capitations that pay based on the number of participants in the group. Studies from many years suggest capitation is more cost-effective among groups that have a high amount of individuals with moderate health care needs.2
At the same time, it’s been shown that capitation systems encourage doctors to reduce services. A Center for Studying Health System Change study found that 7% of doctors in a capitation system reduce services because there’s financial incentive to do so.3
Advantages and Disadvantages of Capitation PaymentsCapitation payments have various advantages when it comes to the alternative—FFS. However, some providers may still opt for FFS given its advantages over capitation.
Advantages of CapitationThe alternative to capitation payments is FFS, where providers are paid based on the number of services provided. Perhaps the biggest benefit to capitation contracts is that they provide fixed payments to providers, dissuading the incentive to order more procedures than necessary, which can be an issue with FFS (i.e. capitation provides greater provider accountability).
As well, the fixed payments by capitation offer greater financial certainty for providers. They can focus on face-to-face services and explore cost-effective care that provides the best treatment. Along those lines, providers have a greater incentive to encourage preventative care.
Disadvantages of CapitationOn the downside, a capitation arrangement can lead providers to opt for less expensive drugs or procedures. That is, providers opt to not use name-brand products to save money. Capitation can also encourage providers to enroll large numbers of patients, which can lead to short visits for patients and long wait times.
Financial risk for patients with major medical issues is borne by the provider in the case of capitation agreements. In higher population areas, the capitation rates might be on the low side. In those circumstances, the provider may supplement the capitation model with FFS.
Pros
- Dissuades providers from unnecessary services
- Promotes efficiency and cost-control
- Reduces bookkeeping overhead
- Allows providers to focus on face-to-face services, preventative care
Cons
- May cause providers to use cheaper drugs/services
- Encourages providing fewer services
- High population areas means low capitation rates
- Can lead to long wait times and short visits
The payment varies depending on the capitation agreement, but generally, they are based on characteristics such as the age of the individual enrolled in the plan. Modifying the plan, according to specific characteristics for groups of patients, is one way to compensate providers for the medical care expected for similar ailments within a group.
Health insurance companies use capitation payments to control health care costs. Capitation payments control the use of healthcare resources by putting the physician at financial risk for patient services.
At the same time, in order to ensure that patients do not receive suboptimal care through the under-utilization of health care services, insurance companies measure rates of resource utilization in physician practices. These reports are publicly available and can be linked to financial rewards, such as bonuses.
One major drawback of capitation is that it incentivizes physicians to spend less time with patients—i.e. spending only a few minutes on appointments.
Example of a Capitation PaymentA capitation example would be an IPA—a type of HMO—that has 5,000 patients. The IPA needs to secure insurance coverage for its patients for the upcoming year. Thus, it would enter into a capitation contract with a physician.
The physician would be paid a fixed payment to treat all 5,000 patients. For example, say the capitation fee is $400 per year per patient. The physician would collect $2 million per year from the IPA. In return, the physician would be expected to cover all expenses related to treating those 5,000 patients.
The idea is that not all patients will use $400 in services over the course of the year. Some may use $2,000, but others may only use $100 or none at all. Overall, the doctor is assuming that (on average) the patients from this IPA will use less than $400 each in services.
The capitation payment amount is expected on how much each patient is expected to use the service. Patients, such as those with preexisting conditions, are likely to have higher expected medical needs and costs. It’s in the IPA or HMO's best interest to try and estimate as best as possible the potential utilization of services.
Caput (which means head) is the Latin word that capitation is derived from. Capitation is the headcount for a group (such as IPA or HMO) that the fees are based on.
Capitation FAQsWhat Is a Capitation Agreement?A capitation agreement is an actual contract between the HMO or IPA and the medical provider or doctor. This agreement lays out the details and expectations between the two, including the fixed amount of money (fee) to be paid to the health care provider.
What Are Capitation Fees?Capitation fee, or capitation rate, is the fixed amount paid from an insurer to a provider. This is the amount that is paid (generally monthly) to cover the cost of services performed for a patient. Capitation fees can be lower in higher population areas.
What Is the Difference Between Capitation and Fee-For-Service?Capitation is a model that pays a fixed amount to providers based on the number of patients they have or see. Meanwhile, fee-for-service (FFS) pays based on the procedures or services that providers perform. Both these systems are used in the U.S. healthcare system.2
Bottom LineCapitation payments are payments made to health care providers for providing services to patients. These payments are fixed and generally paid monthly (based on yearly contracts—i.e. capitation contracts).
This system helps doctors reduce bookkeeping, accounting, and other operating costs. Capitation also benefits the HMO or IPA by ensuring that providers don’t undertake more services than necessary. The idea is that it reduces the potential for excessive billing.
SPONSORED
Trade smarter with TradingView and Economic Calendar
Become a smarter trader with eToro’s advanced trading tools: be ready for every market movement, from earnings reports to dividend payments, and get the best out of our technical analysis skills with the power of TradingView charts — all easily accessible on the eToro trading platform. Join eToro today.